NHS North Lincolnshire Clinical Commissioning Group 2014-15
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

LEICESTER - Loughborough - EAST MIDLANDS AIRPORT - DERBY
LEICESTER - Loughborough - EAST MIDLANDS AIRPORT - DERBY Mondays to Fridays pm am am am am am am am am am am am am am am am am am am pm pm pm pm pm pm LEICESTER Gravel Street Stop Z1 11.55 12.55 1.55 2.55 3.55 - 4.55 - - - - - - - - - - - - - - - - - - - - - LEICESTER St Margarets Bus Stn - - - - - - - - - - 5.55 - 6.25 6.45 7.05 7.25 7.45 8.05 8.30 50 10 30 4.10 4.30 4.50 5.10 5.30 5.50 LOUGHBOROUGH High Street arr 12.20 1.20 2.20 3.20 4.20 - 5.20 - - - 6.17 - 6.53 7.13 7.33 7.58 8.18 8.38 8.58 18 38 58 4.38 4.58 5.18 5.43 6.03 6.18 LOUGHBOROUGH High Street dep 12.20 1.20 2.20 3.20 4.20 4.50 5.20 5.40 5.55 6.10 6.19 6.39 6.54 7.14 7.34 7.59 8.19 8.39 8.59 19 39 59 4.39 4.59 5.19 5.44 6.04 6.19 Hathern opp Anchor Inn 12.32 1.32 2.32 3.32 4.32 5.02 5.32 5.52 6.07 6.22 6.28 6.48 7.03 7.23 7.43 8.08 8.28 8.48 9.08 then 28 48 08 4.48 5.08 5.33 5.58 6.18 6.28 Long Whatton Piper Drive l l l l l l l l l l 6.32 l l 7.27 l l 8.32 l l at 32 l l l l 5.37 l l 6.32 Diseworth opp Bull & Swan l l l l l l l l l l 6.38 l l 7.33 l l 8.38 l l these 38 l l l l 5.43 l l 6.38 Kegworth Square 12.38 1.38 2.38 3.38 4.38 5.08 5.38 5.58 6.13 6.28 l 6.54 7.09 l 7.49 8.14 l 8.54 9.14 mins l 54 14 4.54 5.14 l 6.04 6.24 l Pegasus Business Park 12.42 1.42 2.42 3.42 4.42 5.12 5.42 6.02 6.17 6.32 6.41 7.01 7.16 7.36 7.56 8.21 8.41 9.01 9.21 past 41 01 21 until 5.01 5.21 5.46 6.11 6.31 6.41 EAST MIDLANDS AIRPORT arr 12.45 1.45 2.45 3.45 4.45 5.15 5.45 6.05 6.20 6.35 6.44 7.04 7.19 7.39 7.59 8.24 8.44 9.04 9.24 each 44 04 24 5.04 5.24 5.49 6.14 6.34 6.44 EAST MIDLANDS AIRPORT -

Borough Profile 2020 Warrington
Borough profile 2020 Warrington 6 4 3 117 122 118 115 9 5 19 120 7 Warrington Wards 2 13 1 1. Appleton 12. Latchford West 110 11 12 2. Bewsey & Whitecross 13. Lymm North & Thelwall 1 14 3. Birchwood 14. Lymm South 4. Burtonwood & Winwick 15. Orford 116 21 5. Chapelford & Old Hall 16. Penketh & Cuerdley 8 6. Culcheth, Glazebury & Croft 17. Poplars & Hulme 7. Fairfield & Howley 18. Poulton North 8. Grappenhall 19. Poulton South 1 9. Great Sankey North & Whittle Hall 20. Rixton & Woolston 10. Great Sankey South 21. Stockton Heath 11. Latchford East 22. Westbrook Produced by Business Intelligence Service Back to top Contents 1. Population of Warrington 2. Deprivation 3. Education - Free School Meals (FSM) 4. Education - Special Educational Needs (SEN) 5. Education - Black Minority Ethnic (BME) 6. Education - English as an Additional Language (EAL) 7. Education - (Early Years aged 4/5) - Early Years Foundation Stage: Good Level of Development (GLD) 8. Education - (End of primary school aged 10/11) – Key Stage 2: Reading, Writing and Maths 9. Education (end of secondary school aged 15/16) – Key Stage 4: Progress 8 10. Education (end of secondary school aged 15/16) – Key Stage 4: Attainment 8 11. Health - Life expectancy 12. Health - Low Birthweight 13. Health - Smoking at time of delivery 14. Health - Overweight and obese reception children 15. Health - Overweight and obese Year 6 children 16. Children’s Social Care – Children in Need 17. Adult Social Care – Request for Support from new clients 18. Adult Social Care – Sequel to the Requests for Support 19. Adult Social Care – Number of clients accessing Long Term Support 20. -

