EMERGING INFECTIOUS DISEASES Volume 5 Number 1 JanuaryFebruary 1999
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hantavirus Disease Were HPS Is More Common in Late Spring and Early Summer in Seropositive in One Study in the U.K
Hantavirus Importance Hantaviruses are a large group of viruses that circulate asymptomatically in Disease rodents, insectivores and bats, but sometimes cause illnesses in humans. Some of these agents can occur in laboratory rodents or pet rats. Clinical cases in humans vary in Hantavirus Fever, severity: some hantaviruses tend to cause mild disease, typically with complete recovery; others frequently cause serious illnesses with case fatality rates of 30% or Hemorrhagic Fever with Renal higher. Hantavirus infections in people are fairly common in parts of Asia, Europe and Syndrome (HFRS), Nephropathia South America, but they seem to be less frequent in North America. Hantaviruses may Epidemica (NE), Hantavirus occasionally infect animals other than their usual hosts; however, there is currently no Pulmonary Syndrome (HPS), evidence that they cause any illnesses in these animals, with the possible exception of Hantavirus Cardiopulmonary nonhuman primates. Syndrome, Hemorrhagic Nephrosonephritis, Epidemic Etiology Hemorrhagic Fever, Korean Hantaviruses are members of the genus Orthohantavirus in the family Hantaviridae Hemorrhagic Fever and order Bunyavirales. As of 2017, 41 species of hantaviruses had officially accepted names, but there is ongoing debate about which viruses should be considered discrete species, and additional viruses have been discovered but not yet classified. Different Last Updated: September 2018 viruses tend to be associated with the two major clinical syndromes in humans, hemorrhagic fever with renal syndrome (HFRS) and hantavirus pulmonary (or cardiopulmonary) syndrome (HPS). However, this distinction is not absolute: viruses that are usually associated with HFRS have been infrequently linked to HPS and vice versa. A mild form of HFRS in Europe is commonly called nephropathia epidemica. -

A Newly Identified Hantavirus: the Development of Immunologic Diagnostic Assays and Phylogenetic Analysis for Detection and Characterization
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Doctoral Dissertations Graduate School 12-2005 A Newly Identified Hantavirus: The Development of Immunologic Diagnostic Assays and Phylogenetic Analysis for Detection and Characterization Shawn Lee Lewis University of Tennessee, Knoxville Follow this and additional works at: https://trace.tennessee.edu/utk_graddiss Part of the Medicine and Health Sciences Commons Recommended Citation Lewis, Shawn Lee, "A Newly Identified Hantavirus: The Development of Immunologic Diagnostic Assays and Phylogenetic Analysis for Detection and Characterization. " PhD diss., University of Tennessee, 2005. https://trace.tennessee.edu/utk_graddiss/4368 This Dissertation is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Doctoral Dissertations by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a dissertation written by Shawn Lee Lewis entitled "A Newly Identified Hantavirus: The Development of Immunologic Diagnostic Assays and Phylogenetic Analysis for Detection and Characterization." I have examined the final electronic copy of this dissertation for form and content and recommend that it be accepted in partial fulfillment of the equirr ements for the degree of Doctor of Philosophy, with a major in Comparative and Experimental Medicine. John -

