Psychosocial Stress and Addison's Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
1 COPYRIGHT STATEMENT This Copy of the Thesis Has Been
University of Plymouth PEARL https://pearl.plymouth.ac.uk 04 University of Plymouth Research Theses 01 Research Theses Main Collection 2012 Life Expansion: Toward an Artistic, Design-Based Theory of the Transhuman / Posthuman Vita-More, Natasha http://hdl.handle.net/10026.1/1182 University of Plymouth All content in PEARL is protected by copyright law. Author manuscripts are made available in accordance with publisher policies. Please cite only the published version using the details provided on the item record or document. In the absence of an open licence (e.g. Creative Commons), permissions for further reuse of content should be sought from the publisher or author. COPYRIGHT STATEMENT This copy of the thesis has been supplied on condition that anyone who consults it is understood to recognize that its copyright rests with its author and that no quotation from the thesis and no information derived from it may be published without the author’s prior consent. 1 Life Expansion: Toward an Artistic, Design-Based Theory of the Transhuman / Posthuman by NATASHA VITA-MORE A thesis submitted to the University of Plymouth in partial fulfillment for the degree of DOCTOR OF PHILOSOPHY School of Art & Media Faculty of Arts April 2012 2 Natasha Vita-More Life Expansion: Toward an Artistic, Design-Based Theory of the Transhuman / Posthuman The thesis’ study of life expansion proposes a framework for artistic, design-based approaches concerned with prolonging human life and sustaining personal identity. To delineate the topic: life expansion means increasing the length of time a person is alive and diversifying the matter in which a person exists. -

ACTH Stimulation Tests for the Diagnosis of Adrenal Insufficiency: Systematic Review and Meta-Analysis
ORIGINAL ARTICLE ACTH Stimulation Tests for the Diagnosis of Adrenal Insufficiency: Systematic Review and Meta-Analysis Naykky Singh Ospina,* Alaa Al Nofal,* Irina Bancos, Asma Javed, Khalid Benkhadra, Ekta Kapoor, Aida N. Lteif, Neena Natt, and M. Hassan Murad Evidence-Based Practice Research Program (N.S.O., A.A.N., K.B., M.H.M.), Mayo Clinic, Rochester, Downloaded from https://academic.oup.com/jcem/article/101/2/427/2810551 by guest on 29 September 2021 Minnesota; Knowledge and Evaluation Research Unit (N.S.O., K.B., M.H.M.), Mayo Clinic, Rochester, Minnesota; Division of Endocrinology, Diabetes, Metabolism, and Nutrition (N.S.O., N.N., I.B.), Mayo Clinic, Rochester, Minnesota; Division of Pediatric Endocrinology and Metabolism (A.A.N., A.J., A.N.L.), Mayo Clinic, Rochester, Minnesota; Division of General Internal Medicine (E.K.), Mayo Clinic, Rochester, Minnesota 55905 Context: The diagnosis of adrenal insufficiency is clinically challenging and often requires ACTH stimulation tests. Objective: To determine the diagnostic accuracy of the high- (250 mcg) and low- (1 mcg) dose ACTH stimulation tests in the diagnosis of adrenal insufficiency. Methods: We searched six databases through February 2014. Pairs of independent reviewers se- lected studies and appraised the risk of bias. Diagnostic association measures were pooled across studies using a bivariate model. Data Synthesis: For secondary adrenal insufficiency, we included 30 studies enrolling 1209 adults and 228 children. High- and low-dose ACTH stimulation tests had similar diagnostic accuracy in adults and children using different peak serum cortisol cutoffs. In general, both tests had low sensitivity and high specificity resulting in reasonable likelihood ratios for a positive test (adults: high dose, 9.1; low dose, 5.9; children: high dose, 43.5; low dose, 7.7), but a fairly suboptimal likelihood ratio for a negative test (adults: high dose, 0.39; low dose, 0.19; children: high dose, 0.65; low dose, 0.34). -

