COPD Agents Review – October 2020 Page 2 | Proprietary Information
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SCH 58261: a Potent and Selective Non-Xanthine A2A Adenosine Receptor Antagonist
22 DIRECTED DRUG DISCOVERY™ LIGAND-SETS™ for Assay Validation and High Throughput Screening Easy-to-use collections of pharmacologically-similar, small organic ligands Sigma-RBI LIGAND-SETS™ are a convenient and affordable way to screen a specific target with a collection of well- characterized, pharmacologically-active compounds. Each LIGAND-SET™ contains 40-80 high purity (>96%), small organic ligands arranged by pharmacological class in a 96-well format, one compound (2 mg) per well (1 ml capacity). N Standardize/validate new screening assays with well-characterized ligands N Guide secondary screening of larger, diverse libraries using pharmaceutically-relevant structures N Screen new drug targets for leads with pharmacologically-active compounds Nine different LIGAND-SETS™ are now available: N Adrenergics (Prod. No. L 0383) N Enzyme Inhibitors (Prod. No. L 6787) N Purines/Pyrimidines (Prod. No. L 2538) N Cholinergics (Prod. No. L 2663) N GABAergics (Prod. No. L 7884) N Glutamatergics (Prod. No. L 6537) N Dopaminergics (Prod. No. L 6412) N Ion Channel Modulators (Prod. No. L 6912) N Serotonergics (Prod. No. L 6662) For further information, please visit our Drug Discovery website at sigma-aldrich.com/drugdiscovery Technical information for each compound is provided in standard SD file format for use with ISIS/Base or other compatible software (software not provided). SCH 58261: A potent and selective non-xanthine A2A adenosine receptor antagonist Vol. 19 No. 4 Vol. Adenosine (Prod. No. A 9251) acts as a modulator of [3]. These results suggest a neuroprotective effect of this neuronal activity through its interaction with four receptor compound. In another study, the role of A1 and A2A subtypes referred to as A1, A2A, A2B and A3. -

1 Effect of Indacaterol, a Novel Long-Acting Beta 2
ERJ Express. Published on November 29, 2006 as doi: 10.1183/09031936.00032806 EFFECT OF INDACATEROL, A NOVEL LONG-ACTING BETA 2-AGONIST, ON HUMAN ISOLATED BRONCHI Emmanuel Naline (1), Alexandre Trifilieff (2), Robin A. Fairhurst (2), Charles Advenier (1), Mathieu Molimard (3) (1) Research Unit EA220, Université de Versailles, Faculté de Médecine, Pharmacology, Hôpital Foch, 40 rue Worth, 92150 Suresnes, France (2) Novartis Institute for BioMedical Research, Horsham, England (3) Département de Pharmacologie, Université Victor Segalen Bordeaux 2; CHU Pellegrin; INSERM U657, Bordeaux, France Correspondence: Mathieu Molimard Département de Pharmacologie CHU de Bordeaux - Université Victor Segalen-INSERM U657 33076 Bordeaux cedex, France Phone: 33 (0)5 57 57 15 60 Fax: 33 (0)5 57 57 46 71 E-mail: [email protected] Short title: Indacaterol effect on isolated human bronchi 1 Copyright 2006 by the European Respiratory Society. Abstract Indacaterol is a novel β2-adrenoceptor agonist in development for the once-daily treatment of asthma and COPD. This study evaluated the relaxant effect of indacaterol on isolated human bronchi obtained from lungs of patients undergoing surgery for lung carcinoma. Potency (-logEC50), intrinsic efficacy (Emax) and onset of action were determined at resting tone. Duration of action was determined against cholinergic neural contraction induced by electrical field stimulation (EFS). At resting tone, -logEC50 and Emax values were, respectively, 8.82±0.41 and 77±5% for indacaterol, 9.84±0.22 and 94±1% for formoterol, 8.36±0.16 and 74±4% for salmeterol, and 8.43±0.22 and 84±4% for salbutamol. In contrast to salmeterol, indacaterol did not antagonize the isoprenaline response. -
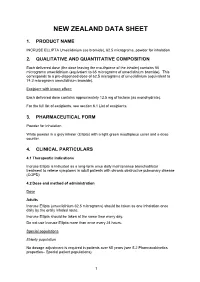
New Zealand Data Sheet
NEW ZEALAND DATA SHEET 1. PRODUCT NAME INCRUSE ELLIPTA Umeclidinium (as bromide), 62.5 micrograms, powder for inhalation 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each delivered dose (the dose leaving the mouthpiece of the inhaler) contains 55 micrograms umeclidinium (equivalent to 65 micrograms of umeclidinium bromide). This corresponds to a pre-dispensed dose of 62.5 micrograms of umeclidinium (equivalent to 74.2 micrograms umeclidinium bromide). Excipient with known effect: Each delivered dose contains approximately 12.5 mg of lactose (as monohydrate). For the full list of excipients, see section 6.1 List of excipients. 3. PHARMACEUTICAL FORM Powder for Inhalation White powder in a grey inhaler (Ellipta) with a light green mouthpiece cover and a dose counter. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Incruse Ellipta is indicated as a long-term once daily maintenance bronchodilator treatment to relieve symptoms in adult patients with chronic obstructive pulmonary disease (COPD). 4.2 Dose and method of administration Dose Adults Incruse Ellipta (umeclidinium 62.5 micrograms) should be taken as one inhalation once daily by the orally inhaled route. Incruse Ellipta should be taken at the same time every day. Do not use Incruse Ellipta more than once every 24 hours. Special populations Elderly population No dosage adjustment is required in patients over 65 years (see 5.2 Pharmacokinetics properties– Special patient populations). 1 Renal impairment No dosage adjustment is required in patients with renal impairment (see 5.2 Pharmacokinetics properties – Special patient populations). Hepatic impairment No dosage adjustment is required in patients with mild or moderate hepatic impairment. Incruse Ellipta has not been studied in patients with severe hepatic impairment (see 5.2 Pharmacokinetics properties– Special patient populations). -