Virus Hébergés Par Les Rongeurs En Guyane Française Anne Lavergne, Séverine Matheus, Francois Catzeflis, Damien Donato, Vincent Lacoste, Benoît De Thoisy
Virus hébergés par les rongeurs en Guyane française Anne Lavergne, Séverine Matheus, Francois Catzeflis, Damien Donato, Vincent Lacoste, Benoît de Thoisy To cite this version: Anne Lavergne, Séverine Matheus, Francois Catzeflis, Damien Donato, Vincent Lacoste, et al.. Virus hébergés par les rongeurs en Guyane française. Virologie, John Libbey Eurotext 2017, 21 (3), pp.130- 146. 10.1684/vir.2017.0698. hal-01836325 HAL Id: hal-01836325 https://hal.umontpellier.fr/hal-01836325 Submitted on 31 Jan 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Virus hébergés par les rongeurs en Guyane franc¸aise Anne Lavergne1 Résumé. Les rongeurs sont décrits comme des réservoirs privilégiés de nom- Séverine Matheus2 breuses zoonoses. Du fait de leur forte abondance, de leur dynamique et, pour Franc¸ois Catzeflis3 plusieurs espèces, de leur capacité à coexister avec les populations humaines, les 1 rongeurs jouent un rôle clé dans le maintien et la transmission de pathogènes. En Damien Donato Guyane, 36 espèces de rongeurs ont été recensées et sont présentes aussi bien en Vincent Lacoste1 forêt primaire et secondaire qu’en savane et en zones urbaines. Certaines popu- Benoit de Thoisy1 lations de rongeurs font face, aujourd’hui, à des perturbations de leurs habitats, 1 Laboratoire des interactions du fait des pressions anthropiques. -
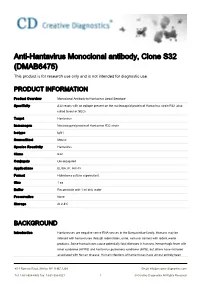
Anti-Hantavirus Monoclonal Antibody, Clone S32 (DMAB6475) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-Hantavirus Monoclonal antibody, Clone S32 (DMAB6475) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Monoclonal Antibody to Hantavirus Seoul Serotype Specificity S32 reacts with an epitope present on the nucleocapsid protein of Hantavirus strain R22 (also called Seoul or SEO) Target Hantavirus Immunogen Nucleocapsid protein of Hantavirus R22 strain Isotype IgG1 Source/Host Mouse Species Reactivity Hantavirus Clone S32 Conjugate Unconjugated Applications ELISA, IF, IHC-Fr Format Hybridoma culture supernatant Size 1 ea Buffer Reconstitute with 1 ml dist. water Preservative None Storage At 2-8℃ BACKGROUND Introduction Hantaviruses are negative sense RNA viruses in the Bunyaviridae family. Humans may be infected with hantaviruses through rodent bites, urine, saliva or contact with rodent waste products. Some hantaviruses cause potentially fatal diseases in humans, hemorrhagic fever with renal syndrome (HFRS) and hantavirus pulmonary syndrome (HPS), but others have not been associated with human disease. Human infections of hantaviruses have almost entirely been 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved linked to human contact with rodent excrement, but recent human-to-human transmission has been reported with the Andes virus in South America. The name hantavirus is derived from the Hantan River area in South Korea, which provided the founding member of the group: Hantaan virus (HTNV), isolated in the late 1970s by Ho-Wang Lee and colleagues. HTNV is one of several hantaviruses that cause HFRS, formerly known as Korean hemorrhagic fever. -

Hantavirus Infection: a Global Zoonotic Challenge
VIROLOGICA SINICA DOI: 10.1007/s12250-016-3899-x REVIEW Hantavirus infection: a global zoonotic challenge Hong Jiang1#, Xuyang Zheng1#, Limei Wang2, Hong Du1, Pingzhong Wang1*, Xuefan Bai1* 1. Center for Infectious Diseases, Tangdu Hospital, Fourth Military Medical University, Xi’an 710032, China 2. Department of Microbiology, School of Basic Medicine, Fourth Military Medical University, Xi’an 710032, China Hantaviruses are comprised of tri-segmented negative sense single-stranded RNA, and are members of the Bunyaviridae family. Hantaviruses are distributed worldwide and are important zoonotic pathogens that can have severe adverse effects in humans. They are naturally maintained in specific reservoir hosts without inducing symptomatic infection. In humans, however, hantaviruses often cause two acute febrile diseases, hemorrhagic fever with renal syndrome (HFRS) and hantavirus cardiopulmonary syndrome (HCPS). In this paper, we review the epidemiology and epizootiology of hantavirus infections worldwide. KEYWORDS hantavirus; Bunyaviridae, zoonosis; hemorrhagic fever with renal syndrome; hantavirus cardiopulmonary syndrome INTRODUCTION syndrome (HFRS) and HCPS (Wang et al., 2012). Ac- cording to the latest data, it is estimated that more than Hantaviruses are members of the Bunyaviridae family 20,000 cases of hantavirus disease occur every year that are distributed worldwide. Hantaviruses are main- globally, with the majority occurring in Asia. Neverthe- tained in the environment via persistent infection in their less, the number of cases in the Americas and Europe is hosts. Humans can become infected with hantaviruses steadily increasing. In addition to the pathogenic hanta- through the inhalation of aerosols contaminated with the viruses, several other members of the genus have not virus concealed in the excreta, saliva, and urine of infec- been associated with human illness. -

