DBL™ Promethazine Hydrochloride Injection BP
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Comparing the Effect of Venlafaxine and the Combination of Nortriptyline and Propranolol in the Prevention of Migraine
Comparing the Effect of Venlafaxine and the Combination of Nortriptyline and Propranolol in the Prevention of Migraine Arash Mosarrezaii1, Mohammad Reza Amiri Nikpour1, Ata Jabarzadeh2 1Department of Neurology, Imam Khomeini Hospital, Urmia University of Medical Sciences, Urmia, Iran, 2Medical Student, Urmia University of Medical Sciences, Urmia, Iran Abstract Background: Migraine is a debilitating neurological condition, which can be categorized into episodic and chronic groups based on its clinical pattern. Avoiding the risk factors exacerbating migraine is not enough to reduce the frequency and severity of migraine headaches, and in the case of non-receiving proper drug treatment, episodic migraines have the potential to become chronic, which increases the risk of cardiovascular complications RESEARCH ARTICLE and leaves great impact on the quality of life of patients and increasing the health-care costs. The objective of this research was to compare the effects of venlafaxine (VFL) and nortriptyline and propranolol in preventing migraines. Methods: This research is an interventional study performed on 60 patients with migraine admitted to the neurological clinic. Patients were visited at 3 time intervals. In each stage, the variables of headache frequency, headache severity, nausea, vomiting, and drowsiness were recorded. Data were analyzed using SPSS 23 software. Results: VFL drug with a daily dose of 37.5 mg is not only more tolerable in the long term but also leaves better effect in reducing the frequency and severity of headaches compared to the combination of nortriptyline and propranolol. Conclusion: VFL is an appropriate, effective, and tolerable alternative to migraine treatment. Key words: Migraine, nortriptyline, propranolol, venlafaxine INTRODUCTION Patients with CM are less likely to have full-time job than patients with episodic type, and they are at risk of job igraine is known as a common incapacity, anxiety, chronic pain, and depression 2 times neurological disorder and causes more than patients with episodic migraine. -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -
![Selective Labeling of Serotonin Receptors Byd-[3H]Lysergic Acid](https://docslib.b-cdn.net/cover/9764/selective-labeling-of-serotonin-receptors-byd-3h-lysergic-acid-319764.webp)
Selective Labeling of Serotonin Receptors Byd-[3H]Lysergic Acid
Proc. Nati. Acad. Sci. USA Vol. 75, No. 12, pp. 5783-5787, December 1978 Biochemistry Selective labeling of serotonin receptors by d-[3H]lysergic acid diethylamide in calf caudate (ergots/hallucinogens/tryptamines/norepinephrine/dopamine) PATRICIA M. WHITAKER AND PHILIP SEEMAN* Department of Pharmacology, University of Toronto, Toronto, Canada M5S 1A8 Communicated by Philip Siekevltz, August 18,1978 ABSTRACT Since it was known that d-lysergic acid di- The objective in this present study was to improve the se- ethylamide (LSD) affected catecholaminergic as well as sero- lectivity of [3H]LSD for serotonin receptors, concomitantly toninergic neurons, the objective in this study was to enhance using other drugs to block a-adrenergic and dopamine receptors the selectivity of [3HJISD binding to serotonin receptors in vitro by using crude homogenates of calf caudate. In the presence of (cf. refs. 36-38). We then compared the potencies of various a combination of 50 nM each of phentolamine (adde to pre- drugs on this selective [3H]LSD binding and compared these clude the binding of [3HJLSD to a-adrenoceptors), apmo ie, data to those for the high-affinity binding of [3H]serotonin and spiperone (added to preclude the binding of [3H[LSD to (39). dopamine receptors), it was found by Scatchard analysis that the total number of 3H sites went down to 300 fmol/mg, compared to 1100 fmol/mg in the absence of the catechol- METHODS amine-blocking drugs. The IC50 values (concentrations to inhibit Preparation of Membranes. Calf brains were obtained fresh binding by 50%) for various drugs were tested on the binding of [3HLSD in the presence of 50 nM each of apomorphine (A), from the Canada Packers Hunisett plant (Toronto). -
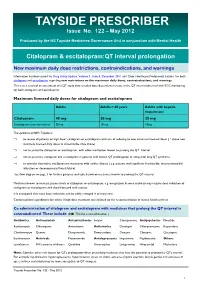
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -

PRODUCT MONOGRAPH ELAVIL® Amitriptyline Hydrochloride Tablets
PRODUCT MONOGRAPH ELAVIL® amitriptyline hydrochloride tablets USP 10, 25, 50 and 75 mg Antidepressant AA PHARMA INC. DATE OF PREPARATION: 1165 Creditstone Road Unit #1 August 29, 2018 Vaughan, ON L4K 4N7 Control No.: 217626 1 PRODUCT MONOGRAPH ELAVIL® amitriptyline hydrochloride tablets USP 10, 25, 50, 75 mg THERAPEUTIC CLASSIFICATION Antidepressant ACTIONS AND CLINICAL PHARMACOLOGY Amitriptyline hydrochloride is a tricyclic antidepressant with sedative properties. Its mechanism of action in man is not known. Amitriptyline inhibits the membrane pump mechanism responsible for the re-uptake of transmitter amines, such as norepinephrine and serotonin, thereby increasing their concentration at the synaptic clefts of the brain. Amitriptyline has pronounced anticholinergic properties and produces EKG changes and quinidine-like effects on the heart (See ADVERSE REACTIONS). It also lowers the convulsive threshold and causes alterations in EEG and sleep patterns. Orally administered amitriptyline is readily absorbed and rapidly metabolized. Steady-state plasma concentrations vary widely and this variation may be genetically determined. Amitriptyline is primarily excreted in the urine, mostly in the form of metabolites, with some excretion also occurring in the feces. INDICATIONS AND CLINICAL USE ELAVIL® (amitriptyline hydrochloride) is indicated in the drug management of depressive illness. ELAVIL® may be used in depressive illness of psychotic or endogenous nature and in selected patients with neurotic depression. Endogenous depression is more likely to be alleviated than are other depressive states. ELAVIL® ®, because of its sedative action, is also of value in alleviating the anxiety component of depression. As with other tricyclic antidepressants, ELAVIL® may precipitate hypomanic episodes in patients with bipolar depression. These drugs are not indicated in mild depressive states and depressive reactions. -

COPD Agents Review – October 2020 Page 2 | Proprietary Information
COPD Agents Therapeutic Class Review (TCR) October 1, 2020 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. October 2020 -

A Drug Repositioning Approach Identifies Tricyclic Antidepressants As Inhibitors of Small Cell Lung Cancer and Other Neuroendocrine Tumors
Published OnlineFirst September 26, 2013; DOI: 10.1158/2159-8290.CD-13-0183 RESEARCH ARTICLE A Drug Repositioning Approach Identifi es Tricyclic Antidepressants as Inhibitors of Small Cell Lung Cancer and Other Neuroendocrine Tumors Nadine S. Jahchan 1 , 2 , Joel T. Dudley 1 , Pawel K. Mazur 1 , 2 , Natasha Flores 1 , 2 , Dian Yang 1 , 2 , Alec Palmerton 1 , 2 , Anne-Flore Zmoos 1 , 2 , Dedeepya Vaka 1 , 2 , Kim Q.T. Tran 1 , 2 , Margaret Zhou 1 , 2 , Karolina Krasinska 3 , Jonathan W. Riess 4 , Joel W. Neal 5 , Purvesh Khatri 1 , 2 , Kwon S. Park 1 , 2 , Atul J. Butte 1 , 2 , and Julien Sage 1 , 2 Downloaded from cancerdiscovery.aacrjournals.org on September 29, 2021. © 2013 American Association for Cancer Research. Published OnlineFirst September 26, 2013; DOI: 10.1158/2159-8290.CD-13-0183 ABSTRACT Small cell lung cancer (SCLC) is an aggressive neuroendocrine subtype of lung cancer with high mortality. We used a systematic drug repositioning bioinformat- ics approach querying a large compendium of gene expression profi les to identify candidate U.S. Food and Drug Administration (FDA)–approved drugs to treat SCLC. We found that tricyclic antidepressants and related molecules potently induce apoptosis in both chemonaïve and chemoresistant SCLC cells in culture, in mouse and human SCLC tumors transplanted into immunocompromised mice, and in endog- enous tumors from a mouse model for human SCLC. The candidate drugs activate stress pathways and induce cell death in SCLC cells, at least in part by disrupting autocrine survival signals involving neurotransmitters and their G protein–coupled receptors. The candidate drugs inhibit the growth of other neuroendocrine tumors, including pancreatic neuroendocrine tumors and Merkel cell carcinoma. -

