Toxicological Profile of Amanita Virosa – a Narrative Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mushrooms Russia and History
MUSHROOMS RUSSIA AND HISTORY BY VALENTINA PAVLOVNA WASSON AND R.GORDON WASSON VOLUME I PANTHEON BOOKS • NEW YORK COPYRIGHT © 1957 BY R. GORDON WASSON MANUFACTURED IN ITALY FOR THE AUTHORS AND PANTHEON BOOKS INC. 333, SIXTH AVENUE, NEW YORK 14, N. Y. www.NewAlexandria.org/ archive CONTENTS LIST OF PLATES VII LIST OF ILLUSTRATIONS IN THE TEXT XIII PREFACE XVII VOLUME I I. MUSHROOMS AND THE RUSSIANS 3 II. MUSHROOMS AND THE ENGLISH 19 III. MUSHROOMS AND HISTORY 37 IV. MUSHROOMS FOR MURDERERS 47 V. THE RIDDLE OF THE TOAD AND OTHER SECRETS MUSHROOMIC 65 1. The Venomous Toad 66 2. Basques and Slovaks 77 3. The Cripple, the Toad, and the Devil's Bread 80 4. The 'Pogge Cluster 92 5. Puff balls, Filth, and Vermin 97 6. The Sponge Cluster 105 7. Punk, Fire, and Love 112 8. The Gourd Cluster 127 9. From 'Panggo' to 'Pupik' 138 10. Mucus, Mushrooms, and Love 145 11. The Secrets of the Truffle 166 12. 'Gripau' and 'Crib' 185 13. The Flies in the Amanita 190 v CONTENTS VOLUME II V. THE RIDDLE OF THE TOAD AND OTHER SECRETS MUSHROOMIC (CONTINUED) 14. Teo-Nandcatl: the Sacred Mushrooms of the Nahua 215 15. Teo-Nandcatl: the Mushroom Agape 287 16. The Divine Mushroom: Archeological Clues in the Valley of Mexico 322 17. 'Gama no Koshikake and 'Hegba Mboddo' 330 18. The Anatomy of Mycophobia 335 19. Mushrooms in Art 351 20. Unscientific Nomenclature 364 Vale 374 BIBLIOGRAPHICAL NOTES AND ACKNOWLEDGEMENTS 381 APPENDIX I: Mushrooms in Tolstoy's 'Anna Karenina 391 APPENDIX II: Aksakov's 'Remarks and Observations of a Mushroom Hunter' 394 APPENDIX III: Leuba's 'Hymn to the Morel' 400 APPENDIX IV: Hallucinogenic Mushrooms: Early Mexican Sources 404 INDEX OF FUNGAL METAPHORS AND SEMANTIC ASSOCIATIONS 411 INDEX OF MUSHROOM NAMES 414 INDEX OF PERSONS AND PLACES 421 VI LIST OF PLATES VOLUME I JEAN-HENRI FABRE. -

Four Patients with Amanita Phalloides Poisoning CASE SERIE
CASE SERIE 353 Four patients with Amanita Phalloides poisoning S. Vanooteghem1, J. Arts2, S. Decock2, P. Pieraerts3, W. Meersseman4, C. Verslype1, Ph. Van Hootegem2 (1) Department of hepatology, UZ Leuven ; (2) Department of gastroenterology, AZ St-Lucas, Brugge ; (3) General Practitioner, Zedelgem ; (4) Department of internal medicine, UZ Leuven. Abstract because they developed stage 2 hepatic encephalopathy. With maximal supportive therapy, all patients gradually Mushroom poisoning by Amanita phalloides is a rare but poten- improved from day 3 and recovered without the need for tially fatal disease. The initial symptoms of nausea, vomiting, ab- dominal pain and diarrhea, which are typical for the intoxication, liver transplantation. They were discharged from the can be interpreted as a common gastro-enteritis. The intoxication hospital between 6 to 10 days after admission. can progress to acute liver and renal failure and eventually death. Recognizing the clinical syndrome is extremely important. In this case report, 4 patients with amatoxin intoxication who showed the Discussion typical clinical syndrome are described. The current therapy of amatoxin intoxication is based on small case series, and no ran- Among mushroom intoxications, amatoxin intoxica- domised controlled trials are available. The therapy of amatoxin intoxication consists of supportive care and medical therapy with tion accounts for 90% of all fatalities. Amatoxin poison- silibinin and N-acetylcysteine. Patients who develop acute liver fail- ing is caused by mushroom species belonging to the gen- ure should be considered for liver transplantation. (Acta gastro- era Amanita, Galerina and Lepiota. Amanita phalloides, enterol. belg., 2014, 77, 353-356). commonly known as the “death cap”, causes the majority Key words : amanita phalloides, mushroom poisoning, acute liver of fatal cases. -