Spangler Ku 0099D 11237 DA
Abstract This study sought to gain a deeper understanding of the types of benefits, programs, and organizational practices employers currently are providing to prevent distress among employees or to help employees become more resilient to adverse conditions. Forty-six employer representatives discussed the perceived strengths of their organizations’ approaches during interviews and discussion groups. Grounded theory methodology was employed to sample and analyze these data. Based on patterns that emerged from the narratives of these participants, a model is proposed to explain three effective approaches used by employers in addressing stress in the workplace: 1) preventing stress/building resilience, 2) providing information, resources, and benefits to employees, and 3) intervening actively with troubled employees. Trust, both in relationships and in organizational structures, emerged as a core concept explaining effectiveness of these approaches. This model may be used to frame future strategies used by employers to support healthy engaged employees and to guide investigations into social and emotional aspects related to work. iii Acknowledgments Finishing a dissertation feels similar to climbing a mountain – looking back on where you have been makes you feel a little weary, but the view from the top is quite exhilarating and immensely satisfying. You also see there are other peaks left to master. I offer warm gratitude to many people who helped me during my climb. To all of the professors over the years who created opportunities for thinking deeply and pondering life’s important questions. To Lisa Mische Lawson for helping to chart my course of study over the years in the Therapeutic Science curriculum and advice during the dissertation process. -

SNAP Cortisol Testing Guide
SNAP® Cortisol Testing Guide Diagnosing and Treating Cases of Suspected Canine Hyperadrenocorticism or Addison’s Disease IMPORTANT: Review history of any administration of corticosteroids as these may influence the reported results. Diagnose ACTH Stimulation Test Diagnostic Protocol for Cases of Suspected Canine Hyperadrenocorticism or Addison’s Disease History, physical exam, CBC, chemistry panel, electrolytes and urinalysis consistent with Canine Hyperadrenocorticism or Addison’s disease Draw baseline cortisol sample. Perform an ACTH stimulation test with Cortrosyn® 5 µg/kg IV or ACTH gel 2.2 U/kg IM. Draw 1-hour cortisol (Cortrosyn®) or 1 and 2-hour cortisol (ACTH gel). Pre-ACTH: 2–6 µg/dL Pre- and Post-ACTH Post-ACTH Post-ACTH Post-ACTH 2 6 µg/dL >22 µg/dL <2 µg/dL – Post-ACTH: 6–18 µg/dL 18–22 µg/dL If both results are <2 µg/dL, results are Equivocal, Consistent Inconclusive consistent with Normal Cushing’s possible with Cushing’s hypoadrenocorticism Perform high-dose dexamethasone* Begin treatment with suppression to mineralocorticoid discriminate between and/or glucocorticoid PDH and ATH, as appropriate. ACTH level and/or abdominal ultrasound. * Do not exceed 0.1 mg/kg of dexamethasone. Diagnose Low-Dose Dexamethasone Suppression Protocol For Cases of Suspected Canine Hyperadrenocorticism History, physical exam, CBC, chemistry panel, electrolytes and urinalysis consistent with Canine Hyperadrenocorticism Draw baseline cortisol sample. Perform a low-dose dexamethasone suppression test with 0.01 mg/kg of dexamethasone IV. Draw 4-hour -
Code Procedure Description Adrenalectomy 60540 Adrenalectomy, Partial Or Complete, Or Exploration of Adrenal Gland with Or Witho
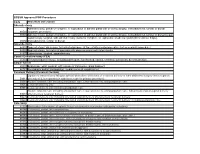
BCBSM Approved POP Procedures Code Procedure Description Adrenalectomy Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal 60540 (separate procedure) 60545 Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal (separate procedure); with excision of adjacent retroperitoneal tumor Laparoscopy, surgical, with adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, 60650 transabdominal, lumbar or dorsal Appendectomy 44955 Appendectomy; when done for indicated purpose at time of other major procedure (not as separate procedure) 44960 Appendectomy; for ruptured appendix with abscess or generalized peritonitis 44970 Laparoscopy, surgical, appendectomy Carotid Endarterectomy (CEA) 35301 Thromboendarterectomy, including patch graft, if performed; carotid, vertebral, subclavian, by neck incision Carpal Tunnel 29848 Endoscopy, wrist, surgical, with release of transverse carpal ligament 64721 Neuroplasty and/or transposition; median nerve at carpal tunnel Cesarean Delivery (Cesarean Section) Ligation or transection of fallopian tube(s) when done at the time of cesarean delivery or intra-abdominal surgery (not a separate 58611 procedure) (List separately in addition to code for primary procedure) 59510 Routine obstetric care including antepartum care, cesarean delivery, and postpartum care 59514 Cesarean delivery only 59515 Cesarean delivery only; including postpartum care -