PERPHENAZINE and AMITRIPTYLINE HYDROCHLORIDE- Perphenazine and Amitriptyline Hydrochloride Tablet, Film Coated Mylan Pharmaceuticals Inc
PERPHENAZINE AND AMITRIPTYLINE HYDROCHLORIDE- perphenazine and amitriptyline hydrochloride tablet, film coated Mylan Pharmaceuticals Inc. ---------- WARNING Increased Mortality in Elderly Patients with Dementia-Related Psychosis Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug- treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. Perphenazine and amitriptyline hydrochloride is not approved for the treatment of patients with dementia- related psychosis (see WARNINGS). Suicidality and Antidepressant Drugs Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of perphenazine and amitriptyline or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. -

Nuedexta) National Drug Monograph May 2013 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives
Dextromethorphan/ Quinidine Monograph Dextromethorphan Hydrobromide and Quinidine Sulfate (Nuedexta) National Drug Monograph May 2013 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a comprehensive drug review for making formulary decisions. These documents will be updated when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. Executive Summary: Current therapy for pseudobulbar affect (PBA) typically utilizes non-pharmacologic coping strategies such as relaxation and distraction techniques. The off-label use of selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs) and dopaminergic agents has found limited success in treating PBA exacerbations. Dextromethorphan/quinidine (Nuedexta) is a combination of two existing generic formulary options; however quinidine is not available in an appropriate strength or in a liquid formulation (200mg, 300mg capsules only). Low dose quinidine inhibits the rapid metabolism of dextromethorphan, therefore increasing the bioavailability of dextromethorphan, resulting in effective plasma levels. In a double-blind, placebo-controlled study, the combination of dextromethorphan (20 or 30 mg) and low dose quinidine (10 mg) [STAR trial] significantly reduced the frequency of pseudobulbar affect episodes vs. placebo over the course of 12 weeks of treatment (p < 0.0001). Patients in the dextromethorphan/quinidine 20 mg/10 mg group reported a mean weekly episode reduction of 82% from baseline vs. a reduction of 47% in the placebo group (p = 0.001). Mean Center for Neurological Study-Lability Scale (CNS-LS) scores decreased by 8.2 points for both dextromethorphan/quinidine dosage groups vs. -