Thesis Is Presented for the Degree of Doctor of Philosophy of Curtin University of Technology
School of Biomedical Sciences Analysis of Candidate Genes within the 3p14-p22 Region of the Human Genome for Association with Bone Mineral Density Phenotypes Benjamin H Mullin This thesis is presented for the Degree of Doctor of Philosophy of Curtin University of Technology February 2011 To the best of my knowledge and belief this thesis contains no material previously published by any other person except where due acknowledgment has been made. This thesis contains no material which has been accepted for the award of any other degree or diploma in any university. Preface The experimental work contained within this thesis was performed in the Department of Endocrinology & Diabetes at Sir Charles Gairdner Hospital under the supervision of Doctor Cyril Mamotte, Associate Professor Scott Wilson, and Professor Richard Prince. All experimental work in this thesis was performed by myself unless otherwise stated. Benjamin H. Mullin, B.Sc. Publications arising from this thesis Mullin, B. H., Prince, R. L., Dick, I. M., Hart, D. J., Spector, T. D., Dudbridge, F. & Wilson, S. G. 2008. Identification of a role for the ARHGEF3 gene in postmenopausal osteoporosis. American Journal of Human Genetics , 82 , 1262-9. Mullin, B. H., Prince, R. L., Mamotte, C., Spector, T. D., Hart, D. J., Dudbridge, F. & Wilson, S. G. 2009. Further genetic evidence suggesting a role for the RhoGTPase-RhoGEF pathway in osteoporosis. Bone , 45 , 387-91. Research grants received during completion of this thesis Wilson, S. G., Prince, R. L., Mamotte C., Mullin B. H. 2008. Influence of the ARHGEF3 gene on bone phenotypes. Arthritis Australia Project Grant ($14,500). -

Bur¯Aq Depicted As Amanita Muscaria in a 15Th Century Timurid-Illuminated Manuscript?
ORIGINAL ARTICLE Journal of Psychedelic Studies 3(2), pp. 133–141 (2019) DOI: 10.1556/2054.2019.023 First published online September 24, 2019 Bur¯aq depicted as Amanita muscaria in a 15th century Timurid-illuminated manuscript? ALAN PIPER* Independent Scholar, Newham, London, UK (Received: May 8, 2019; accepted: August 2, 2019) A series of illustrations in a 15th century Timurid manuscript record the mi’raj, the ascent through the seven heavens by Mohammed, the Prophet of Islam. Several of the illustrations depict Bur¯aq, the fabulous creature by means of which Mohammed achieves his ascent, with distinctive features of the Amanita muscaria mushroom. A. muscaria or “fly agaric” is a psychoactive mushroom used by Siberian shamans to enter the spirit world for the purposes of conversing with spirits or diagnosing and curing disease. Using an interdisciplinary approach, the author explores the routes by which Bur¯aq could have come to be depicted in this manuscript with the characteristics of a psychoactive fungus, when any suggestion that the Prophet might have had recourse to a drug to accomplish his spirit journey would be anathema to orthodox Islam. There is no suggestion that Mohammad’s night journey (isra) or ascent (mi’raj) was accomplished under the influence of a psychoactive mushroom or plant. Keywords: Mi’raj, Timurid, Central Asia, shamanism, Siberia, Amanita muscaria CULTURAL CONTEXT Bur¯aq depicted as Amanita muscaria in the mi’raj manscript The mi’raj manuscript In the Muslim tradition, the mi’raj was preceded by the isra or “Night Journey” during which Mohammed traveled An illustrated manuscript depicting, in a series of miniatures, overnight from Mecca to Jerusalem by means of a fabulous thesuccessivestagesofthemi’raj, the miraculous ascent of beast called Bur¯aq. -
Field Guide to Common Macrofungi in Eastern Forests and Their Ecosystem Functions
United States Department of Field Guide to Agriculture Common Macrofungi Forest Service in Eastern Forests Northern Research Station and Their Ecosystem General Technical Report NRS-79 Functions Michael E. Ostry Neil A. Anderson Joseph G. O’Brien Cover Photos Front: Morel, Morchella esculenta. Photo by Neil A. Anderson, University of Minnesota. Back: Bear’s Head Tooth, Hericium coralloides. Photo by Michael E. Ostry, U.S. Forest Service. The Authors MICHAEL E. OSTRY, research plant pathologist, U.S. Forest Service, Northern Research Station, St. Paul, MN NEIL A. ANDERSON, professor emeritus, University of Minnesota, Department of Plant Pathology, St. Paul, MN JOSEPH G. O’BRIEN, plant pathologist, U.S. Forest Service, Forest Health Protection, St. Paul, MN Manuscript received for publication 23 April 2010 Published by: For additional copies: U.S. FOREST SERVICE U.S. Forest Service 11 CAMPUS BLVD SUITE 200 Publications Distribution NEWTOWN SQUARE PA 19073 359 Main Road Delaware, OH 43015-8640 April 2011 Fax: (740)368-0152 Visit our homepage at: http://www.nrs.fs.fed.us/ CONTENTS Introduction: About this Guide 1 Mushroom Basics 2 Aspen-Birch Ecosystem Mycorrhizal On the ground associated with tree roots Fly Agaric Amanita muscaria 8 Destroying Angel Amanita virosa, A. verna, A. bisporigera 9 The Omnipresent Laccaria Laccaria bicolor 10 Aspen Bolete Leccinum aurantiacum, L. insigne 11 Birch Bolete Leccinum scabrum 12 Saprophytic Litter and Wood Decay On wood Oyster Mushroom Pleurotus populinus (P. ostreatus) 13 Artist’s Conk Ganoderma applanatum -