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group R01 (Nasal preparations) Table of Contents Page INTRODUCTION 5 DISCLAIMER 7 GLOSSARY OF TERMS USED IN THIS DOCUMENT 8 ACTIVE SUBSTANCES Cyclopentamine (ATC: R01AA02) 10 Ephedrine (ATC: R01AA03) 11 Phenylephrine (ATC: R01AA04) 14 Oxymetazoline (ATC: R01AA05) 16 Tetryzoline (ATC: R01AA06) 19 Xylometazoline (ATC: R01AA07) 20 Naphazoline (ATC: R01AA08) 23 Tramazoline (ATC: R01AA09) 26 Metizoline (ATC: R01AA10) 29 Tuaminoheptane (ATC: R01AA11) 30 Fenoxazoline (ATC: R01AA12) 31 Tymazoline (ATC: R01AA13) 32 Epinephrine (ATC: R01AA14) 33 Indanazoline (ATC: R01AA15) 34 Phenylephrine (ATC: R01AB01) 35 Naphazoline (ATC: R01AB02) 37 Tetryzoline (ATC: R01AB03) 39 Ephedrine (ATC: R01AB05) 40 Xylometazoline (ATC: R01AB06) 41 Oxymetazoline (ATC: R01AB07) 45 Tuaminoheptane (ATC: R01AB08) 46 Cromoglicic Acid (ATC: R01AC01) 49 2 Levocabastine (ATC: R01AC02) 51 Azelastine (ATC: R01AC03) 53 Antazoline (ATC: R01AC04) 56 Spaglumic Acid (ATC: R01AC05) 57 Thonzylamine (ATC: R01AC06) 58 Nedocromil (ATC: R01AC07) 59 Olopatadine (ATC: R01AC08) 60 Cromoglicic Acid, Combinations (ATC: R01AC51) 61 Beclometasone (ATC: R01AD01) 62 Prednisolone (ATC: R01AD02) 66 Dexamethasone (ATC: R01AD03) 67 Flunisolide (ATC: R01AD04) 68 Budesonide (ATC: R01AD05) 69 Betamethasone (ATC: R01AD06) 72 Tixocortol (ATC: R01AD07) 73 Fluticasone (ATC: R01AD08) 74 Mometasone (ATC: R01AD09) 78 Triamcinolone (ATC: R01AD11) 82 -