87 York Road Brigg North Lincolnshire DN20 8DX Asking Price
The Largest Independent Auction, Estate & Letting Agency in the Region 87 York Road Brigg North Lincolnshire DN20 8DX . Good sized family home in popular location . Lounge with sun room off . Breakfast kitchen & utility . Four bedrooms & bathroom . Off road parking & garage . EPC RATING : D Asking Price: £159,000 Further information and viewings: DDM Residential - Brigg Office - 01652 653666 DESCRIPTION A four bedroom detached family home situated in a popular residential area of Brigg with easy access to the town centre and local schools. The property is decorated to a high standard throughout and briefly comprises entrance hall, lounge with sun room off, breakfast kitchen, utility and cloakroom. To the first floor there are four bedrooms and a family bathroom. Having off road parking, garage and gardens to the front and rear. A good sized family home in excellent location. ACCOMMODATION ENTRANCE HALL uPVC double glazed entrance door, cornice to ceiling, uPVC double glazed window to the front aspect, radiator, stairs to first floor. SITTING ROOM 15' 1'' x 11' 5'' (4.59m x 3.49m) Cornice to ceiling, uPVC double glazed bay window to the front aspect, traditional style painted fire surround with tiled inset and hearth to flame effect electric fire, radiator. SUN ROOM/DINING AREA 14' 0'' x 8' 3'' (4.26m x 2.51m) Cornice to ceiling, uPVC double glazed windows and roof, combination heater/air conditioning unit, tiled floor and uPVC double glazed French doors to the rear garden. BREAKFAST KITCHEN 15' 0'' x 11' 5'' (4.58m x 3.48m) Inset ceiling spot lights, uPVC double glazed windows to the front and rear aspects, range of base and wall mounted units with contrasting beech effect work surfaces, inset one and a half bowl composite sink and drainer with mixer tap, integrated dishwasher and fridge freezer, tiled splashback, black ash effect flooring, archway to: REAR LOBBY Understairs storage cupboard, radiator, black ash effect flooring. -