Meeting Key Synthetic Challenges in Amanitin Synthesis with a New Cytotoxic Analog: 50-Hydroxy- Cite This: Chem
Chemical Science View Article Online EDGE ARTICLE View Journal | View Issue Meeting key synthetic challenges in amanitin synthesis with a new cytotoxic analog: 50-hydroxy- Cite this: Chem. Sci., 2020, 11, 11927 0 † All publication charges for this article 6 -deoxy-amanitin have been paid for by the Royal Society of Chemistry Alla Pryyma, Kaveh Matinkhoo, Antonio A. W. L. Wong and David M. Perrin * Appreciating the need to access synthetic analogs of amanitin, here we report the synthesis of 50-hydroxy- Received 29th July 2020 60-deoxy-amanitin, a novel, rationally-designed bioactive analog and constitutional isomer of a-amanitin, Accepted 2nd October 2020 that is anticipated to be used as a payload for antibody drug conjugates. In completing this synthesis, we DOI: 10.1039/d0sc04150e meet the challenge of diastereoselective sulfoxidation by presenting two high-yielding and rsc.li/chemical-science diastereoselective sulfoxidation approaches to afford the more toxic (R)-sulfoxide. drug-tolerant cell subpopulations.7 Examples include ADCs for Creative Commons Attribution-NonCommercial 3.0 Unported Licence. Introduction targeting human epidermal growth factor receptor 2 and pros- 8 9 a-Amanitin, the deadliest of the amatoxins produced by the tate specic membrane antigen. With but a few exceptions, death-cap mushroom Amanita phalloides, is a potent, orally nearly all bioconjugates to a cytotoxic amanitin have emerged 1 a available inhibitor of RNA polymerase II (pol II) (Ki 10 nM), from naturally-sourced -amanitin. To date, conjugation that has been validated as a payload for targeted cancer handles used for a-amanitin-based bioconjugates include the d- 2a therapy.2 First described in 1907 3 and isolated in 1941,4 a- hydroxyl of (2S,3R,4R)-4,5-dihydroxyisoleucine (DHIle), the 10 0 amanitin is a compact bicyclic octapeptide that has been asparagine side chain, and the 6 -hydroxyl of the tryptathio- 11 indispensable for probing RNA pol II-catalysed transcription in nine staple. -
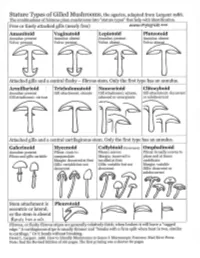
Agarics-Stature-Types.Pdf
Gilled Mushroom Genera of Chicago Region, by stature type and spore print color. Patrick Leacock – June 2016 Pale spores = white, buff, cream, pale green to Pinkish spores Brown spores = orange, Dark spores = dark olive, pale lilac, pale pink, yellow to pale = salmon, yellowish brown, rust purplish brown, orange pinkish brown brown, cinnamon, clay chocolate brown, Stature Type brown smoky, black Amanitoid Amanita [Agaricus] Vaginatoid Amanita Volvariella, [Agaricus, Coprinus+] Volvopluteus Lepiotoid Amanita, Lepiota+, Limacella Agaricus, Coprinus+ Pluteotoid [Amanita, Lepiota+] Limacella Pluteus, Bolbitius [Agaricus], Coprinus+ [Volvariella] Armillarioid [Amanita], Armillaria, Hygrophorus, Limacella, Agrocybe, Cortinarius, Coprinus+, Hypholoma, Neolentinus, Pleurotus, Tricholoma Cyclocybe, Gymnopilus Lacrymaria, Stropharia Hebeloma, Hemipholiota, Hemistropharia, Inocybe, Pholiota Tricholomatoid Clitocybe, Hygrophorus, Laccaria, Lactarius, Entoloma Cortinarius, Hebeloma, Lyophyllum, Megacollybia, Melanoleuca, Inocybe, Pholiota Russula, Tricholoma, Tricholomopsis Naucorioid Clitocybe, Hygrophorus, Hypsizygus, Laccaria, Entoloma Agrocybe, Cortinarius, Hypholoma Lactarius, Rhodocollybia, Rugosomyces, Hebeloma, Gymnopilus, Russula, Tricholoma Pholiota, Simocybe Clitocyboid Ampulloclitocybe, Armillaria, Cantharellus, Clitopilus Paxillus, [Pholiota], Clitocybe, Hygrophoropsis, Hygrophorus, Phylloporus, Tapinella Laccaria, Lactarius, Lactifluus, Lentinus, Leucopaxillus, Lyophyllum, Omphalotus, Panus, Russula Galerinoid Galerina, Pholiotina, Coprinus+, -