Intranasal Rhinitis Agents
Intranasal Rhinitis Agents Therapeutic Class Review (TCR) February 1, 2020 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. -

Early Protective Effects of Tiotropium Bromide in Patients with Airways Hyperres P O N S I V E N E S S
European Review for Medical and Pharmacological Sciences 2004; 8: 259-264 Early protective effects of tiotropium bromide in patients with airways hyperres p o n s i v e n e s s C. TERZANO, A. PETROIANNI, A. RICCI, L. D’ANTONI, L. ALLEGRA* Department of Cardiovascular and Respiratory Sciences, Respiratory Diseases Unit, Fondazione E. Lorillard Spencer Cenci, “La Sapienza” University - Rome (Italy) *Institute of Respiratory Diseases, University of Milan, Ospedale Maggiore IRCCS – Milan (Italy) Abstract. – Tiotropium is an anticholiner- Introduction gic drug for Ch ronic Obstructive Pulmonary Di sease (COPD) patients, with a peak b ron- Ti o t rop ium is a qu atern a ry amm o niu m chodilator effect observed after 1.5 to 2 hours and a long duration of action. The aim of our co ngener of atropine. It has been developed study was to quantify the early protection of a as a lon g-acting an ticho linergic bro n c h o d i l a- single dose of inhaled tiotropium against metha- tor for inhalation by patients with chronic ob- choline-induced bronchoconstriction in asthmat- s t ructive pu lmon ary d isease (COPD). Dru g ic patients with airway hyperresponsiveness. p ro p e rties o f ant icho lin ergic agent s have Ten subjects (7M, 3F), with history of asthma been well-kno wn to man y cultures for many and a baseline FEV (Forced Expiratory Volume 1 1 1 c e n t u r i e s . In the 1920s the d iscovery o f the sec) >80% of pred icted, were enrolled in the s t u d y. -

Non-Steroidal Drug-Induced Glaucoma MR Razeghinejad Et Al 972
Eye (2011) 25, 971–980 & 2011 Macmillan Publishers Limited All rights reserved 0950-222X/11 www.nature.com/eye 1,2 1 1 Non-steroidal drug- MR Razeghinejad , MJ Pro and LJ Katz REVIEW induced glaucoma Abstract vision. The majority of drugs listed as contraindicated in glaucoma are concerned with Numerous systemically used drugs are CAG. These medications may incite an attack in involved in drug-induced glaucoma. Most those individuals with narrow iridocorneal reported cases of non-steroidal drug-induced angle.3 At least one-third of acute closed-angle glaucoma are closed-angle glaucoma (CAG). glaucoma (ACAG) cases are related to an Indeed, many routinely used drugs that have over-the-counter or prescription drug.1 Prevalence sympathomimetic or parasympatholytic of narrow angles in whites from the Framingham properties can cause pupillary block CAG in study was 3.8%. Narrow angles are more individuals with narrow iridocorneal angle. The resulting acute glaucoma occurs much common in the Asian population. A study of a more commonly unilaterally and only rarely Vietnamese population estimated a prevalence 4 bilaterally. CAG secondary to sulfa drugs is a of occludable angles at 8.5%. The reported bilateral non-pupillary block type and is due prevalence of elevated IOP months to years to forward movement of iris–lens diaphragm, after controlling ACAG with laser iridotomy 5,6 which occurs in individuals with narrow or ranges from 24 to 72%. Additionally, a open iridocorneal angle. A few agents, significant decrease in retinal nerve fiber layer including antineoplastics, may induce thickness and an increase in the cup/disc ratio open-angle glaucoma. -