Leicester Area Strategic Advice 2020
How can growth and partners’ aspirations be accommodated in the Leicester area over the coming decades? Leicester Area Strategic Advice July 2020 02 Contents 01: Foreword 03 02: Executive Summary 04 03: Continuous Modular Strategic Planning 07 04: Leicester Area Strategic Context 08 05: Delivering Additional Future Services 12 06: Leicester Area Capacity 16 07: Accommodating Future Services 22 08: Recommendations and Next Steps 27 Photo credits: Front cover - lower left: Jeff Chapman Front cover - lower right: Jamie Squibbs Leicester Area Strategic Advice July 2020 03 01 Foreword The Leicester Area Strategic Advice forms part of the The report was produced collaboratively with inputs railway industry’s Long-Term Planning Process covering from key, interested organisations and considers the the medium-term and long-term planning horizon. impact of planned major programmes such as High Investment in the railway is an aid to long-term Speed 2 (HS2), and the strategies and aspirations of sustainable growth for the Leicester area, supporting bodies such as Leicester City Council, the Department economic, social and environmental objectives. of Transport (DfT), Midlands Connect and the Train Network Rail has worked collaboratively with rail and Freight Operating Companies. industry stakeholders and partners to develop long- The recommendations from this report support term plans for a safe, reliable and efficient railway to Network Rail’s focus of putting passengers first by support economic growth across Britain. aiming to increase the number of direct services from This study has considered the impact of increased Leicester Station, supporting freight growth and demand for passenger services in the medium and improving performance and satisfaction with the rail long term, starting from a baseline of today’s railway, network. -
Changes in the Ethnic Diversity of the Christian Population in England
National Census 2001 and 2011 Changes in the Ethnic Diversity of the Christian Population in England between 2001 and 2011 East Midlands Region Council for Christian Unity 2014 CONTENTS Foreword from the Chair of the Council for Christian Unity Page 1 Summary and Headlines Page 2 Introduction Page 2 Christian Ethnicity - Comparison of 2001 and 2011 Census Data Page 5 In England Page 5 By region Page 8 Overall trends Page 24 Analysis of Regional data by local authority Page 27 Introduction Page 27 Tables and Figures Page 28 Annex 2 Muslim Ethnicity in England Page 52 Census 2001/2011 East Midlands CCU(14)C3 Changes in the Ethnic Diversity of the Christian Population in England between 2001 and 2011 Foreword from the Chair of the Council for Christian Unity There are great ecumenical, evangelistic, pastoral and missional challenges presented to all the Churches by the increasing diversity of Christianity in England. The comparison of Census data from 2001 and 2011about the ethnic diversity of the Christian population, which is set out in this report, is one element of the work the Council for Christian Unity is doing with a variety of partners in this area. We are very pleased to be working with the Research and Statistics Department and the Committee for Minority Ethnic Anglican Affairs at Church House, and with Churches Together in England on a number of fronts. We hope that the set of eight reports, for each of the eight regions of England, will be a helpful resource for Church Leaders, Dioceses, Districts and Synods, Intermediate Ecumenical Bodies and local churches. -
Comparison of Overview and Scrutiny Functions at Similarly Sized Unitary Authorities
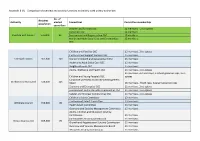
Appendix B (4) – Comparison of overview and scrutiny functions at similarly sized unitary authorities No. of Resident Authority elected Committees Committee membership population councillors Children and Families OSC 12 members + 2 co-optees Corporate OSC 12 members Cheshire East Council 378,800 82 Environment and Regeneration OSC 12 members Health and Adult Social Care and Communities 15 members OSC Children and Families OSC 15 members, 2 co-optees Customer and Support Services OSC 15 members Cornwall Council 561,300 123 Economic Growth and Development OSC 15 members Health and Adult Social Care OSC 15 members Neighbourhoods OSC 15 members Adults, Wellbeing and Health OSC 21 members, 2 co-optees 21 members, 4 church reps, 3 school governor reps, 2 co- Children and Young People's OSC optees Corporate Overview and Scrutiny Management Durham County Council 523,000 126 Board 26 members, 4 faith reps, 3 parent governor reps Economy and Enterprise OSC 21 members, 2 co-optees Environment and Sustainable Communities OSC 21 members, 2 co-optees Safeter and Stronger Communities OSC 21 members, 2 co-optees Children's Select Committee 13 members Environment Select Committee 13 members Wiltshere Council 496,000 98 Health Select Committee 13 members Overview and Scrutiny Management Committee 15 members Adults, Children and Education Scrutiny Commission 11 members Communities Scrutiny Commission 11 members Bristol City Council 459,300 70 Growth and Regeneration Scrutiny Commission 11 members Overview and Scrutiny Management Board 11 members Resources -

Income, Skills and Deprivation in Leicester and Nottingham
Institute for Applied Economics and Social Value East Midlands Economic Data Repository Short Report 21-02 Income, Skills and Deprivation in Leicester and Nottingham Data for this report is available at If citing this work please use: Cartwright, E., T. Luong and Al. Orazgani (2021) ‘Income, skills and deprivation in Leicester and Nottingham’. IAESV EMEDR Data Brief 21-02. Introduction In this data brief we provide some background on economic deprivation in Leicester and Nottingham. The data in this report largely pre-dates the coronavirus pandemic and so identifies long-term economic challenges in the respective cities. The coronavirus pandemic will no doubt exasperate these challenges. In the brief we look at: • Measures of deprivation, • Employment and wages, • Skills and type of employment. Key findings • Leicester and Nottingham are two of the most deprived areas in England with high levels of income deprivation and skills deprivation. • In comparison to other cities, Leicester and Nottingham residents earn relatively low salaries and work in relatively low-skilled occupations. • In comparison to other cities, Leicester residents have relatively low levels of qualification. Nottingham is closer to the national average. Definitions We focus on Leicester and Nottingham as defined by the unitary authority boundary. We also focus on people who are resident in the two cities, rather than people who work there. Source of data. We are using data from a range of sources but primarily the Annual Survey of Hours and Earnings (ASHE) and the Annual Population Survey (APS), accessed on Nomis. The Annual Survey of Hours and Earnings is based on a snapshot of the workforce in April of each year. -