Peptide Chemistry up to Its Present State
Appendix In this Appendix biographical sketches are compiled of many scientists who have made notable contributions to the development of peptide chemistry up to its present state. We have tried to consider names mainly connected with important events during the earlier periods of peptide history, but could not include all authors mentioned in the text of this book. This is particularly true for the more recent decades when the number of peptide chemists and biologists increased to such an extent that their enumeration would have gone beyond the scope of this Appendix. 250 Appendix Plate 8. Emil Abderhalden (1877-1950), Photo Plate 9. S. Akabori Leopoldina, Halle J Plate 10. Ernst Bayer Plate 11. Karel Blaha (1926-1988) Appendix 251 Plate 12. Max Brenner Plate 13. Hans Brockmann (1903-1988) Plate 14. Victor Bruckner (1900- 1980) Plate 15. Pehr V. Edman (1916- 1977) 252 Appendix Plate 16. Lyman C. Craig (1906-1974) Plate 17. Vittorio Erspamer Plate 18. Joseph S. Fruton, Biochemist and Historian Appendix 253 Plate 19. Rolf Geiger (1923-1988) Plate 20. Wolfgang Konig Plate 21. Dorothy Hodgkins Plate. 22. Franz Hofmeister (1850-1922), (Fischer, biograph. Lexikon) 254 Appendix Plate 23. The picture shows the late Professor 1.E. Jorpes (r.j and Professor V. Mutt during their favorite pastime in the archipelago on the Baltic near Stockholm Plate 24. Ephraim Katchalski (Katzir) Plate 25. Abraham Patchornik Appendix 255 Plate 26. P.G. Katsoyannis Plate 27. George W. Kenner (1922-1978) Plate 28. Edger Lederer (1908- 1988) Plate 29. Hennann Leuchs (1879-1945) 256 Appendix Plate 30. Choh Hao Li (1913-1987) Plate 31. -

Forest Fungi in Ireland
FOREST FUNGI IN IRELAND PAUL DOWDING and LOUIS SMITH COFORD, National Council for Forest Research and Development Arena House Arena Road Sandyford Dublin 18 Ireland Tel: + 353 1 2130725 Fax: + 353 1 2130611 © COFORD 2008 First published in 2008 by COFORD, National Council for Forest Research and Development, Dublin, Ireland. All rights reserved. No part of this publication may be reproduced, or stored in a retrieval system or transmitted in any form or by any means, electronic, electrostatic, magnetic tape, mechanical, photocopying recording or otherwise, without prior permission in writing from COFORD. All photographs and illustrations are the copyright of the authors unless otherwise indicated. ISBN 1 902696 62 X Title: Forest fungi in Ireland. Authors: Paul Dowding and Louis Smith Citation: Dowding, P. and Smith, L. 2008. Forest fungi in Ireland. COFORD, Dublin. The views and opinions expressed in this publication belong to the authors alone and do not necessarily reflect those of COFORD. i CONTENTS Foreword..................................................................................................................v Réamhfhocal...........................................................................................................vi Preface ....................................................................................................................vii Réamhrá................................................................................................................viii Acknowledgements...............................................................................................ix -