COPD: Treatment Updates and Transitions of Care
COPD: Treatment Updates and Transitions of Care PRESENTED AS A LIVE WEBINAR ON-DEMAND ACTIVITY Thursday, May 21, 2020 Release date: 5/31/2020 1:00 p.m. - 2:00 p.m. Expiration date: 5/31/2023 FACULTY Dennis M. Williams, Pharm.D., BCPS, AE-C, FASHP, FCCP, FAPhA Associate Professor Division of Pharmacotherapy and Experimental Therapeutics UNC Eshelman School of Pharmacy University of North Carolina Chapel Hill, North Carolina Bradley Drummond, M.D., MHS Associate Professor of Medicine University of North Carolina at Chapel Hill Chapel Hill, North Carolina View faculty bios at https://www.copdcare.org/faculty-bios.php ASHP FINANCIAL RELATIONSHIP DISCLOSURE STATEMENT Planners, presenters, reviewers, ASHP staff, and others with an opportunity to control CE content are required to disclose relevant financial relationships with ACCME-defined commercial interests. All actual conflicts of interest have been resolved prior to the continuing education activity taking place. ASHP will disclose financial relationship information prior to the beginning of the activity. A relevant financial relationship is a defined as a financial relationship between an individual (or spouse/partner) in control of content and a commercial interest, in any amount, in the past 12 months, and products and/or services of the commercial interest (with which they have the financial relationship) are related to the continuing education activity. An ACCME-defined commercial interest is any entity producing, marketing re-selling, or distributing healthcare goods or services consumed by, or used on, patients. The ACCME does not consider providers of clinical serve directly to patients to be commercial interests—unless the provider of clinical service is owned, or controlled by, an ACCME-defined commercial interest. -
Advantages and Disadvantages of Beta- Adrenergic Blocking Drugs in Hypertension
Reprinted from ANCIOLOCY Vol. 29, No. -I April 1978 Copyright 0 1978 Prinred in U.S.A. All Rights Rewrced Advantages and Disadvantages of Beta- Adrenergic Blocking Drugs in Hypertension Eoin T. O'Brien DUBLIN, IRELAND General Measures Elevation of blood pressure should be regarded as one of a number of potential risk factors for cardiovascular disease-albeit a major risk factor- rather than a disease per se.' It is important to identify additional risk factors in the hypertensive patient, not only because collectively these factors may greatly magnify the cardiovascular risk, but also because modification of them may, of itself, lower the blood pressure and thus alleviate the risk and save the patient the inconvenience, expense, and potential harm that may result from even the simplest of drug regimes. Careful consideration should be given to the patient's diet (particularly in relation to the calorie intake in the case of obesity, the cholesterol and saturated fat content in the case of hyperlipidemia and patients at high risk, and the salt content) and to smoking habits, physical activity. stress. personality, and drug therapy, especially anovulant preparations. Other diseases, such as diabetes mellitus, which are associated with a high incidence of hypertension and pri- mary causes of hypertension must be excluded. Although there is still no statistical evidence to show that modification of these risk factors-with the exception of tobacco and anovulant preparations-will actually reduce mortal- ity, it does seem prudent on the basis of the evidence available to encourage the hypertensive patient to adjust his or her life-style not only to reduce the cardiovascular risk,2 but also because in many instances the mildly hypertensive patient will respond to this approach alone. -

Drug Class Review Antianginal Agents
Drug Class Review Antianginal Agents 24:12.08 Nitrates and Nitrites 24:04.92 Cardiac Drugs, Miscellaneous Amyl Nitrite Isosorbide Dinitrate (IsoDitrate ER®, others) Isosorbide Mononitrate (Imdur®) Nitroglycerin (Minitran®, Nitrostat®, others) Ranolazine (Ranexa®) Final Report May 2015 Review prepared by: Melissa Archer, PharmD, Clinical Pharmacist Carin Steinvoort, PharmD, Clinical Pharmacist Gary Oderda, PharmD, MPH, Professor University of Utah College of Pharmacy Copyright © 2015 by University of Utah College of Pharmacy Salt Lake City, Utah. All rights reserved. Table of Contents Executive Summary ......................................................................................................................... 3 Introduction .................................................................................................................................... 4 Table 1. Antianginal Therapies .............................................................................................. 4 Table 2. Summary of Agents .................................................................................................. 5 Disease Overview ........................................................................................................................ 8 Table 3. Summary of Current Clinical Practice Guidelines .................................................... 9 Pharmacology ............................................................................................................................... 10 Table 4. Pharmacokinetic Properties -

