Toronto Subway Air Quality Health Impact Assessment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Toronto Subway System, ON
Canadian Geotechnical Society Canadian Geotechnical Achievements 2017 Toronto Subway System Geotechnical Investigation and Design of Tunnels Geographical location Key References Wong, JW. 1981. Geotechnical/ Toronto, Ontario geological aspects of the Toronto subway system. Toronto Transit Commission. When it began or was completed Walters, DL, Main, A, Palmer, S, Construction began in 1949 and continues today. Westland, J, and Bihendi, H. 2011. Managing subsurface risk for Toronto- York Spadina Subway extension project. Why a Canadian geotechnical achievement? 2011 Pan-Am and CGS Geotechnical Conference. Construction of the Toronto Transit Commission (TTC) subway system, the first in Canada, began in 1949 and currently consists Photograph and Map of four subway lines. In total there are currently approximately 68 km of subway tracks and 69 stations. Over one million trips are taken daily on the TTC during weekdays. The subway system has been expanded in several stages, from 1954, when the first line (the Yonge Line) was opened, to 2002, when the most recently completed line (the Sheppard Line) was opened. Currently the Toronto-York Spadina Subway Extension is under construction. The subway tunnels have been constructed using a number of different technologies over the years including: open cut excavation, open/closed shield tunneling under ambient air pressure and compressed air, hand mining and earth pressurized tunnel boring machines. The subway tunnels range in design from reinforced concrete box structures to approximately 6 m diameter precast concrete segmental liners or cast iron segmental liners. Looking east inside newly constructed TTC subway The tunnels have been advanced through various geological tunnel, 1968. (City of Toronto Archives) formations: from hard glacial tills to saturated alluvial sands and silts, and from glaciolacustrine clays to shale bedrock. -

Rapid Transit in Toronto Levyrapidtransit.Ca TABLE of CONTENTS
The Neptis Foundation has collaborated with Edward J. Levy to publish this history of rapid transit proposals for the City of Toronto. Given Neptis’s focus on regional issues, we have supported Levy’s work because it demon- strates clearly that regional rapid transit cannot function eff ectively without a well-designed network at the core of the region. Toronto does not yet have such a network, as you will discover through the maps and historical photographs in this interactive web-book. We hope the material will contribute to ongoing debates on the need to create such a network. This web-book would not been produced without the vital eff orts of Philippa Campsie and Brent Gilliard, who have worked with Mr. Levy over two years to organize, edit, and present the volumes of text and illustrations. 1 Rapid Transit in Toronto levyrapidtransit.ca TABLE OF CONTENTS 6 INTRODUCTION 7 About this Book 9 Edward J. Levy 11 A Note from the Neptis Foundation 13 Author’s Note 16 Author’s Guiding Principle: The Need for a Network 18 Executive Summary 24 PART ONE: EARLY PLANNING FOR RAPID TRANSIT 1909 – 1945 CHAPTER 1: THE BEGINNING OF RAPID TRANSIT PLANNING IN TORONTO 25 1.0 Summary 26 1.1 The Story Begins 29 1.2 The First Subway Proposal 32 1.3 The Jacobs & Davies Report: Prescient but Premature 34 1.4 Putting the Proposal in Context CHAPTER 2: “The Rapid Transit System of the Future” and a Look Ahead, 1911 – 1913 36 2.0 Summary 37 2.1 The Evolving Vision, 1911 40 2.2 The Arnold Report: The Subway Alternative, 1912 44 2.3 Crossing the Valley CHAPTER 3: R.C. -
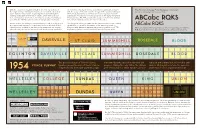
TTC Typography History
