PRODUCT MONOGRAPH ELAVIL® Amitriptyline Hydrochloride Tablets
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Experience in Schizophrenia: a Neuromedicine New Option to Address Unmet Needs
Bhat L, Cantillon M, Ings R. Brilaroxazine (RP5063) Clinical Experience in Schizophrenia: A Neuromedicine New Option to Address Unmet Needs. J Neurol Neuromedicine (2018) 3(5): 39-50 www.jneurology.com www.jneurology.com Journal of Neurology && NeuromedicineNeuromedicine Review Article Open Access Brilaroxazine (RP5063) Clinical Experience in Schizophrenia: A New Option to Address Unmet Needs Laxminarayan Bhat*, Marc Cantillon, and Robert Ings Reviva Pharmaceuticals, Inc., Sunnyvale, CA, USA Article Info ABSTRACT Article Notes Schizophrenia is a condition comprising of both treatment and comorbidity Received: September 18, 2018 factors that both complicate its management and present multiple unmet needs. Accepted: October 22, 2018 Brilaroxazine (RP5063), a dopamine (D)/serotonin (5-HT) modulator, possesses in vitro *Correspondence: a broad pharmacology profile against D2/3/4 and 5-HT1A/2A/2B/6/7 receptors, Dr. Laxminarayan Bhat, 1250 Oakmead Parkway, Suite 210, nicotinic acetylcholine (α4β2) receptors, and the serotonin transporter. In Phase 1 Sunnyvale, CA 94085, USA; Telephone No. +1 (408) 816 1454; and 2 clinical experience in healthy volunteers, patients with schizophrenia and Fax No. +1 (408) 904 6270; ORCID Number: 0000-0003-0503- schizoaffective disorder, brilaroxazine was well tolerated, with the repeated 100 mg 8537; Email: [email protected]. oral dose as the maximum tolerated dose. Investigators observed no cardiometabolic, cardiovascular, prolactin, or neurologic complications. Adherence in Phase 2 was © 2018 Bhat L. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License good with discontinuation rates generally less than placebo. In a Phase 2 evaluation of patients with acute exacerbations in schizophrenia and schizoaffective disorders, brilaroxazine met its primary endpoint of significance versus placebo for Total Positive and Negative Symptom Scale (PANSS) Score at Day 28 as compared to baseline. -

Medication: Amitriptyline 10 Mg
Amitriptyline (Elavil) COMPLEX CHRONIC DISEASES PROGRAM Medication Handout Date: May 15, 2018 Medication: Amitriptyline 10 mg What is Amitriptyline? Amitriptyline belongs to a group of medications called tricyclic antidepressants (TCAs) that were first used to treat depression. It works by altering the levels of certain neuro- transmitters in the brain such as noradrenalin and serotonin. They have since been found to be effective for many different uses such as: pain, helping with sleep quality (but is not a sleeping pill), irritable bowel syndrome (with diarrhea), migraine prevention, and interstitial cystitis. Expected Benefit: Usually takes several weeks to notice a benefit You may not notice a benefit until you get to a dose of 25 mg Watch for possible side effects: This list of side effects is important for you to be aware of; however, it is also important to remember that not all side effects happen to all people. Many of these less serious side effects will improve over the first few days of taking the medications. If you have problems with these side effects talk with your doctor or pharmacist: Dry mouth – this is the most common side; the others are much less frequent Hangover effect – too sleepy in the morning Blurred vision Urinary retention, trouble with urination Tiredness, dizziness that is more than usual Diarrhea or constipation Stopping the medication: Do NOT stop taking this medication suddenly without asking your doctor – this medication is usually decreased slowly (at higher doses) before it is stopped completely How to use this medication: Take this medication with or without food Dosing Schedule: Start with 5 mg (½ tablet) 2 hrs before bed Increase dose according to table below Many patients can only tolerate 20 or 30 mg If you don’t have dry mouth or side effects, you can continue slowly increasing the dose to a maximum of 70 mg You can stay at a lower dose (stop increasing) if you get side effects (usually dry mouth). -

