Trimbow, INN-Beclometasone Dipropionate, Formoterol Fumarate
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
TAYSIDE PRESCRIBER Issue No
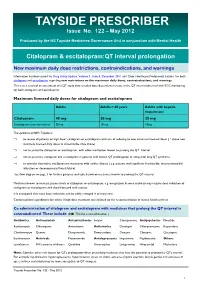
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -

PRODUCT MONOGRAPH ELAVIL® Amitriptyline Hydrochloride Tablets
PRODUCT MONOGRAPH ELAVIL® amitriptyline hydrochloride tablets USP 10, 25, 50 and 75 mg Antidepressant AA PHARMA INC. DATE OF PREPARATION: 1165 Creditstone Road Unit #1 August 29, 2018 Vaughan, ON L4K 4N7 Control No.: 217626 1 PRODUCT MONOGRAPH ELAVIL® amitriptyline hydrochloride tablets USP 10, 25, 50, 75 mg THERAPEUTIC CLASSIFICATION Antidepressant ACTIONS AND CLINICAL PHARMACOLOGY Amitriptyline hydrochloride is a tricyclic antidepressant with sedative properties. Its mechanism of action in man is not known. Amitriptyline inhibits the membrane pump mechanism responsible for the re-uptake of transmitter amines, such as norepinephrine and serotonin, thereby increasing their concentration at the synaptic clefts of the brain. Amitriptyline has pronounced anticholinergic properties and produces EKG changes and quinidine-like effects on the heart (See ADVERSE REACTIONS). It also lowers the convulsive threshold and causes alterations in EEG and sleep patterns. Orally administered amitriptyline is readily absorbed and rapidly metabolized. Steady-state plasma concentrations vary widely and this variation may be genetically determined. Amitriptyline is primarily excreted in the urine, mostly in the form of metabolites, with some excretion also occurring in the feces. INDICATIONS AND CLINICAL USE ELAVIL® (amitriptyline hydrochloride) is indicated in the drug management of depressive illness. ELAVIL® may be used in depressive illness of psychotic or endogenous nature and in selected patients with neurotic depression. Endogenous depression is more likely to be alleviated than are other depressive states. ELAVIL® ®, because of its sedative action, is also of value in alleviating the anxiety component of depression. As with other tricyclic antidepressants, ELAVIL® may precipitate hypomanic episodes in patients with bipolar depression. These drugs are not indicated in mild depressive states and depressive reactions. -

COPD Agents Review – October 2020 Page 2 | Proprietary Information
COPD Agents Therapeutic Class Review (TCR) October 1, 2020 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. October 2020 -

PERPHENAZINE and AMITRIPTYLINE HYDROCHLORIDE- Perphenazine and Amitriptyline Hydrochloride Tablet, Film Coated Mylan Pharmaceuticals Inc
PERPHENAZINE AND AMITRIPTYLINE HYDROCHLORIDE- perphenazine and amitriptyline hydrochloride tablet, film coated Mylan Pharmaceuticals Inc. ---------- WARNING Increased Mortality in Elderly Patients with Dementia-Related Psychosis Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug- treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. Perphenazine and amitriptyline hydrochloride is not approved for the treatment of patients with dementia- related psychosis (see WARNINGS). Suicidality and Antidepressant Drugs Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of perphenazine and amitriptyline or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. -

Nuedexta) National Drug Monograph May 2013 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives
Dextromethorphan/ Quinidine Monograph Dextromethorphan Hydrobromide and Quinidine Sulfate (Nuedexta) National Drug Monograph May 2013 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a comprehensive drug review for making formulary decisions. These documents will be updated when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. Executive Summary: Current therapy for pseudobulbar affect (PBA) typically utilizes non-pharmacologic coping strategies such as relaxation and distraction techniques. The off-label use of selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs) and dopaminergic agents has found limited success in treating PBA exacerbations. Dextromethorphan/quinidine (Nuedexta) is a combination of two existing generic formulary options; however quinidine is not available in an appropriate strength or in a liquid formulation (200mg, 300mg capsules only). Low dose quinidine inhibits the rapid metabolism of dextromethorphan, therefore increasing the bioavailability of dextromethorphan, resulting in effective plasma levels. In a double-blind, placebo-controlled study, the combination of dextromethorphan (20 or 30 mg) and low dose quinidine (10 mg) [STAR trial] significantly reduced the frequency of pseudobulbar affect episodes vs. placebo over the course of 12 weeks of treatment (p < 0.0001). Patients in the dextromethorphan/quinidine 20 mg/10 mg group reported a mean weekly episode reduction of 82% from baseline vs. a reduction of 47% in the placebo group (p = 0.001). Mean Center for Neurological Study-Lability Scale (CNS-LS) scores decreased by 8.2 points for both dextromethorphan/quinidine dosage groups vs. -