With the exception of Eglinton Station, 11 of the 12 stations of The intention of using Helvetica and Univers is unknown, however The Toronto Subway Font (Designer Unknown) the original Yonge Subway line have been renovated extensively. with the usage of the latter on the design of the Spadina Subway in Based on Futura by Paul Renner (1928) Some stations retained the original typefaces but with tighter 1978, it may have been an internal decision to try and assimilate tracking and subtle differences in weight, while other stations subsequent renovations of existing stations in the aging Yonge and were renovated so poorly there no longer is a sense of simplicity University lines. The TTC avoided the usage of the Toronto Subway seen with the 1954 designs in terms of typographical harmony. font on new subway stations for over two decades. ABCabc RQKS Queen Station, for example, used Helvetica (LT Std 75 Bold) in such The Sheppard Subway in 2002 saw the return of the Toronto Subway an irresponsible manner; it is repulsively inconsistent with all the typeface as it is used for the names of the stations posted on ABCabc RQKS other stations, and due to the renovators preserving the original platfrom level. Helvetica became the primary typeface for all TTC There are subtle differences between the two typefaces, notably the glass tile trim, the font weight itself looks botched and unsuitable. wayfinding signages and informational material system-wide. R, Q, K, and S; most have different terminals, spines, and junctions. ST CLAIR SUMMERHILL BLOOR DANGER DA N GER Danger DO NOT ENTER Do Not Enter Do Not Enter DAVISVILLE ST CL AIR SUMMERHILL ROSEDALE BLOOR EGLINTON DAVISVILLE ST CLAIR SUMMERHILL ROSEDALE BLOOR EGLINTON DAVISVILLE ST CLAIR SUMMERHILL ROSEDALE BLOOR The specially-designed Toronto Subway that embodied the spirit of modernism and replaced with a brutal mix of Helvetica and YONGE SUBWAY typeface graced the walls of the 12 stations, progress. -

Relief Line Update
Relief Line Update Mathieu Goetzke, Vice-President, Planning David Phalp, Manager, Rapid Transit Planning FEBRUARY 7, 2019 EXECUTIVE SUMMARY • The Relief Line South alignment identified by the City of Toronto as preferred, has a Benefit Cost Ratio (BCR) above 1.0, demonstrating the project’s value; however, since it is close to 1.0, it is highly sensitive to costs, so more detailed design work and procurement method choice will be of importance to maintain or improve this initial BCR. • Forecasts suggest that Relief Line South will attract ridership to unequivocally justify subway-level service; transit-oriented development opportunities can further boost ridership. • Transit network forecasts show that Relief Line South needs to be in operation before the Yonge North Subway Extension. Relief Line North provides further crowding relief for Line 1. RELIEF LINE UPDATE 2 SUBWAY EXPANSION - PROJECT STATUS Both Relief Line North and South and the Yonge North Subway Extension are priority projects included in the 2041 Regional Transportation Plan. RELIEF LINE UPDATE 3 RELIEF LINE SOUTH: Initial Business Case Alignments Evaluated • Metrolinx is developing an Initial Business Case on Relief Line South, evaluating six alignments according to the Metrolinx Business Case Guidance and the Auditor General’s 2018 recommendations • Toronto City Council approved the advancement of alignment “A” (Pape- Queen via Carlaw & Eastern) • Statement of Completion of the Transit Project Assessment Process (TPAP) received October 24, 2018. RELIEF LINE UPDATE 4 RELIEF -

Applying Life Cycle Assessment to Analyze the Environmental Sustainability of Public Transit Modes for the City of Toronto
Applying life cycle assessment to analyze the environmental sustainability of public transit modes for the City of Toronto by Ashton Ruby Taylor A thesis submitted to the Department of Geography & Planning in conformity with the requirements for the Degree of Master of Science Queen’s University Kingston, Ontario, Canada September, 2016 Copyright © Ashton Ruby Taylor, 2016 Abstract One challenge related to transit planning is selecting the appropriate mode: bus, light rail transit (LRT), regional express rail (RER), or subway. This project uses data from life cycle assessment to develop a tool to measure energy requirements for different modes of transit, on a per passenger-kilometer basis. For each of the four transit modes listed, a range of energy requirements associated with different vehicle models and manufacturers was developed. The tool demonstrated that there are distinct ranges where specific transit modes are the best choice. Diesel buses are the clear best choice from 7-51 passengers, LRTs make the most sense from 201-427 passengers, and subways are the best choice above 918 passengers. There are a number of other passenger loading ranges where more than one transit mode makes sense; in particular, LRT and RER represent very energy-efficient options for ridership ranging from 200 to 900 passengers. The tool developed in the thesis was used to analyze the Bloor-Danforth subway line in Toronto using estimated ridership for weekday morning peak hours. It was found that ridership across the line is for the most part actually insufficient to justify subways over LRTs or RER. This suggests that extensions to the existing Bloor-Danforth line should consider LRT options, which could service the passenger loads at the ends of the line with far greater energy efficiency. -

