Tricyclic Antidepressant Overdose
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dosulepin Prescribing
SAFETY BULLETIN: DOSULEPIN PRESCRIBING In December 2007, the Medicines and Healthcare Regulatory Agency (MHRA) issued safety advice around prescribing of dosulepin, related to the narrow margin between therapeutic doses and potentially fatal doses. Nevertheless, dosulepin continues to be prescribed widely. Over eight years after the safety advice was published, prescribing of dosulepin in the Dorset area remains high. In the South West area, Dorset CCG was the highest prescriber of dosulepin for the 2015/16 financial year (3.238% of all antidepressant items). Of the 209 CCGs in the UK, Dorset is the fourteenth highest prescriber of dosulepin, and well above the national average of 2.111%. The following points summarise the reasons that dosulepin is not recommended for prescribing nationally, and in Dorset: Dosulepin has a small margin of safety between the (maximum) therapeutic dose and potentially fatal doses. The NICE guideline on depression in adults recommends that dosulepin should not be prescribed for adults with depression because evidence supporting its tolerability relative to other antidepressants is outweighed by the increased cardiac risk and toxicity in overdose. Dosulepin has also been used ‘off label’ in other indications such as fibromyalgia and neuropathic pain. However the evidence for use in in this way is weak, and is not recommended. The lethal dose of dosulepin is relatively low and can be potentiated by alcohol and other CNS depressants. Dosulepin overdose is associated with high mortality and can occur rapidly, even before hospital treatment can be received. Onset of toxicity occurs within 4-6 hours. Every year, up to 200 people in England and Wales fatally overdose with dosulepin. -

Comparing the Effect of Venlafaxine and the Combination of Nortriptyline and Propranolol in the Prevention of Migraine
Comparing the Effect of Venlafaxine and the Combination of Nortriptyline and Propranolol in the Prevention of Migraine Arash Mosarrezaii1, Mohammad Reza Amiri Nikpour1, Ata Jabarzadeh2 1Department of Neurology, Imam Khomeini Hospital, Urmia University of Medical Sciences, Urmia, Iran, 2Medical Student, Urmia University of Medical Sciences, Urmia, Iran Abstract Background: Migraine is a debilitating neurological condition, which can be categorized into episodic and chronic groups based on its clinical pattern. Avoiding the risk factors exacerbating migraine is not enough to reduce the frequency and severity of migraine headaches, and in the case of non-receiving proper drug treatment, episodic migraines have the potential to become chronic, which increases the risk of cardiovascular complications RESEARCH ARTICLE and leaves great impact on the quality of life of patients and increasing the health-care costs. The objective of this research was to compare the effects of venlafaxine (VFL) and nortriptyline and propranolol in preventing migraines. Methods: This research is an interventional study performed on 60 patients with migraine admitted to the neurological clinic. Patients were visited at 3 time intervals. In each stage, the variables of headache frequency, headache severity, nausea, vomiting, and drowsiness were recorded. Data were analyzed using SPSS 23 software. Results: VFL drug with a daily dose of 37.5 mg is not only more tolerable in the long term but also leaves better effect in reducing the frequency and severity of headaches compared to the combination of nortriptyline and propranolol. Conclusion: VFL is an appropriate, effective, and tolerable alternative to migraine treatment. Key words: Migraine, nortriptyline, propranolol, venlafaxine INTRODUCTION Patients with CM are less likely to have full-time job than patients with episodic type, and they are at risk of job igraine is known as a common incapacity, anxiety, chronic pain, and depression 2 times neurological disorder and causes more than patients with episodic migraine. -