Zoonotic Potential of International Trade in CITES-Listed Species Annexes B, C and D JNCC Report No
Zoonotic potential of international trade in CITES-listed species Annexes B, C and D JNCC Report No. 678 Zoonotic potential of international trade in CITES-listed species Annex B: Taxonomic orders and associated zoonotic diseases Annex C: CITES-listed species and directly associated zoonotic diseases Annex D: Full trade summaries by taxonomic family UNEP-WCMC & JNCC May 2021 © JNCC, Peterborough 2021 Zoonotic potential of international trade in CITES-listed species Prepared for JNCC Published May 2021 Copyright JNCC, Peterborough 2021 Citation UNEP-WCMC and JNCC, 2021. Zoonotic potential of international trade in CITES- listed species. JNCC Report No. 678, JNCC, Peterborough, ISSN 0963-8091. Contributing authors Stafford, C., Pavitt, A., Vitale, J., Blömer, N., McLardy, C., Phillips, K., Scholz, L., Littlewood, A.H.L, Fleming, L.V. & Malsch, K. Acknowledgements We are grateful for the constructive comments and input from Jules McAlpine (JNCC), Becky Austin (JNCC), Neville Ash (UNEP-WCMC) and Doreen Robinson (UNEP). We also thank colleagues from OIE for their expert input and review in relation to the zoonotic disease dataset. Cover Photographs Adobe Stock images ISSN 0963-8091 JNCC Report No. 678: Zoonotic potential of international trade in CITES-listed species Annex B: Taxonomic orders and associated zoonotic diseases Annex B: Taxonomic orders and associated zoonotic diseases Table B1: Taxonomic orders1 associated with at least one zoonotic disease according to the source papers, ranked by number of associated zoonotic diseases identified. -

Disparity in Sin Nombre Virus Antibody Reactivity Between Neighboring Mojave Desert Communities
VECTOR-BORNE AND ZOONOTIC DISEASES Volume XX, Number XX, 2018 ª Mary Ann Liebert, Inc. DOI: 10.1089/vbz.2018.2341 A Tale of Two Valleys: Disparity in Sin Nombre Virus Antibody Reactivity Between Neighboring Mojave Desert Communities Risa Pesapane,1 Barryett Enge,2,* Austin Roy,3,{ Rebecca Kelley,4 Karen Mabry,4 Brian C. Trainor,5 Deana Clifford,3 and Janet Foley1 Abstract Introduction: Hantaviruses are a group of globally distributed rodent-associated viruses, some of which are responsible for human morbidity and mortality. Sin Nombre orthohantavirus, a particularly virulent species of hantavirus associated with Peromyscus spp. mice, is actively monitored by the Department of Public Health in California (CDPH). Recently, CDPH documented high (40%) seroprevalence in a potentially novel reservoir species, the cactus mouse (Peromyscus eremicus) in Death Valley National Park. Methods: This study was performed in the extremely isolated Mojave Desert Amargosa River valley region of southeastern Inyo County, California, 105 km from Death Valley, approximately over the same time interval as the CDPH work in Death Valley (between 2011 and 2016). Similar rodent species were captured as in Death Valley and were tested for select hantaviruses using serology and RT-PCR to assess risk to human health and the conservation of the endemic endangered Amargosa vole. Results: Among 192 rodents tested, including 56 Peromyscus spp., only one seropositive harvest mouse (Reithro- dontomys megalotis) was detected. Discussion: These data highlight the heterogeneity in the prevalence of hantavirus infection even among nearby desert communities and suggest that further studies of hantavirus persistence in desert environments are needed to more accurately inform the risks to public health and wildlife conservation. -

Disparity in Sin Nombre Virus Antibody Reactivity Between Neighboring Mojave Desert Communities
VECTOR-BORNE AND ZOONOTIC DISEASES Volume XX, Number XX, 2018 ª Mary Ann Liebert, Inc. DOI: 10.1089/vbz.2018.2341 A Tale of Two Valleys: Disparity in Sin Nombre Virus Antibody Reactivity Between Neighboring Mojave Desert Communities Risa Pesapane,1 Barryett Enge,2,* Austin Roy,3,{ Rebecca Kelley,4 Karen Mabry,4 Brian C. Trainor,5 Deana Clifford,3 and Janet Foley1 Abstract Introduction: Hantaviruses are a group of globally distributed rodent-associated viruses, some of which are responsible for human morbidity and mortality. Sin Nombre orthohantavirus, a particularly virulent species of hantavirus associated with Peromyscus spp. mice, is actively monitored by the Department of Public Health in California (CDPH). Recently, CDPH documented high (40%) seroprevalence in a potentially novel reservoir species, the cactus mouse (Peromyscus eremicus) in Death Valley National Park. Methods: This study was performed in the extremely isolated Mojave Desert Amargosa River valley region of southeastern Inyo County, California, 105 km from Death Valley, approximately over the same time interval as the CDPH work in Death Valley (between 2011 and 2016). Similar rodent species were captured as in Death Valley and were tested for select hantaviruses using serology and RT-PCR to assess risk to human health and the conservation of the endemic endangered Amargosa vole. Results: Among 192 rodents tested, including 56 Peromyscus spp., only one seropositive harvest mouse (Reithro- dontomys megalotis) was detected. Discussion: These data highlight the heterogeneity in the prevalence of hantavirus infection even among nearby desert communities and suggest that further studies of hantavirus persistence in desert environments are needed to more accurately inform the risks to public health and wildlife conservation. -