Ontario Line Early Works - Presentation by Metrolinx
REPORT FOR ACTION Ontario Line Early Works - Presentation by Metrolinx Date: February 4, 2021 To: The Board of Governors of Exhibition Place From: Don Boyle, Chief Executive Officer Wards: All Wards SUMMARY Announced by the Province of Ontario in 2019, the proposed Ontario Line is one of four priority transit projects Metrolinx is leading for the Greater Toronto Area (GTA). The line will be the largest single expansion in Toronto’s subway history, helping to ease congestion on existing transit lines throughout the city, and bring transit to underserviced neighbourhoods. The Ontario Line will bring nearly 16 kilometres of much-needed subway service to Toronto to make it faster and easier for hundreds of thousands of people to get where they need to be each day. The line will stretch across the city, from the Ontario Science Centre in the northeast to Exhibition Place in the southwest. Current plans for the Ontario Line include 15 stations including 6 interchange stations, and over 40 new connections to GO train lines and existing subway, streetcar, and bus lines. Staff form Metrolinx will be attending the Board meeting of February 19, 2021 to do a power point presentation on the design and progress of the Ontario Line development to date for the benefit of the Board Members. RECOMMENDATIONS The Chief Executive Officer recommends that: 1.The Board receive this report for information. Ontario Early Line Works - Presentation by Metrolinx Page 1 of 3 FINANCIAL IMPACT There are no financial implications associated with this report. DECISION HISTORY The Exhibition Place 2017-2019 Strategic Plan has a focus on Public Space and Infrastructure, which includes an objective to identify the linkages to future public transit and road networks. -
Canada Rail Opportunities Scoping Report Preface
01 Canada Rail Opportunities Canada Rail Opportunities Scoping Report Preface Acknowledgements Photo and image credits The authors would like to thank the Agence Métropolitaine de Transport following organisations for their help and British Columbia Ministry of Transportation support in the creation of this publication: and Infrastructure Agence Métropolitaine de Transport BC Transit Alberta Ministry of Transport Calgary Transit Alberta High Speed Rail City of Brampton ARUP City of Hamilton Balfour Beatty City of Mississauga Bombardier City of Ottawa Calgary Transit Edmonton Transit Canadian National Railway Helen Hemmingsen, UKTI Toronto Canadian Urban Transit Association Metrolinx Edmonton Transit OC Transpo GO Transit Sasha Musij, UKTI Calgary Metrolinx Société de Transport de Montréal RailTerm TransLink SNC Lavalin Toronto Transit Commission Toronto Transit Commission Wikimedia Commons Wikipedia Front cover image: SkyTrain in Richmond, Vancouver Canada Rail Opportunities Contents Preface Foreword 09 About UK Trade & Investment 10 High Value Opportunities Programme 11 Executive Summary 12 1.0 Introduction 14 2.0 Background on Canada 15 2.1 Macro Economic Review 16 2.2 Public-Private Partnerships 18 3.0 Overview of the Canadian Rail Sector 20 4.0 Review of Urban Transit Operations and Opportunities by Province 21 4.1 Summary Table of Existing Urban Transit Rail Infrastructure and Operations 22 4.2 Summary Table of Key Project Opportunities 24 4.3 Ontario 26 4.4 Québec 33 4.5 Alberta 37 4.6 British Columbia 41 5.0 In-Market suppliers 45 5.1 Contractors 45 5.2 Systems and Rolling Stock 48 5.3 Consultants 49 6.0 Concluding Remarks 51 7.0 Annexes 52 7.1 Doing Business in Canada 52 7.2 Abbreviations 53 7.3 Bibliography 54 7.4 List of Reference Websites 56 7.5 How can UKTI Help UK Organisations Succeed in Canada 58 Contact UKTI 59 04 Canada Rail Opportunities About the Authors David Bill Helen Hemmingsen David is the International Helen Hemmingsen is a Trade Officer Development Director for the UK with the British Consulate General Railway Industry Association (RIA). -