Medication Conversion Chart
Fluphenazine FREQUENCY CONVERSION RATIO ROUTE USUAL DOSE (Range) (Range) OTHER INFORMATION KINETICS Prolixin® PO to IM Oral PO 2.5-20 mg/dy QD - QID NA ↑ dose by 2.5mg/dy Q week. After symptoms controlled, slowly ↓ dose to 1-5mg/dy (dosed QD) Onset: ≤ 1hr 1mg (2-60 mg/dy) Caution for doses > 20mg/dy (↑ risk EPS) Cmax: 0.5hr 2.5mg Elderly: Initial dose = 1 - 2.5mg/dy t½: 14.7-15.3hr 5mg Oral Soln: Dilute in 2oz water, tomato or fruit juice, milk, or uncaffeinated carbonated drinks Duration of Action: 6-8hr 10mg Avoid caffeinated drinks (coffee, cola), tannics (tea), or pectinates (apple juice) 2° possible incompatibilityElimination: Hepatic to inactive metabolites 5mg/ml soln Hemodialysis: Not dialyzable HCl IM 2.5-10 mg/dy Q6-8 hr 1/3-1/2 po dose = IM dose Initial dose (usual): 1.25mg Onset: ≤ 1hr Immediate Caution for doses > 10mg/dy Cmax: 1.5-2hr Release t½: 14.7-15.3hr 2.5mg/ml Duration Action: 6-8hr Elimination: Hepatic to inactive metabolites Hemodialysis: Not dialyzable Decanoate IM 12.5-50mg Q2-3 wks 10mg po = 12.5mg IM CONVERTING FROM PO TO LONG-ACTING DECANOATE: Onset: 24-72hr (4-72hr) Long-Acting SC (12.5-100mg) (1-4 wks) Round to nearest 12.5mg Method 1: 1.25 X po daily dose = equiv decanoate dose; admin Q2-3wks. Cont ½ po daily dose X 1st few mths Cmax: 48-96hr 25mg/ml Method 2: ↑ decanoate dose over 4wks & ↓ po dose over 4-8wks as follows (accelerate taper for sx of EPS): t½: 6.8-9.6dy (single dose) ORAL DECANOATE (Administer Q 2 weeks) 15dy (14-100dy chronic administration) ORAL DOSE (mg/dy) ↓ DOSE OVER (wks) INITIAL DOSE (mg) TARGET DOSE (mg) DOSE OVER (wks) Steady State: 2mth (1.5-3mth) 5 4 6.25 6.25 0 Duration Action: 2wk (1-6wk) Elimination: Hepatic to inactive metabolites 10 4 6.25 12.5 4 Hemodialysis: Not dialyzable 20 8 6.25 12.5 4 30 8 6.25 25 4 40 8 6.25 25 4 Method 3: Admin equivalent decanoate dose Q2-3wks. -

Drug Use Evaluation: Antipsychotic Utilization in Schizophrenia Patients
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35 Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 Drug Use Evaluation: Antipsychotic Utilization in Schizophrenia Patients Research Questions: 1. How many schizophrenia patients are prescribed recommended first-line second-generation treatments for schizophrenia? 2. How many schizophrenia patients switch to an injectable antipsychotic after stabilization on an oral antipsychotic? 3. How many schizophrenia patients are prescribed 2 or more concomitant antipsychotics? 4. Are claims for long-acting injectable antipsychotics primarily billed as pharmacy or physician administered claims? 5. Does adherence to antipsychotic therapy differ between patients with claims for different routes of administration (oral vs. long-acting injectable)? Conclusions: In total, 4663 schizophrenia patients met inclusion criteria, and approximately 14% of patients (n=685) were identified as treatment naïve without claims for antipsychotics in the year before their first antipsychotic prescription. Approximately 45% of patients identified as treatment naïve had a history of remote antipsychotic use, but it is unclear if antipsychotics were historically prescribed for schizophrenia. Oral second-generation antipsychotics which are recommended as first-line treatment in the MHCAG schizophrenia algorithm were prescribed as initial treatment in 37% of treatment naive patients and 28% of all schizophrenia patients. Recommended agents include risperidone, paliperidone, and aripiprazole. Utilization of parenteral antipsychotics was limited in patients with schizophrenia. Overall only 8% of patients switched from an oral to an injectable therapy within 6 months of their first claim. Approximately, 60% of all schizophrenia patients (n=2512) had claims for a single antipsychotic for at least 12 continuous weeks and may be eligible to transition to a long-acting injectable antipsychotic. -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -
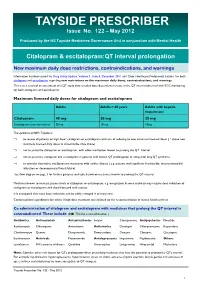
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -

Adverse Reactions to Hallucinogenic Drugs. 1Rnstttutton National Test
DOCUMENT RESUME ED 034 696 SE 007 743 AUTROP Meyer, Roger E. , Fd. TITLE Adverse Reactions to Hallucinogenic Drugs. 1rNSTTTUTTON National Test. of Mental Health (DHEW), Bethesda, Md. PUB DATP Sep 67 NOTE 118p.; Conference held at the National Institute of Mental Health, Chevy Chase, Maryland, September 29, 1967 AVATLABLE FROM Superintendent of Documents, Government Printing Office, Washington, D. C. 20402 ($1.25). FDPS PRICE FDPS Price MFc0.50 HC Not Available from EDRS. DESCPTPTOPS Conference Reports, *Drug Abuse, Health Education, *Lysergic Acid Diethylamide, *Medical Research, *Mental Health IDENTIFIEPS Hallucinogenic Drugs ABSTPACT This reports a conference of psychologists, psychiatrists, geneticists and others concerned with the biological and psychological effects of lysergic acid diethylamide and other hallucinogenic drugs. Clinical data are presented on adverse drug reactions. The difficulty of determining the causes of adverse reactions is discussed, as are different methods of therapy. Data are also presented on the psychological and physiolcgical effects of L.S.D. given as a treatment under controlled medical conditions. Possible genetic effects of L.S.D. and other drugs are discussed on the basis of data from laboratory animals and humans. Also discussed are needs for futher research. The necessity to aviod scare techniques in disseminating information about drugs is emphasized. An aprentlix includes seven background papers reprinted from professional journals, and a bibliography of current articles on the possible genetic effects of drugs. (EB) National Clearinghouse for Mental Health Information VA-w. Alb alb !bAm I.S. MOMS Of NAM MON tMAN IONE Of NMI 105 NUNN NU IN WINES UAWAS RCM NIN 01 NUN N ONMININI 01011110 0. -

NORPRAMIN® (Desipramine Hydrochloride Tablets USP)
NORPRAMIN® (desipramine hydrochloride tablets USP) Suicidality and Antidepressant Drugs Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of NORPRAMIN or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction in risk with antidepressants compared to placebo in adults aged 65 and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers should be advised of the need for close observation and communication with the prescriber. NORPRAMIN is not approved for use in pediatric patients. (See WARNINGS: Clinical Worsening and Suicide Risk, PRECAUTIONS: Information for Patients, and PRECAUTIONS: Pediatric Use.) DESCRIPTION NORPRAMIN® (desipramine hydrochloride USP) is an antidepressant drug of the tricyclic type, and is chemically: 5H-Dibenz[bƒ]azepine-5-propanamine,10,11-dihydro-N-methyl-, monohydrochloride. 1 Reference ID: 3536021 Inactive Ingredients The following inactive ingredients are contained in all dosage strengths: acacia, calcium carbonate, corn starch, D&C Red No. 30 and D&C Yellow No. 10 (except 10 mg and 150 mg), FD&C Blue No. 1 (except 25 mg, 75 mg, and 100 mg), hydrogenated soy oil, iron oxide, light mineral oil, magnesium stearate, mannitol, polyethylene glycol 8000, pregelatinized corn starch, sodium benzoate (except 150 mg), sucrose, talc, titanium dioxide, and other ingredients. -

PRODUCT MONOGRAPH ELAVIL® Amitriptyline Hydrochloride Tablets
PRODUCT MONOGRAPH ELAVIL® amitriptyline hydrochloride tablets USP 10, 25, 50 and 75 mg Antidepressant AA PHARMA INC. DATE OF PREPARATION: 1165 Creditstone Road Unit #1 August 29, 2018 Vaughan, ON L4K 4N7 Control No.: 217626 1 PRODUCT MONOGRAPH ELAVIL® amitriptyline hydrochloride tablets USP 10, 25, 50, 75 mg THERAPEUTIC CLASSIFICATION Antidepressant ACTIONS AND CLINICAL PHARMACOLOGY Amitriptyline hydrochloride is a tricyclic antidepressant with sedative properties. Its mechanism of action in man is not known. Amitriptyline inhibits the membrane pump mechanism responsible for the re-uptake of transmitter amines, such as norepinephrine and serotonin, thereby increasing their concentration at the synaptic clefts of the brain. Amitriptyline has pronounced anticholinergic properties and produces EKG changes and quinidine-like effects on the heart (See ADVERSE REACTIONS). It also lowers the convulsive threshold and causes alterations in EEG and sleep patterns. Orally administered amitriptyline is readily absorbed and rapidly metabolized. Steady-state plasma concentrations vary widely and this variation may be genetically determined. Amitriptyline is primarily excreted in the urine, mostly in the form of metabolites, with some excretion also occurring in the feces. INDICATIONS AND CLINICAL USE ELAVIL® (amitriptyline hydrochloride) is indicated in the drug management of depressive illness. ELAVIL® may be used in depressive illness of psychotic or endogenous nature and in selected patients with neurotic depression. Endogenous depression is more likely to be alleviated than are other depressive states. ELAVIL® ®, because of its sedative action, is also of value in alleviating the anxiety component of depression. As with other tricyclic antidepressants, ELAVIL® may precipitate hypomanic episodes in patients with bipolar depression. These drugs are not indicated in mild depressive states and depressive reactions. -