Reference List of Drugs with Potential Anticholinergic Effects 1, 2, 3, 4, 5
ANTICHOLINERGICS: Reference List of Drugs with Potential Anticholinergic Effects 1, 2, 3, 4, 5 J Bareham BSP © www.RxFiles.ca Aug 2021 WHENEVER POSSIBLE, AVOID DRUGS WITH MODERATE TO HIGH ANTICHOLINERGIC ACTIVITY IN OLDER ADULTS (>65 YEARS OF AGE) Low Anticholinergic Activity; Moderate/High Anticholinergic Activity -B in combo Beers Antibiotics Antiparkinsonian Cardiovascular Agents Immunosuppressants ampicillin *ALL AVAILABLE AS amantadine SYMMETREL atenolol TENORMIN azaTHIOprine IMURAN cefOXitin GENERIC benztropine mesylate COGENTIN captopril CAPOTEN cyclosporine NEORAL clindamycin bromocriptine PARLODEL chlorthalidone GENERIC ONLY hydrocortisone CORTEF gentamicin (Oint & Sol’n NIHB covered) carbidopa/levodopa SINEMET digoxin LANOXIN, TOLOXIN methylprednisolone MEDROL piperacillin entacapone COMTAN dilTIAZem CARDIZEM, TIAZAC prednisone WINPRED dipyridamole PERSANTINE, ethopropazine PARSITAN vancomycin phenelzine NARDIL AGGRENOX disopyramide RYTHMODAN Muscle Relaxants pramipexole MIRAPEX Antidepressants baclofen LIORESAL ( on intrathecal only) procyclidine KEMADRIN furosemide LASIX amitriptyline ELAVIL cyclobenzaprine FLEXERIL selegiline ELDEPRYL hydrALAZINE APRESOLINE clomiPRAMINE ANAFRANIL isosorbide ISORDIL methocarbamol ROBAXIN OTC trihexyphenidyl ARTANE desipramine NORPRAMIN metoprolol LOPRESOR orphenadrine NORFLEX OTC doxepin >6mg SINEQUAN Antipsychotics NIFEdipine ADALAT tiZANidine ZANAFLEX A imipramine TOFRANIL quiNIDine GENERIC ONLY C ARIPiprazole ABILIFY & MAINTENA -

Stable Pressurised Aerosol Solution Composition of Glycopyrronium Bromide and Formoterol Combination
(19) TZZ¥¥_T (11) EP 3 384 898 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 10.10.2018 Bulletin 2018/41 A61K 9/00 (2006.01) A61M 15/00 (2006.01) A61K 31/167 (2006.01) A61K 31/40 (2006.01) (2006.01) (2006.01) (21) Application number: 18171127.6 B65D 83/54 A61K 31/573 A61K 31/54 (2006.01) A61K 45/06 (2006.01) (2006.01) (2006.01) (22) Date of filing: 23.12.2014 A61K 9/12 A61K 31/58 A61M 39/22 (2006.01) (84) Designated Contracting States: • COPELLI, Diego AL AT BE BG CH CY CZ DE DK EE ES FI FR GB 43100 PARMA (IT) GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO • DAGLI ALBERI, Massimiliano PL PT RO RS SE SI SK SM TR 43100 PARMA (IT) Designated Extension States: • USBERTI, Francesca BA ME 43100 PARMA (IT) • ZAMBELLI, Enrico (30) Priority: 30.12.2013 EP 13199784 43100 PARMA (IT) (62) Document number(s) of the earlier application(s) in (74) Representative: Bianchetti Bracco Minoja S.r.l. accordance with Art. 76 EPC: Via Plinio, 63 14825154.9 / 3 089 735 20129 Milano (IT) (71) Applicant: Chiesi Farmaceutici S.p.A. Remarks: 43100 Parma (IT) This application was filed on 08-05-2018 as a divisional application to the application mentioned (72) Inventors: under INID code 62. • BONELLI, Sauro 43100 PARMA (IT) (54) STABLE PRESSURISED AEROSOL SOLUTION COMPOSITION OF GLYCOPYRRONIUM BROMIDE AND FORMOTEROL COMBINATION (57) The invention concerns an aerosol solution lower than the limit of quantification, when stored in ac- composition intended for use with a pressurised metered celerated conditions at 25°C and 60% relative humidity dose inhaler, comprising glycopyrronium bromide and (RH) for 6 months in a can internally coated by a resin formoterol, or a salt thereof or a solvate of said salt, op- comprising a fluorinated ethylene propylene (FEP) poly- tionally in combination with one or more additional active mer.