Conservation and the Crosstown: Exploring the Intersection of Retail Heritage and Transportation Infrastructure in Toronto
CONSERVATION AND THE CROSSTOWN: EXPLORING THE INTERSECTION OF RETAIL HERITAGE AND TRANSPORTATION INFRASTRUCTURE IN TORONTO By: Sophia Sousa Supervised By: Laura E. Taylor A Major Paper submitted to the Faculty of Environmental Studies in partial fulfillment of the requirements for the degree of Master in Environmental Studies York University, Toronto, Ontario, Canada November 29, 2018 CONTENTS CONTENTS LIST OF FIGURES .............................................................................................................................................. i ACKNOWLEDGEMENTS .................................................................................................................................. ii ABSTRACT ..................................................................................................................................................... iii FOREWORD ................................................................................................................................................... iv INTERSECTING THE PLAN OF STUDY .......................................................................................................... v INTRODUCTION .............................................................................................................................................. 1 METHODOLOGY ........................................................................................................................................ 6 CHAPTER 1 ................................................................................................................................................... -

Scarborough Subway Extension Preliminary Design Business Case February 2020
Scarborough Subway Extension Preliminary Design Business Case February 2020 Scarborough Subway Extension Preliminary Design Business Case February 2020 Contents Executive Summary 7 Scope 7 Method of Analysis 7 Findings 8 Recommendation 9 1 Introduction 10 Preliminary Design Business Case Scope and Objectives 11 Background 11 Business Case Overview 13 2 Problem Statement 15 Introduction 16 Case for Change 16 Business as Usual 16 Strategic Value 18 Strategic Outcomes 19 Strong Connections: 19 Complete Travel Experiences: 19 Sustainable and Healthy Communities: 19 Strategic Objectives 19 3 Investment Options 21 Introduction 22 iv Options Development 22 Summary of Assumptions Used in this Business Case for Analysis and Travel Demand Modelling 25 4 Strategic Case 26 Introduction 27 BENEFIT 1: Bring rapid transit closer to Scarborough residents 28 BENEFIT 2: Increase access to existing economic opportunities and support the important employment centre at Scarborough Centre 29 BENEFIT 3: Support planned development in Scarborough 33 Outcome 2: COMPLETE TRAVEL EXPERIENCES 35 BENEFIT 4: Improve Travel Time and Reliability 36 BENEFIT 5: Build an Integrated Transportation Network 40 Outcome 3: SUSTAINABLE AND HEALTHY COMMUNITIES 43 BENEFIT 6: Move People with Less Energy and Pollution 44 BENEFIT 7: Improve Quality of Life and Public Health 45 Strategic Case Summary 46 5 Economic Case 48 Introduction and Assumptions 49 Costs 51 6 Financial Case 57 Introduction 58 Assumptions 58 Capital Costs 58 7 Deliverability and Operations Case 63 Introduction -
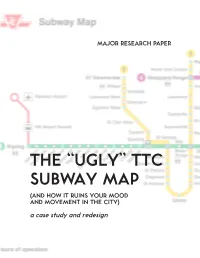
TTC SUBWAY MAP (AND HOW IT RUINS YOUR MOOD and MOVEMENT in the CITY) a Case Study and Redesign MPC MAJOR RESEARCH PAPER
MAJOR RESEARCH PAPER THE “UGLY” TTC SUBWAY MAP (AND HOW IT RUINS YOUR MOOD AND MOVEMENT IN THE CITY) a case study and redesign MPC MAJOR RESEARCH PAPER THE “UGLY” TTC SUBWAY MAP (AND HOW IT RUINS YOUR MOOD AND MOVEMENT IN THE CITY) A CASE STUDY AND REDESIGN JOANNA SIDA LIU Dr. Matthew Tiessen The Major Research Paper is submitted in partial fulfillment of the requirements for the degree of Master of Professional Communication Ryerson University Toronto, Ontario, Canada September 1, 2016 i. AUTHOR’S DECLARATION I hereby declare that I am the sole author of this Major Research Paper and the accompanying Research Poster. This is a true copy of the MRP and the research poster, including any required final revisions, as accepted by my examiners. I authorize Ryerson University to lend this major research paper and/or poster to other institutions or individuals for the purpose of scholarly research. I further authorize Ryerson University to reproduce this MRP and/or poster by photocopying or by other means, in total or in part, at the request of other institutions or individuals for the purpose of scholarly research. I understand that my MRP and/or my MRP research poster may be made electronically available to the public. 