Microtus Oeconomus) in Lithuania, Eastern Europe
Infection, Genetics and Evolution 90 (2021) 104520 Contents lists available at ScienceDirect Infection, Genetics and Evolution journal homepage: www.elsevier.com/locate/meegid Research Paper Identification of a novel hantavirus strain in the root vole (Microtus oeconomus) in Lithuania, Eastern Europe Stephan Drewes a,1, Kathrin Jeske a,b,1, Petra Strakova´ a,c, Linas Balˇciauskas d, Ren´e Ryll a, Laima Balˇciauskiene_ d, David Kohlhause a,e, Guy-Alain Schnidrig f, Melanie Hiltbrunner f, ˇ g g g f Aliona Spakova , Rasa Insodaite_ , Rasa Petraityte-Burneikien_ e_ , Gerald Heckel , Rainer G. Ulrich a,* a Institute of Novel and Emerging Infectious Diseases, Friedrich-Loeffler-Institut,Federal Research Institute for Animal Health, Südufer 10, 17493 Greifswald-Insel Riems, Germany b Institute of Diagnostic Virology, Friedrich-Loeffler-Institut, Federal Research Institute for Animal Health, Südufer 10, 17493 Greifswald-Insel Riems, Germany c Department of Virology, Veterinary Research Institute, Hudcova 70, 62100 Brno, Czech Republic d Nature Research Centre, Akademijos 2, LT-08412 Vilnius, Lithuania e University Greifswald, Domstraße 11, 17498 Greifswald, Germany f Institute of Ecology and Evolution, University of Bern, Baltzerstrasse 6, 3012 Bern, Switzerland g Institute of Biotechnology, Life Sciences Center, Vilnius University, Sauletekio_ al. 7, LT-10257 Vilnius, Lithuania ARTICLE INFO ABSTRACT Keywords: Hantaviruses are zoonotic pathogens that can cause subclinical to lethal infections in humans. In Europe, five Microtus oeconomus orthohantaviruses are present in rodents: Myodes-associated Puumala orthohantavirus (PUUV), Microtus-asso Lithuania ciated Tula orthohantavirus, Traemmersee hantavirus (TRAV)/ Tatenale hantavirus (TATV)/ Kielder hantavirus, Reservoir host rat-borne Seoul orthohantavirus, and Apodemus-associated Dobrava-Belgrade orthohantavirus (DOBV). Human Tatenale hantavirus PUUV and DOBV infections were detected previously in Lithuania, but the presence of Microtus-associated Traemmersee hantavirus Rusne hantavirus hantaviruses is not known. -

Hantaviruses: an Overview
Comparative Medicine Vol 52, No 2 Copyright 2002 April 2002 by the American Association for Laboratory Animal Science Pages 97-110 Overview Hantaviruses: An Overview Joe H. Simmons, DVM, PhD and Lela K. Riley, PhD Hantaviruses are a newly emerging group of rodent-borne viruses that have significant zoonotic potential. Hu- man infection by hantaviruses can result in profound morbidity and mortality, with death rates as high as 50%, and potentially long-term cardiovascular consequences. Hantaviruses are carried by peridomestic and wild rodents worldwide and have occasionally been linked to infections in laboratory rodents. Because these viruses have been associated with significant human disease, they have become the subject of intense scientific investigation. In this review the reader is introduced to the hantaviruses, including hantavirus diseases and their pathogenesis. A re- view of the biology, morphology, and molecular biology of the hantaviruses with a brief overview of the ecology and biology of hantavirus-rodent pairs is also included. The risks of occupational exposure to hantaviruses, diagnosis of hantavirus infections, and methods for handling potentially infected rodents and tissues are discussed as well. Introduction cluding Hantaan virus (HTNV), Seoul virus (SEOV), Puumala The genus Hantavirus belongs to the family Bunyaviridae; virus (PUUV), and Dobrava virus (DOBV), infect humans, they other genera in the family include Bunyavirus, Nairovirus, typically affect the urinary system and cause a disease syn- Phlebovirus, and Tospovirus. All of the members of the family are drome known as hemorrhagic fever with renal syndrome enveloped, with tri-segmented, negative sense RNA genomes. (HFRS). A more recently described hantavirus disease emerged Bunyaviruses, Nairoviruses, Phleboviruses, and Tospoviruses are in the New World in May 1993 when a cluster of deaths oc- classical arboviruses in that they are all transmitted through curred in the Four Corners area of the U.S. -