Derby Nottingham Leicester # # # # # # # Cc05 : East Midlands
T070 #17 A38 EUROGAUGE-CAPABLE NORTH- A61 HIGH SPEED UK : REGIONAL MAPS SOUTH FREIGHT ROUTE 0 ASHFIELD PARKWAY 07 1 ALFRETON T04 CC05 : EAST MIDLANDS KIRKBY in MML T069 2828 ASHFIELD T05 214 © NETWORK2020 MAPPING JULY 2018 A6 FOR EXPLANATION OF SYMBOLS IN M1 T068 HSUK MAPPING SEE KEY PLAN K01 HSUK 27 A60 FOR FURTHER INFO SEE HSUK EAST MIDLANDS RAIL STRATEGY T067 NOTTINGHAM–BOTTESFORD–GRANTHAM 16 ROUTE UPGRADED & BOTTESFORD–NEWARK A38 # HUCK- BELPER A610 ROUTE RESTORED TO ACCESS ECML TO 0T066 NALL SOUTH & NORTH AND ENHANCE INTERCITY GREAT NORTHERN ROUTE 1 FLOWS THROUGH NOTTINGHAM FROM DERBY TO EREWASH EASTWOOD BIRMINGHAM- VALLEY RESTORED TO NOTTINGHAM ALLOW DIRECT ACCESS TO DIRECT HS HSUK FROM UPGRADED NOTTINGHAM ROUTE VIA XCML ROUTE VIA DERBY RESTORED T065 EXPRESS D065 26 DERBY TRANSIT TEARDROP D064 (NET) T064 NOTTINGHAM D063 ILKESTON N161 N065 N068 PRIMARY HIGH D062 N162 N064 N067 SPEED INTERCITY HUB AT DERBY HSUK & NORTH-SOUTH MIDLAND EUROGAUGE FREIGHT N066 15 ROUTE VIA TOTON YARD # D061 & EREWASH VALLEY LINE, 0 T063 A52 A38 UPGRADED/RESTORED TO N063 D001 4 TRACKS 1 25 A46 DERBY T062 D060 A52 N062 A606 NOTE ONGOING A453 NET EXTENSIONS D059 A6 MML T061 TO TOTON & XCML N061 PRIMARY HIGH SPEED CLIFTON INTERCITY HUB AT D058 NOTTINGHAM MIDLAND A50 T060 POTENTIAL FREIGHT YARD 5 D057 & TRAIN MAINTENANCE 5 24A #14 DEPOT AT TOTON 24 HSUK0 DIRECT HIGH SPEED ACCESS TO NOTTINGHAM VIA NEW DERBY AVOIDING LINE UPGRADED AS 1 EAST T059 ROUTE AVOIDING ATTEN- CORE ELEMENT OF EUROGAUGE- MML BOROUGH LEVEL CROSSINGS CAPABLE NORTH-SOUTH FREIGHT ROUTE MIDLANDS -

23-25 Whitley Street Reading, Berkshire RG2 0EG Flats 26, 27
Flats 26, 27 & 39 Minster Court LOT 2 Lower Brown Street 81 Leicester, Leicestershire LE1 5TH By Order of a Housing Association Three flats located in an attractive block let on Assured Shorthold Tenancies, well located for the centre of Leicester and De Montfort University. Investment let at £17,820 per annum . Tenure Leicester Leasehold. 125 year lease from 29th Description September 2002. • Three flats located in an attractive Ground rent £100 per annum. apartment block • Two allocated parking spaces Location • Situated by the junction with York Road Accommodation and Tenancies • A variety of shops, cafés, bars and A schedule of Accommodation and restaurants can be found close by in Tenancies is set out bel ow. the centre of Leicester • Castle Park and Nelson Mandela Park Total Current Rent £17,820 per annum are both within easy reach • Highly convenient for De Montfort University and Leicester Royal Infirmary Unit Accommodation Tenancy Rent (p.c. m.) Flat 26 One Bedroom Flat Assured Shorthold Tenancy £450 Plan not to scale Flat 27 Two Bedroom Flat Assured Shorthold Tenancy £560 Crown Copyright reserved. Flat 39 One Bedroom Flat Assured Shorthold Tenancy £475 This plan is based upon the Ordnance Survey Map with the sanction of the Controller of H M Stationery Office. LOT 23-25 Whitley Street 82 Reading, Berkshire RG2 0EG A mid terrace building arranged as a ground floor shop unit (let at £17,000 per annum) and a ten bedroom fully licensed vacant HMO above which has been recently refurbished. Well located in the centre of Reading, close to local shops and restaurants. -