3 ii. ABSTRACT The TTC subway was built in 1949 to resolve the traffic issues of that era, issues that have only since intensified. At the time, any underground transportation system was an impressive accomplishment in design, engineering, construction, and city planning. Today, those same accomplishments—left to stagnate, age, and become overburdened—have become outdated and—measured against contemporary designs—sometimes even ridiculed. -

Facts and Figures Trains on Theyonge/University/Spadina
3. SIGNALLING 3.1 INTRODUCTION Present Operation - Facts and Figures Trains on theYonge/University/Spadina (Y/U/S) route of the TTC subway network are presently scheduled at a constant time interval (headway) of 130 seconds apart during normal peak service periods. A short turn operation is instituted on the Spadina portion of the route, wherein alternate trains turnback at St. Glair West Station rather than proceeding to Wilson Station, resulting in scheduled headways between St. Clair West and Wilson of 260 seconds. Scheduled operation at 130 second headways corresponds to a service level of approximately 28 trains per hour. This in turn corresponds to a passenger carrying capacity of approximately 34,000 passengers per hour per direction (pphpd), based on the Commission's Vehicle Loading Standard of 1200 passengers per subway train. 1 A total of 45 trains are operated in service on the Y/U/S route during peak periods. Of this total, 20 trains are involved in the short turn operation (Finch Station to St. Clair West Station), while the remaining 25 trains are operated over the entire route, Finch Station to Wilson Station. The present Y/U/S fleet is composed of a mixture of three different types of rolling stock. The original red subway cars acquired in the 1950's for the first segment of the Toronto subway (Union to Eglinton) are still operated on the Y/U/S route. These cars, manufactured by the Gloucester Railway Carriage and Wagon Co. Ltd. (G-cars), have performed well for over 30 years, but are heavy and slow by modern standards, and are at the end of their design life. -

Toronto-Ontario Transit Update
EX9.1 Part 2 Appendix A Advertising Campaign • Advertisements • Notice of Phase 1 PICs • Postcards Advertisements The future of the transit system is on a need-to-know basis. And you need to know. Have your say at Toronto.ca/TransitReview Transit expansion is exciting news. Transit maintenance? Not so much. Yet both are equally important. Learn why at Toronto.ca/TransitReview Notice of Phase 1 PICs The City of Toronto holds public consultations as one way to engage residents in the life of their city. We invite you to get involved. Transit Review - Public Information Meeting Maintaining and expanding Toronto’s transit system The City is holding public meetings where you can learn more about the review on transit responsibilities between the City and Province. Open house, followed by presentation. Thurs. June 13, 6:30 to 8:30 p.m. Father Serra Separate School, 111 Sun Row Dr., Etobicoke Thurs. June 20, 6:30 to 8:30 p.m. North York Memorial Community Hall, 5110 Yonge St., North York Sat. June 22, 10:30 a.m. to 12:30 p.m. Scarborough Civic Centre, 150 Borough Dr., Scarborough Thurs. June 27, 6:30 to 8:30 p.m. City Hall, Council Chamber, 100 Queen St. W., Toronto Public transit services in Toronto are integral to the city and region’s vitality. Changes are being made by the Province to the way transit is planned, designed, constructed, and funded in the city. Come learn more and have your say about the changes. If you are unable to attend in person, please note that we are live streaming the June 27 meeting at youtube.com/thecityoftoronto Tel: 416-398-5395 Email: [email protected] Visit: toronto.ca/transitreview Postcards Changes are being made to how transit is planned, designed, funded and delivered in Toronto.