Management of Major Depressive Disorder Clinical Practice Guidelines May 2014
Federal Bureau of Prisons Management of Major Depressive Disorder Clinical Practice Guidelines May 2014 Table of Contents 1. Purpose ............................................................................................................................................. 1 2. Introduction ...................................................................................................................................... 1 Natural History ................................................................................................................................. 2 Special Considerations ...................................................................................................................... 2 3. Screening ........................................................................................................................................... 3 Screening Questions .......................................................................................................................... 3 Further Screening Methods................................................................................................................ 4 4. Diagnosis ........................................................................................................................................... 4 Depression: Three Levels of Severity ............................................................................................... 4 Clinical Interview and Documentation of Risk Assessment............................................................... -
Neuroprotection by Chlorpromazine and Promethazine in Severe Transient and Permanent Ischemic Stroke
Mol Neurobiol (2017) 54:8140–8150 DOI 10.1007/s12035-016-0280-x Neuroprotection by Chlorpromazine and Promethazine in Severe Transient and Permanent Ischemic Stroke Xiaokun Geng1,2 & Fengwu Li1 & James Yip2 & Changya Peng2 & Omar Elmadhoun2 & Jiamei Shen1 & Xunming Ji1,3 & Yuchuan Ding1,2 Received: 29 June 2016 /Accepted: 31 October 2016 /Published online: 28 November 2016 # Springer Science+Business Media New York 2016 Abstract Previous studies have demonstrated depressive or enhance C + P-induced neuroprotection. C + P therapy im- hibernation-like roles of phenothiazine neuroleptics [com- proved brain metabolism as determined by increased ATP bined chlorpromazine and promethazine (C + P)] in brain levels and NADH activity, as well as decreased ROS produc- activity. This ischemic stroke study aimed to establish neuro- tion. These therapeutic effects were associated with alterations protection by reducing oxidative stress and improving brain in PKC-δ and Akt protein expression. C + P treatments con- metabolism with post-ischemic C + P administration. ferred neuroprotection in severe stroke models by suppressing Sprague-Dawley rats were subjected to transient (2 or 4 h) the damaging cascade of metabolic events, most likely inde- middle cerebral artery occlusion (MCAO) followed by 6 or pendent of drug-induced hypothermia. These findings further 24 h reperfusion, or permanent (28 h) MCAO without reper- prove the clinical potential for C + P treatment and may direct fusion. At 2 h after ischemia onset, rats received either an us closer towards the development of an efficacious neuropro- intraperitoneal (IP) injection of saline or two doses of C + P. tective therapy. Body temperatures, brain infarct volumes, and neurological deficits were examined. -

Is Aristada (Aripiprazole Lauroxil) a Safe and Effective Treatment for Schizophrenia in Adult Patients? Kyle J
Philadelphia College of Osteopathic Medicine DigitalCommons@PCOM PCOM Physician Assistant Studies Student Student Dissertations, Theses and Papers Scholarship 2017 Is Aristada (Aripiprazole Lauroxil) a Safe and Effective Treatment For Schizophrenia In Adult Patients? Kyle J. Knowles Philadelphia College of Osteopathic Medicine Follow this and additional works at: https://digitalcommons.pcom.edu/pa_systematic_reviews Part of the Psychiatry Commons Recommended Citation Knowles, Kyle J., "Is Aristada (Aripiprazole Lauroxil) a Safe and Effective Treatment For Schizophrenia In Adult Patients?" (2017). PCOM Physician Assistant Studies Student Scholarship. 381. https://digitalcommons.pcom.edu/pa_systematic_reviews/381 This Selective Evidence-Based Medicine Review is brought to you for free and open access by the Student Dissertations, Theses and Papers at DigitalCommons@PCOM. It has been accepted for inclusion in PCOM Physician Assistant Studies Student Scholarship by an authorized administrator of DigitalCommons@PCOM. For more information, please contact [email protected]. Is Aristada (Aripiprazole Lauroxil) a Safe and Effective Treatment For Schizophrenia In Adult Patients? Kyle J. Knowles, PA-S A SELECTIVE EVIDENCE BASED MEDICINE REVIEW In Partial Fulfillment of the Requirements For The Degree of Master of Science In Health Sciences- Physician Assistant Department of Physician Assistant Studies Philadelphia College of Osteopathic Medicine Philadelphia, Pennsylvania December 16, 2016 ABSTRACT OBJECTIVE: The objective of this selective EBM review is to determine whether or not “Is Aristada (aripiprazole lauroxil) a safe and effective treatment for schizophrenia in adult patients?” STUDY DESIGN: Review of three randomized controlled studies. All three trials were conducted between 2014 and 2015. DATA SOURCES: One randomized, controlled trial and two randomized, controlled, double- blind trials found via Cochrane Library and PubMed.