Chronic Olanzapine Or Sertindole Treatment Results in Reduced Oral Chewing Movements in Rats Compared to Haloperidol Xue-Min Gao, M.D., Kazuo Sakai, M.D., and Carol A
Chronic Olanzapine or Sertindole Treatment Results in Reduced Oral Chewing Movements in Rats Compared to Haloperidol Xue-Min Gao, M.D., Kazuo Sakai, M.D., and Carol A. Tamminga, M.D. Chronic haloperidol treatment typically produces late-onset, haloperidol-like chewing in rats, nor did movement ratings purposeless oral chewing movements in laboratory rats with after their chronic administration differ from placebo; a prevalence of 40 to 60%. Chronic clozapine does not whereas, haloperidol produced a 60% prevalence of produce these movements. Based on the phenomenologic purposeless chewing and a prevalence significantly and pharmacologic similarities between these rat chewing increased from placebo. This low rate of oral dyskinesias in movements and human tardive dyskinesia (TD), the animal rats is consistent with several of the preclinical movements are often used as a model of tardive dyskinesia characteristics of the drugs and correlates with their low (TD). Here we report results of the association of oral acute motor side effects in clinical trials. We propose, chewing movements in rats with chronic administration of although have not yet tested in humans, that these animal two new antipsychotic drugs, olanzapine and sertindole. results will predict low TD liability of these drugs. Because each of these antipsychotic drugs has a very low [Neuropsychopharmacology 19:428–433, 1998] incidence of acute Parkinsonism in human studies, they are © 1998 American College of Neuropsychopharmacology. candidates for showing a low tardive dyskinesia risk. Published by Elsevier Science Inc. Neither new drug produced a significant incidence of KEY WORDS: Dyskinesia; Olanzapine; Sertindole; movements parallel certain features (although not all) Haloperidol; Tardive dyskinesia; Chronic neuroleptic of the human neuroleptic-induced dyskinetic syndrome treatment tardive dyskinesia (TD), they are often used in its study. -
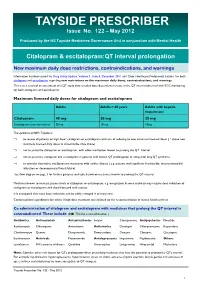
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -

COPD Agents Review – October 2020 Page 2 | Proprietary Information
COPD Agents Therapeutic Class Review (TCR) October 1, 2020 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. October 2020 -

PERPHENAZINE and AMITRIPTYLINE HYDROCHLORIDE- Perphenazine and Amitriptyline Hydrochloride Tablet, Film Coated Mylan Pharmaceuticals Inc
PERPHENAZINE AND AMITRIPTYLINE HYDROCHLORIDE- perphenazine and amitriptyline hydrochloride tablet, film coated Mylan Pharmaceuticals Inc. ---------- WARNING Increased Mortality in Elderly Patients with Dementia-Related Psychosis Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug- treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. Perphenazine and amitriptyline hydrochloride is not approved for the treatment of patients with dementia- related psychosis (see WARNINGS). Suicidality and Antidepressant Drugs Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of perphenazine and amitriptyline or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. -

Nuedexta) National Drug Monograph May 2013 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives
Dextromethorphan/ Quinidine Monograph Dextromethorphan Hydrobromide and Quinidine Sulfate (Nuedexta) National Drug Monograph May 2013 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a comprehensive drug review for making formulary decisions. These documents will be updated when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. Executive Summary: Current therapy for pseudobulbar affect (PBA) typically utilizes non-pharmacologic coping strategies such as relaxation and distraction techniques. The off-label use of selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs) and dopaminergic agents has found limited success in treating PBA exacerbations. Dextromethorphan/quinidine (Nuedexta) is a combination of two existing generic formulary options; however quinidine is not available in an appropriate strength or in a liquid formulation (200mg, 300mg capsules only). Low dose quinidine inhibits the rapid metabolism of dextromethorphan, therefore increasing the bioavailability of dextromethorphan, resulting in effective plasma levels. In a double-blind, placebo-controlled study, the combination of dextromethorphan (20 or 30 mg) and low dose quinidine (10 mg) [STAR trial] significantly reduced the frequency of pseudobulbar affect episodes vs. placebo over the course of 12 weeks of treatment (p < 0.0001). Patients in the dextromethorphan/quinidine 20 mg/10 mg group reported a mean weekly episode reduction of 82% from baseline vs. a reduction of 47% in the placebo group (p = 0.001). Mean Center for Neurological Study-Lability Scale (CNS-LS) scores decreased by 8.2 points for both dextromethorphan/quinidine dosage groups vs. -