ANTIDEPRESSANTS in USE in CLINICAL PRACTICE Mark Agius1 & Hannah Bonnici2 1Clare College, University of Cambridge, Cambridge, UK 2Hospital Pharmacy St
Psychiatria Danubina, 2017; Vol. 29, Suppl. 3, pp 667-671 Conference paper © Medicinska naklada - Zagreb, Croatia ANTIDEPRESSANTS IN USE IN CLINICAL PRACTICE Mark Agius1 & Hannah Bonnici2 1Clare College, University of Cambridge, Cambridge, UK 2Hospital Pharmacy St. James Hospital Malta, Malta SUMMARY The object of this paper, rather than producing new information, is to produce a useful vademecum for doctors prescribing antidepressants, with the information useful for their being prescribed. Antidepressants need to be seen as part of a package of treatment for the patient with depression which also includes psychological treatments and social interventions. Here the main Antidepressant groups, including the Selective Serotonin uptake inhibiters, the tricyclics and other classes are described, together with their mode of action, side effects, dosages. Usually antidepressants should be prescribed for six months to treat a patient with depression. The efficacy of anti-depressants is similar between classes, despite their different mechanisms of action. The choice is therefore based on the side-effects to be avoided. There is no one ideal drug capable of exerting its therapeutic effects without any adverse effects. Increasing knowledge of what exactly causes depression will enable researchers not only to create more effective antidepressants rationally but also to understand the limitations of existing drugs. Key words: antidepressants – depression - psychological therapies - social therapies * * * * * Introduction Monoamine oxidase (MAO) inhibitors í Non-selective Monoamine Oxidase Inhibitors Depression may be defined as a mood disorder that í Selective Monoamine Oxidase Type A inhibitors negatively and persistently affects the way a person feels, thinks and acts. Common signs include low mood, Atypical Anti-Depressants and other classes changes in appetite and sleep patterns and loss of inte- rest in activities that were once enjoyable. -
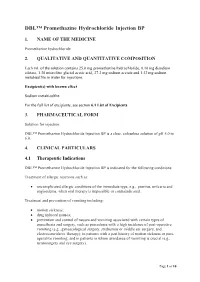
DBL™ Promethazine Hydrochloride Injection BP
DBL™ Promethazine Hydrochloride Injection BP 1. NAME OF THE MEDICINE Promethazine hydrochloride 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each mL of the solution contains 25.0 mg promethazine hydrochloride, 0.10 mg disodium edetate, 1.30 microlitre glacial acetic acid, 27.2 mg sodium acetate and 1.32 mg sodium metabisulfite in water for injections. Excipient(s) with known effect Sodium metabisulfite For the full list of excipients, see section 6.1 List of Excipients. 3. PHARMACEUTICAL FORM Solution for injection. DBL™ Promethazine Hydrochloride Injection BP is a clear, colourless solution of pH 5.0 to 6.0. 4. CLINICAL PARTICULARS 4.1 Therapeutic Indications DBL™ Promethazine Hydrochloride Injection BP is indicated for the following conditions: Treatment of allergic reactions such as: uncomplicated allergic conditions of the immediate type, e.g., pruritus, urticaria and angioedema, when oral therapy is impossible or contraindicated. Treatment and prevention of vomiting including: motion sickness; drug induced nausea; prevention and control of nausea and vomiting associated with certain types of anaesthesia and surgery, such as procedures with a high incidence of post-operative vomiting (e.g., gynaecological surgery, strabismus or middle ear surgery, and electroconvulsive therapy); in patients with a past history of motion sickness or post- operative vomiting; and in patients in whom avoidance of vomiting is crucial (e.g., neurosurgery and eye surgery). Page 1 of 10 Promethazine has sedative effects and it is also used in: pre-operative, post-operative and obstetric (during labour) sedation. 4.2 Dose and Method of Administration Dosage Allergic conditions Adults: 25 mg to 50 mg by deep intramuscular injection or slow intravenous injection; may be repeated within two hours if necessary. -