STP: Latest Position Developing and Delivering the Humber, Coast and Vale Sustainability and Transformation Plan July 2016 Who’S Involved?
STP: Latest position Developing and delivering the Humber, Coast and Vale Sustainability and Transformation Plan July 2016 Who’s involved? NHS Commissioners Providers Local Authorities East Riding of Yorkshire CCG Humber NHS Foundation Trust City of York Council Hull CCG North Lincolnshire and Goole East Riding of Yorkshire Council NHS Foundation Trust Hull City Council North Lincolnshire CCG Tees, Esk and Wear Valleys North East Lincolnshire CCG NHS Foundation Trust North Lincolnshire Council City Health Care Partnerships North East Lincolnshire Council Scarborough and Ryedale CCG CIC Vale of York CCG Hull and East Yorkshire North Yorkshire County Council Hospitals NHS Trust Navigo Rotherham, Doncaster and South Humber NHS Foundation Trust York Teaching Hospital NHS Foundation Trust Our footprint Population characteristics 1.4 million population 23% live in the most deprived areas of England Diverse rural, urban and coastal communities Huge variation in health outcomes Three main acute providers Hull and East Yorkshire Hospitals NHS Trust North Lincolnshire and Goole NHS Foundation Trust York Teaching Hospital NHS Foundation Trust Drivers for change • Financial pressures across the system – significant and growing financial deficit across the system, doing nothing is not an option • Average life expectancies across the footprint range widely • Smoking, child and adult obesity rates and excessive alcohol consumption are above (some significantly) national averages • Stroke – our premature mortality rates from stroke are higher than average -

Identifying Richard III – an Interview with Dr Turi King
The Post Hole Special Feature Identifying Richard III – an interview with Dr Turi King Emily Taylor1 1Department of Archaeology, University of York, The King’s Manor, York, YO1 7EP Email: [email protected] In light of the recent discovery of Richard III, Dr Turi King, lecturer in genetics and archaeology at the University of Leicester, talks about her involvement in the research project that found England’s final Plantagenet king in this exclusive interview with The Post Hole. You were an important part in the exciting search for Richard III. When did you become involved with the project? Richard Buckley contacted me about the idea of my involvement in 2011, but it wasn’t until August 2012 that the project went ahead. The University of Leicester worked in collaboration with the Richard III Society and Leicester City Council and the search didn’t begin until 2012 due to issues with getting funding sorted and carrying out the desk-based survey. In 1986, David Baldwin wrote an article called 'King Richard's Grave in Leicester' giving the potential location of Richard’s grave. Then the historian John Ashdown-Hill wrote a book in 2011, The Last Days of Richard III, which again spoke about the likely location of the grave and also included a section on the possibility of identifying Richard through DNA analysis. John had traced a female line relative of Richard III, Joy Ibsen, who could act as a comparator if any putative remains of Richard III were found. This, among other things, inspired Philippa Langley to contact the University of Leicester Archaeological Services about the possibility of carrying out an archaeological project. -
02/07/2018 – 30/06/2022 Document 1 of 2 Version 4 – May 2019
02/07/2018 – 30/06/2022 Document 1 of 2 Version 4 – May 2019 1 Provider Page ABC Counselling, Play Therapy & Family Solutions C.I.C. 3 ‐ 6 A Time 4 You Child and Family Psychological Services Ltd 7 – 10 Alliance Psychological Services Limited 11 – 14 Barnardo’s 15 – 17 Brook 18 – 21 Children North East 22 – 24 Doorways 25 – 27 MATRIX Neurological 28 – 31 Rainbows End Coaching 32 – 34 Redcar and Cleveland Mind 35 – 37 Tees Valley Therapies 38 – 39 The Junction 40 – 42 The Link CIC 43 – 46 The Wellbeing Centre (Saltburn) CIC 47 – 48 Volunteering Matters 49 – 52 Intervention costs are outlined in a separate document, Schools and RCBC staff can obtain a copy of this by emailing: becky.dale@redcar‐cleveland.gov.uk 2 Name of organisation: ABC Counselling, Play Therapy & Family Solutions C.I.C. Contact name for Peter Lowe MBE or Karen Lowe referrals/enquiries: Email [email protected] ‐ [email protected] Contact Details: Tel 01642 913060 mobile : 07971072789 ‐ 07939922194 Website: www.abccounsellingservices.com Overview of Partnership working services/interventions: ABC Counselling, Play Therapy & Family Solutions and A Time 4 You Psychological Service partnered together to expand reach and share professional expertise and have provided professional counselling and play therapy across over 60 schools in the Tees valley area. We have built up excellent working relationships with key staff, children and importantly Parents to support children and young people to build resilience and use coping strategies through a range of therapeutic interventions, both short and long term, including group work. What we provide Support can be offered to any child or young person with emotional, behavioural or mild to moderate mental health concerns.