The Ecology of New World Rodent Borne Hemorrhagic Fevers
THE ECOLOGY OF NEW WORLD RODENT BORNE HEMORRHAGIC FEVERS DARJN S. CARROLL , Centers for Disease Control and Prevention , National Centers for Infectious Diseases , Special Pathogens Branch , Atlanta , GA 30333 , USA EMILY JENTES , Centers for Disease Control and Prevention , National Centers for Infectious Diseases , Special Pathogens Branch , Atlanta , GA 30333, USA JAMES N. MILLS , Centers for Disease Control and Prevention , National Centers for Infectious Diseases, Special Pathogens Branch , Atlanta , GA 30333 , USA Abstract: Few, if any, human settlements are free of peridomestic rodent populations. The threat of rodent borne zoonotic diseases has been widely recognized since the bubonic plague outbreaks of the Middle Ages . In the last decades, outbreaks of human disease caused by the rodent borne hemorrhagic fever viruses , the arenaviruses (family Arenaviridae), and the hantaviruses (family Bunyaviridae, genus Hantaviru s) have again generated interest in the general public and scientific community regarding the biology of these types of diseases. Recent studie s have identified more than 30 new members of these two groups of viruses. Most are associated with rodents in the family Muridae and many are known to be pathogenic. Ongoing studies are investigating aspects of the ecology and systematics of these viruses and their reservoirs . Ecological studies are currently examining modes of transmission between members of the host species , and environmental factors associated with increased frequency of infection. Systematic research is identifying patterns of co-evolution between the viruses and their hosts. The overall goal of these research efforts is develop predictive models that will identify times and places of increased risk and. therefore provide an opportunity for risk reduction in these areas. -

The Role of Animals in Emerging Viral Diseases
The Role of Animals in Emerging Viral Diseases Edited by Nicholas Johnson AMSTERDAM • BOSTON • HEIDELBERG • LONDON NEW YORK • OXFORD • PARIS • SAN DIEGO SAN FRANCISCO • SINGAPORE • SYDNEY • TOKYO Academic Press is an Imprint of Elsevier Academic Press is an imprint of Elsevier 525 B Street, Suite 1900, San Diego, CA 92101-4495, USA 32 Jamestown Road, London NW1 7BY, UK 225 Wyman Street, Waltham, MA 02451, USA Copyright © 2014 Elsevier Inc. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means electronic, mechanical, photocopying, recording or otherwise without the prior written permission of the publisher. Permissions may be sought directly from Elsevier’s Science & Technology Rights, Department in Oxford, UK: phone (+44) (0) 1865 843830; fax (+44) (0) 1865 853333; email: [email protected]. Alternatively, visit the Science and Technology Books website at www.elsevierdirect.com/rights for further information. Notice No responsibility is assumed by the publisher for any injury and/or damage to persons, or property as a matter of products liability, negligence or otherwise, or from any use or, operation of any methods, products, instructions or ideas contained in the material herein. Because of rapid advances in the medical sciences, in particular, independent verification of diagnoses and drug dosages should be made. British Library Cataloguing-in-Publication Data A catalog record for this book is available from the British Library. Library of Congress Cataloging-in-Publication Data A catalog record for this book is available from the Library of Congress. ISBN: 978-0-12-405191-1 For information on all Academic Press publications visit our website at elsevierdirect.com Typeset by TNQ Books and Journals www.tnq.co.in Printed and bound in China 14 15 16 17 18 10 9 8 7 6 5 4 3 2 1 Dedication This book is dedicated to Clive and Jean for a lifetime of support Contributors Andrew B.