IEHP Dualchoice Cal Mediconnect Formulary Maintenance Drug List
IEHP DualChoice Cal MediConnect (Medicare-Medicaid Plan) Formulary Maintenance Drug List The following formulary medications may be approvable up to a three-month supply. Certain medications on this list may require prior approval from the plan based on existing criteria before being covered. For coverage information please see our formulary located on our website. BRAND GENERIC STREGTH DOSAGE FORM ABACAVIR ABACAVIR SULFATE 300 MG TABLET ABACAVIR ABACAVIR SULFATE 20 MG/ML SOLUTION TRIUMEQ ABACAVIR SULFATE/DOLUTEGRAVIR 600-50-300 TABLET SODIUM/LAMIVUDINE ABACAVIR-LAMIVUDINE ABACAVIR SULFATE/LAMIVUDINE 600-300MG TABLET ABACAVIR-LAMIVUDINE- ABACAVIR SULFATE/LAMIVUDINE/ZIDOVUDINE 150-300 MG TABLET ZIDOVUDINE TYMLOS ABALOPARATIDE 80MCG/DOSE PEN INJCTR ORENCIA ABATACEPT 125 MG/ML SYRINGE ORENCIA CLICKJECT ABATACEPT 125 MG/ML AUTO INJCT ORENCIA ABATACEPT 50MG/0.4ML SYRINGE ORENCIA ABATACEPT 87.5MG/0.7 SYRINGE VERZENIO ABEMACICLIB 50 MG TABLET VERZENIO ABEMACICLIB 100 MG TABLET VERZENIO ABEMACICLIB 150 MG TABLET VERZENIO ABEMACICLIB 200 MG TABLET ABIRATERONE ACETATE ABIRATERONE ACETATE 500 MG TABLET ABIRATERONE ACETATE ABIRATERONE ACETATE 250 MG TABLET YONSA ABIRATERONE ACETATE, SUBMICRONIZED 125 MG TABLET CALQUENCE ACALABRUTINIB 100 MG CAPSULE ACAMPROSATE CALCIUM ACAMPROSATE CALCIUM 333 MG TABLET DR ACARBOSE ACARBOSE 25 MG TABLET ACARBOSE ACARBOSE 50 MG TABLET ACARBOSE ACARBOSE 100 MG TABLET ACEBUTOLOL HCL ACEBUTOLOL HCL 200 MG CAPSULE ACEBUTOLOL HCL ACEBUTOLOL HCL 400 MG CAPSULE ACETAZOLAMIDE ER ACETAZOLAMIDE 500 MG CAPSULE ER ACETAZOLAMIDE -

Prothiaden 25Mg & 75Mg (Front) Size: 222 X 252Mm Colour: Black Date: 01-04-2014, 13-08-2014, 18-09-2014, 09-06-2015, 11-06-2015 Ammara Commercial Printers (Pvt.) Ltd
d te a Lactation trimester of pregnancy have also been reported (see o Dosulepin/metabolites are excreted in human milk. Breast- PREGNANCY AND LACTATION). C m For the information of Medical Profession feeding should be discontinued during treatment with Dosulepin. il Class effects F EFFECTS ON ABILITY TO DRIVE AND USE MACHINES Epidemiological studies, mainly conducted in patients 50 years of PROTHIADEN Initially, Dosulepin may impair alertness; therefore Dosulepin has age and older, show an increased risk of bone fractures in patients minor influence on the ability to drive and use machines. receiving SSRIs and TCAs. The mechanism leading to this risk is (Dosulepin Hydrochloride) unknown. ADVERSE REACTIONS The following adverse effects, although not necessarily all OVERDOSAGE reported with Dosulepin, have occurred with other tricyclic Symptoms: PRODUCT DESCRIPTION antidepressants. Deaths may occur from overdosage with this class of drugs. Dosulepin hydrochloride is a tricyclic antidepressant that has Multiple drug ingestion (including alcohol) is common in deliberate anxiolytic properties. The chemical name is 3-(6H-dibenzo(b,e)- Blood and lymphatic system disorders tricyclic antidepressant overdose. Onset of toxicity occurs within thiepin-11-ylidene) propyldimethylamine hydrochloride. Bone marrow depression, agranulocytosis 4-6 hours after tricyclic antidepressant overdose. Dosulepin hydrochloride is a white to faintly yellow crystalline Symptoms of overdose include dry mouth, excitement, ataxia, powder that is almost without odor. The compound is soluble in Immune system disorder drowsiness,unconsciousness, muscle twitching, convulsions, water, chloroform, and alcohol but is almost insoluble in ether. The Hypersensitivity reactions widely dilated pupils, hyperreflexia, sinus tachycardia, cardiac molecular weight is 331.9. arrhythmias, hypotension, hypothermia, depression of respiration, visual hallucinations, delirium, urinary retention, Endocrine disorders Inactive Ingredients paralytic ileus, and respiratory or metabolic alkalosis. -