Amitriptyline (Elavil): Important Patient Information
What is most important to remember? If you have questions: Strong Internal Medicine • You must check to make sure that it is safe for you to take Ask your doctor, nurse or pharmacist for amitriptyline with all of your other more information about amitriptyline medicines and health problems (Elavil®). • Do not start any new medications, over-the-counter drugs or herbal remedies without talking to your doctor • Contact your prescriber If your symptoms or health problems do not get any better or they become worse • This medicine comes with an Strong Internal Medicine extra patient fact sheet called a 601 Elmwood Avenue Medication Guide. Read it with Ambulatory Care Facility, 5th Floor care. Read it again each time this Rochester, NY 14642 Phone: (585) 275 -7424 medicine is refilled Amitriptyline (Elavil®): • If you think there has been an Visit our website at: Important Patient Information www.urmc.rochester.edu/medicine/ - overdose, call your poison control general-medicine/patientcare/ center or get medical care right away What does amitriptyline (Elavil®) do? What side effects could occur with amitriptyline What are some things that I need to be aware of when • It belongs to a class of medications called tricyclic (Elavil®)? taking amitriptyline (Elavil®)? antidepressants (TCAs). It works by increasing the • Hard stools (constipation) • Tell your doctor or pharmacist if you are allergic to amitriptyline, any other medicines, foods, or substances amounts of certain natural substances in the brain that • Dizziness, feeling sleepy are needed -

Trimbow, INN-Beclometasone Dipropionate, Formoterol Fumarate
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Trimbow 87 micrograms/5 micrograms/9 micrograms pressurised inhalation, solution 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each delivered dose (the dose leaving the mouthpiece) contains 87 micrograms of beclometasone dipropionate, 5 micrograms of formoterol fumarate dihydrate and 9 micrograms of glycopyrronium (as 11 micrograms glycopyrronium bromide). Each metered dose (the dose leaving the valve) contains 100 micrograms of beclometasone dipropionate, 6 micrograms of formoterol fumarate dihydrate and 10 micrograms of glycopyrronium (as 12.5 micrograms glycopyrronium bromide). Excipient with known effect Trimbow contains 8.856 mg ethanol per actuation. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Pressurised inhalation, solution (pressurised inhalation). Colourless to yellowish liquid solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications COPD Maintenance treatment in adult patients with moderate to severe chronic obstructive pulmonary disease (COPD) who are not adequately treated by a combination of an inhaled corticosteroid and a long-acting beta2-agonist or a combination of a long-acting beta2-agonist and a long-acting muscarinic antagonist (for effects on symptoms control and prevention of exacerbations see section 5.1). Asthma Maintenance treatment of asthma, in adults not adequately controlled with a maintenance combination of a long-acting beta2-agonist and medium dose of inhaled corticosteroid, and who experienced one or more asthma exacerbations in the previous year. 4.2 Posology and method of administration Posology Adults The recommended dose is two inhalations twice daily. The maximum dose is two inhalations twice daily. Patients should be advised to take Trimbow every day even when asymptomatic. -

Antipsychotics
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35 Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 Class Update with New Drug Evaluations: Antipsychotics Date of Review: May 2016 End Date of Literature Search: February 2016 New Drugs: brexpiprazole Brand Names (Manufacturer): Rexulti® (Otsuka) cariprazine Vraylar™ (Actavis) Dossiers Received: yes PDL Classes: Antipsychotics, First generation Antipsychotics, Second generation Antipsychotics, Parenteral Current Status of PDL Class: See Appendix 1. Purpose for Class Update: Several new antipsychotic drug products have been approved by the U.S. Food and Drug Administration since these drug classes were last reviewed by the Oregon Health Plan (OHP) Pharmacy and Therapeutics Committee. Research Questions: 1. Is there new comparative evidence of meaningful difference in efficacy or effectiveness outcomes for schizophrenia, bipolar mania or major depressive disorders (MDD) between oral antipsychotic agents (first‐ or second‐generation) or between parenteral antipsychotic agents (first‐ or second‐generation)? 2. Is there new comparative evidence of meaningful difference in harms between oral antipsychotic agents (first‐ or second‐generation) or between parenteral antipsychotic agents (first‐ or second‐generation)? 3. Is there new comparative evidence of meaningful difference in effectiveness or harms in certain subpopulations based on demographic characteristics? Conclusions: There is insufficient evidence of clinically meaningful differences between antipsychotic agents in efficacy or effectiveness or harms between antipsychotic agents for schizophrenia, bipolar mania or MDD. There is insufficient evidence to determine if brexpiprazole and cariprazine offer superior efficacy or safety to other antipsychotic agents for schizophrenia. There is insufficient evidence to determine if brexpiprazole offers superior efficacy or safety to other antipsychotic agents for MDD. -