Trimbow, INN-Beclometasone Dipropionate, Formoterol Fumarate
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Trimbow 87 micrograms/5 micrograms/9 micrograms pressurised inhalation, solution 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each delivered dose (the dose leaving the mouthpiece) contains 87 micrograms of beclometasone dipropionate, 5 micrograms of formoterol fumarate dihydrate and 9 micrograms of glycopyrronium (as 11 micrograms glycopyrronium bromide). Each metered dose (the dose leaving the valve) contains 100 micrograms of beclometasone dipropionate, 6 micrograms of formoterol fumarate dihydrate and 10 micrograms of glycopyrronium (as 12.5 micrograms glycopyrronium bromide). Excipient with known effect Trimbow contains 8.856 mg ethanol per actuation. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Pressurised inhalation, solution (pressurised inhalation). Colourless to yellowish liquid solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications COPD Maintenance treatment in adult patients with moderate to severe chronic obstructive pulmonary disease (COPD) who are not adequately treated by a combination of an inhaled corticosteroid and a long-acting beta2-agonist or a combination of a long-acting beta2-agonist and a long-acting muscarinic antagonist (for effects on symptoms control and prevention of exacerbations see section 5.1). Asthma Maintenance treatment of asthma, in adults not adequately controlled with a maintenance combination of a long-acting beta2-agonist and medium dose of inhaled corticosteroid, and who experienced one or more asthma exacerbations in the previous year. 4.2 Posology and method of administration Posology Adults The recommended dose is two inhalations twice daily. The maximum dose is two inhalations twice daily. Patients should be advised to take Trimbow every day even when asymptomatic. -

ANTIDEPRESSANTS in USE in CLINICAL PRACTICE Mark Agius1 & Hannah Bonnici2 1Clare College, University of Cambridge, Cambridge, UK 2Hospital Pharmacy St
Psychiatria Danubina, 2017; Vol. 29, Suppl. 3, pp 667-671 Conference paper © Medicinska naklada - Zagreb, Croatia ANTIDEPRESSANTS IN USE IN CLINICAL PRACTICE Mark Agius1 & Hannah Bonnici2 1Clare College, University of Cambridge, Cambridge, UK 2Hospital Pharmacy St. James Hospital Malta, Malta SUMMARY The object of this paper, rather than producing new information, is to produce a useful vademecum for doctors prescribing antidepressants, with the information useful for their being prescribed. Antidepressants need to be seen as part of a package of treatment for the patient with depression which also includes psychological treatments and social interventions. Here the main Antidepressant groups, including the Selective Serotonin uptake inhibiters, the tricyclics and other classes are described, together with their mode of action, side effects, dosages. Usually antidepressants should be prescribed for six months to treat a patient with depression. The efficacy of anti-depressants is similar between classes, despite their different mechanisms of action. The choice is therefore based on the side-effects to be avoided. There is no one ideal drug capable of exerting its therapeutic effects without any adverse effects. Increasing knowledge of what exactly causes depression will enable researchers not only to create more effective antidepressants rationally but also to understand the limitations of existing drugs. Key words: antidepressants – depression - psychological therapies - social therapies * * * * * Introduction Monoamine oxidase (MAO) inhibitors í Non-selective Monoamine Oxidase Inhibitors Depression may be defined as a mood disorder that í Selective Monoamine Oxidase Type A inhibitors negatively and persistently affects the way a person feels, thinks and acts. Common signs include low mood, Atypical Anti-Depressants and other classes changes in appetite and sleep patterns and loss of inte- rest in activities that were once enjoyable. -

Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss
Supplemental Material can be found at: /content/suppl/2020/12/18/73.1.202.DC1.html 1521-0081/73/1/202–277$35.00 https://doi.org/10.1124/pharmrev.120.000056 PHARMACOLOGICAL REVIEWS Pharmacol Rev 73:202–277, January 2021 Copyright © 2020 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: MICHAEL NADER Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss Antonio Inserra, Danilo De Gregorio, and Gabriella Gobbi Neurobiological Psychiatry Unit, Department of Psychiatry, McGill University, Montreal, Quebec, Canada Abstract ...................................................................................205 Significance Statement. ..................................................................205 I. Introduction . ..............................................................................205 A. Review Outline ........................................................................205 B. Psychiatric Disorders and the Need for Novel Pharmacotherapies .......................206 C. Psychedelic Compounds as Novel Therapeutics in Psychiatry: Overview and Comparison with Current Available Treatments . .....................................206 D. Classical or Serotonergic Psychedelics versus Nonclassical Psychedelics: Definition ......208 Downloaded from E. Dissociative Anesthetics................................................................209 F. Empathogens-Entactogens . ............................................................209