The Ectomycorrhizal Fungus Amanita Phalloides Was Introduced and Is
Molecular Ecology (2009) doi: 10.1111/j.1365-294X.2008.04030.x TheBlackwell Publishing Ltd ectomycorrhizal fungus Amanita phalloides was introduced and is expanding its range on the west coast of North America ANNE PRINGLE,* RACHEL I. ADAMS,† HUGH B. CROSS* and THOMAS D. BRUNS‡ *Department of Organismic and Evolutionary Biology, Biological Laboratories, 16 Divinity Avenue, Harvard University, Cambridge, MA 02138, USA, †Department of Biological Sciences, Gilbert Hall, Stanford University, Stanford, CA 94305-5020, USA, ‡Department of Plant and Microbial Biology, 111 Koshland Hall, University of California, Berkeley, CA 94720, USA Abstract The deadly poisonous Amanita phalloides is common along the west coast of North America. Death cap mushrooms are especially abundant in habitats around the San Francisco Bay, California, but the species grows as far south as Los Angeles County and north to Vancouver Island, Canada. At different times, various authors have considered the species as either native or introduced, and the question of whether A. phalloides is an invasive species remains unanswered. We developed four novel loci and used these in combination with the EF1α and IGS loci to explore the phylogeography of the species. The data provide strong evidence for a European origin of North American populations. Genetic diversity is generally greater in European vs. North American populations, suggestive of a genetic bottleneck; polymorphic sites of at least two loci are only polymorphic within Europe although the number of individuals sampled from Europe was half the number sampled from North America. Endemic alleles are not a feature of North American populations, although alleles unique to different parts of Europe were common and were discovered in Scandinavian, mainland French, and Corsican individuals. -

Toxic Fungi of Western North America
Toxic Fungi of Western North America by Thomas J. Duffy, MD Published by MykoWeb (www.mykoweb.com) March, 2008 (Web) August, 2008 (PDF) 2 Toxic Fungi of Western North America Copyright © 2008 by Thomas J. Duffy & Michael G. Wood Toxic Fungi of Western North America 3 Contents Introductory Material ........................................................................................... 7 Dedication ............................................................................................................... 7 Preface .................................................................................................................... 7 Acknowledgements ................................................................................................. 7 An Introduction to Mushrooms & Mushroom Poisoning .............................. 9 Introduction and collection of specimens .............................................................. 9 General overview of mushroom poisonings ......................................................... 10 Ecology and general anatomy of fungi ................................................................ 11 Description and habitat of Amanita phalloides and Amanita ocreata .............. 14 History of Amanita ocreata and Amanita phalloides in the West ..................... 18 The classical history of Amanita phalloides and related species ....................... 20 Mushroom poisoning case registry ...................................................................... 21 “Look-Alike” mushrooms ..................................................................................... -

Mushrooms on Stamps
Mushrooms On Stamps Paul J. Brach Scientific Name Edibility Page(s) Amanita gemmata Poisonous 3 Amanita inaurata Not Recommended 4-5 Amanita muscaria v. formosa Poisonous (hallucenogenic) 6 Amanita pantherina Deadly Poisonous 7 Amanita phalloides Deadly Poisonous 8 Amanita rubescens Not Recommended 9-11 Amanita virosa Deadly Poisonous 12-14 Aleuria aurantiaca Edible 15 Sarcocypha coccinea Edible 16 Phlogiotis helvelloides Edible 17 Leccinum aurantiacum Good Edible 18 Boletus parasiticus Not Recommended 19 For this presentation I chose the species for Cantharellus cibarius Choice Edible 20 their occurrence in our 5 county region Cantharellus cinnabarinus Choice Edible 21 Coprinus atramentarius Poisonous 22 surrounding Rochester, NY. My intent is to Coprinus comatus Choice Edible 23 show our stamp collecting audience that an Coprinus disseminatus Edible 24 Clavulinopsis fusiformis Edible 25 artist's rendition of a fungi species depicted Leotia viscosa Harmless 26 on a stamp could be used akin to a Langermannia gigantea Choice Edible 27 Lycoperdon perlatum Good Edible 28-29 guidebook for the study of mushrooms. Entoloma murraii Not Recommended 30 Most pages depict a photograph and related Morchella esculenta Choice Edible 31-32 Russula rosacea Not Recommended (bitter) 33 stamp of the species, along with an edibility Laetiporus sulphureus Choice Edible 34 icon. Enjoy… but just the edible ones! Polyporus squamosus Edible 35 Choice/Good Edible Harmless Not Recommended Poisonous Deadly Poisonous 2 3 4 5 6 7 8 Amanita rubescens (blusher) 9 10