Quinidine, Beta-Blockers, Diphenylhydantoin, Bretylium *
Pharmacology of Antiarrhythmics: Quinidine, Beta-Blockers, Diphenylhydantoin, Bretylium * ALBERT J. WASSERMAN, M.D. Professor of Medicine, Chairman, Division of Clinical Pharmacology, Medical College of Virginia, Health Sciences Division of Virginia Commonwealth University, Richmond, Virginia JACK D. PROCTOR, M.D. Assistant Professor of Medicine, Medical College of Virginia, Health Sciences Division of Virginia Commonwealth University, Richmond, Virginia The electrophysiologic effects of the antiar adequate, controlled clinical comparisons are virtu rhythmic drugs, presented elsewhere in this sym ally nonexistent. posium, form only one of the bases for the selec A complete presentation of the non-electro tion of a therapeutic agent in any given clinical physiologic pharmacology would include the follow situation. The final choice depends at least on the ing considerations: following factors: 1. Absorption and peak effect times 1. The specific arrhythmia 2. Biotransformation 2. Underlying heart disease, if any 3. Rate of elimination or half-life (t1d 3. The degree of compromise of the circula 4. Drug interactions tion, if any 5. Toxicity 4. The etiology of the arrhythmia 6. Clinical usefulness 5. The efficacy of the drug for that arrhythmia 7. Therapeutic drug levels due to that etiology 8. Dosage schedules 6. The toxicity of the drug, especially in the As all of the above data cannot be presented in given patient with possible alterations in the limited space available, only selected items will volume of distribution, biotransformation, be discussed. Much of the preceding information and excretion is available, however, in standard texts ( 1 7, 10). 7. The electrophysiologic effects of the drug (See Addendum 1) 8. The routes and frequency of administration Quinidine. -

The Metabolic Side Effects of 12 Antipsychotic Drugs Used for The
Zhang et al. BMC Psychiatry (2017) 17:373 DOI 10.1186/s12888-017-1539-0 RESEARCHARTICLE Open Access The metabolic side effects of 12 antipsychotic drugs used for the treatment of schizophrenia on glucose: a network meta-analysis Yangyu Zhang†, Yingyu Liu†, Yingying Su, Yueyue You, Yue Ma, Guang Yang, Yan Song, Xinyu Liu, Mohan Wang, Lili Zhang and Changgui Kou* Abstract Background: Antipsychotics have serious metabolic side effects on blood glucose. However, the comparative influence of these drugs on blood glucose levels has not been comprehensively evaluated. We conducted a network meta-analysis to create a hierarchy of the side effects of 12 antipsychotic drugs on changes in blood glucose levels. Methods: A systematic search of the PubMed, EMBASE and Cochrane databases (last search June 2016) was conducted to identify studies that reported randomized controlled trials (RCTs) comparing changes in blood glucose levels between patients receiving one of 12 antipsychotic drugs or a placebo for the treatment of schizophrenia or related disorders. The studies we searched were limited to those published in English. Two reviewers independently extracted data. The primary outcome of interest was changes in fasting glucose levels. Results: We included 47 studies with 114 relevant arms. Of the antipsychotic drugs, only olanzapine was associated with significantly increased glucose levels compared to a placebo (mean difference (MD) = 3.95, 95% confidence interval (CI) = 0.14 to 7.76). Moreover, olanzapine was associated with a significantly greater change in the glucose levels than ziprasidone (MD = 5.51, 95% CI = 1.62 to 9.39), lurasidone (MD = 5.58, 95% CI = 0.53 to 10.64) or risperidone (MD = 3.05, 95% CI = 0.87 to 5.22).