Nuedexta, INN-Dextromethorphan/Quinidine
authorised longer no product Medicinal SUMMARY OF PRODUCT CHARACTERISTICS ANNEX I 1 1. NAME OF THE MEDICINAL PRODUCT NUEDEXTA 15 mg/9 mg hard capsules 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each capsule contains dextromethorphan hydrobromide monohydrate, equivalent to 15.41 mg dextromethorphan and quinidine sulfate dihydrate, equivalent to 8.69 mg quinidine. Excipient with known effect: Each hard capsule contains 119.1 mg of lactose (as monohydrate). For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Hard capsule Brick red gelatin capsule, size 1, with “DMQ / 20-10” printed in white inkauthorised on the capsule. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications longer NUEDEXTA is indicated for the symptomatic treatmentno of pseudobulbar affect (PBA) in adults (see section 4.4). Efficacy has only been studied in patients with underlying Amyotrophic Lateral Sclerosis or Multiple Sclerosis (see section 5.1). 4.2 Posology and method of administration product Posology The recommended starting dose is NUEDEXTA 15 mg/9 mg once daily. The recommended dose titration schedule is outlined below: Week 1 (day 1-7): The patientMedicinal should take one NUEDEXTA 15 mg/9 mg capsule once daily, in the morning, for the initial 7 days. Weeks 2-4 (day 8-28): The patient should take one NUEDEXTA 15 mg/9 mg capsule, two times per day, one in the morning and one in the evening, 12-hours apart, for 21 days. From Week 4 on: If the clinical response with NUEDEXTA 15 mg/9 mg is adequate, the dose taken in weeks 2-4 should be continued. -

West Essex CCG Anticholinergic Side-Effects and Prescribing Guidance
Anticholinergic side-effects and prescribing guidance . Anticholinergic (antimuscarinic) medications: associated with increased risks of impaired cognition and falls in patients over the age of 65 years. Recent research also points to a link to mortality increasing with the number and potency of anticholinergic agents prescribed. Anticholinergic Syndrome: is a state of confusion with characteristic features related to dysfunction of the autonomic parasympathetic (cholinergic) nervous system. Symptoms classified into systemic and CNS manifestations: o Systemic (peripheral) symptoms: Blurred vision, photophobia, non-reactive mydriasis, loss of accommodation response, flushed and dry skin, dry mouth, tachycardia, hypertension and fever. Gastrointestinal and urinary motility are frequently reduced o CNS symptoms: Delirium, agitation, disorientation, and visual hallucinations. Ataxia, choreoathetosis, myoclonus and seizures may also occur without peripheral symptoms. Medication Issues: several commonly prescribed medications that may not be thought of as anticholinergic have significant anticholinergic effects, which when taken with known anticholinergic medication can increase the risk of adverse effects. Many medication groups e.g. antihistamines, tricyclic antidepressants, drugs for asthma and COPD, cold preparations, hyoscine have varying degrees of anticholinergic activity and have the potential to cause Anticholinergic Syndrome . Clinicians should be aware of the risk for chronic anticholinergic toxicity and the fact that not all the symptoms may manifest in patients and if they do suffer some symptoms they could be wrongly attributed to another diagnosis Evidence . A study of patients over 65 found that 20% of participants who scored four or more had died by the end of the two year study period compared with 7% of patients with a score of zero. -

Current and Experimental Therapeutics of Ocd
114 CURRENT AND EXPERIMENTAL THERAPEUTICS OF OCD ERIC HOLLANDER STEFANO PALLANTI versely, other disorders may present with symptoms remi- niscent of OCD. For example, the ruminations of depres- UNIQUE ASPECTS OF OCD sion, intrusive thoughts, or delusions of psychotic disorders, PHARMACOTHERAPY and stereotyped behaviors of developmental disorders, may mimic OCD. Thus, comprehensive clinical evaluation and Obsessive-compulsive disorder (OCD) is a chronic disorder careful differential diagnosis are essential. with substantial impact on quality of life (1) that affects Psychiatric comorbidity is the rule rather than the excep- 2% to 3% of the US population (2,3). Previously believed tion in OCD. Up to two-thirds of all patients with OCD to be refractory to treatment, the symptoms of OCD are have lifetime comorbidities (3,4). These comorbid condi- substantially reduced with the use of medications having tions not only serve to cloud the diagnostic picture, but also potent effects on blocking the serotonin (5-HT) transporter. can influence the selection of optimal treatments. The response to serotonin reuptake inhibitors (SRIs) in The prevalence of obsessive-compulsive symptoms in OCD is somewhat unique compared to that in other mood schizophrenic patients has been estimated to range from and anxiety disorders, in that higher doses and a longer lag- 7.8% to 46.6% (5–7). A recent paper reported that in the time to therapeutic effect of SSRIs may be required, and a early phase of the disorder, 14% of schizophrenic patients lack of response to other antidepressant/antianxiety agents fulfilled criteria for a diagnosis of OCD (8). Atypical neuro- in OCD is evident.