Adrenalectomy Patient Information Leaflet
Adrenalectomy Patient information leaflet UHB is a no smoking Trust To see all of our current patient information leaflets please visit www.uhb.nhs.uk/patient-information-leaflets.htm What is an adrenalectomy? An adrenalectomy (ad-renal-ect-omy) is an operation to remove one or both of the adrenal glands. The adrenal glands sit above the kidneys. Right Left adrenal adrenal gland gland Kidney Kidney The main role of the adrenal glands is to release hormones into the body. The main hormones released are stress related hormones (cortisol, noradrenaline and adrenaline), hormones that regulate metabolism, hormones that affect immune system function, androgens (sex hormones) and hormones for saltwater balance (aldosterone). 2 | PI18/1289/03 Adrenalectomy An adrenalectomy can be done: • ‘Open’ with one large surgical cut below the ribcage • Or ‘laparoscopic’ which involves four smaller cuts being made allowing the inside of the abdomen to be seen using a camera Some laparoscopic operations may have be converted to ‘open’ at the time of the surgery due to the surgeon not being able to see the inside of the abdomen clearly enough (about 5% of cases). The surgery is performed under general anaesthetic so you will be asleep and will not feel any pain. The surgery normally takes 1–2 hours. The adrenal gland(s) will be sent to a pathologist after it is removed for further tests in a laboratory using a microscope. Why is an adrenalectomy performed? The adrenal gland(s) need to be removed if there is a mass/ tumour in the gland(s). An adrenalectomy is performed if: 1. -

Advances in Risk-Oriented Surgery for Multiple Endocrine Neoplasia Type 2
25 2 Endocrine-Related A Machens et al. Advances in risk-oriented 25:2 T41–T52 Cancer surgery for MEN2 THEMATIC REVIEW Advances in risk-oriented surgery for multiple endocrine neoplasia type 2 Andreas Machens1 and Henning Dralle2 1Department of General, Visceral and Vascular Surgery, Martin Luther University Halle-Wittenberg, Halle, Saale, Germany 2Department of General, Visceral and Transplantation Surgery, Section of Endocrine Surgery, University of Duisburg-Essen, Essen, Germany Correspondence should be addressed to A Machens: [email protected] This paper is part of a thematic review section on 25 Years of RET and MEN2. The guest editors for this section were Lois Mulligan and Frank Weber. Abstract Genetic association studies hinge on definite clinical case definitions of the disease of Key Words interest. This is why more penetrant mutations were overrepresented in early multiple f biochemical screening endocrine neoplasia type 2 (MEN2) studies, whereas less penetrant mutations went f DNA-based screening underrepresented. Enrichment of genetic association studies with advanced disease f RET proto-oncogene may produce a flawed understanding of disease evolution, precipitating far-reaching f gene test surgical strategies like bilateral total adrenalectomy and 4-gland parathyroidectomy in f gene carrier MEN2. The insight into the natural course of the disease gleaned over the past 25 years f multiple endocrine caused a paradigm shift in MEN2: from the removal of target organs at the expense of neoplasia type 2A greater operative -

Stress, Cortison Und Homöostase
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by RERO DOC Digital Library N.T.M. 18 (2010) 169–195 0036-6978/10/020169-27 DOI 10.1007/s00048-010-0017-2 Published online: 10 August 2010 RTICLES PRINGER ASEL Ó 2010 S B AG /A . RTIKEL A Stress, Cortison und Homöostase Künstliche Nebennierenrindenhormone und physiologisches Gleichgewicht, 1936–1960 Lea Haller Stress, Cortisone and Homeostasis. Adrenal Cortex Hormones and Physiological Equilibrium, 1936–1960 This article investigates the emergence of the concept of stress in the 1930s and outlines its changing disciplinary and conceptual frames up until 1960. Originally stress was a physio- logical concept applied to the hormonal regulation of the body under stressful conditions. Correlated closely with chemical research into corticosteroids for more than a decade, the stress concept finally became a topic in cognitive psychology. One reason for this shift of the concept to another discipline was the fact that the hormones previously linked to the stress concept were successfully transferred from laboratory to medical practice and adopted by disciplines such as rheumatology and dermatology. Thus the stress concept was dissociated from its hormonal context and became a handy formula that allowed postindustrial soci- ety to conceive of stress as a matter of individual concern. From a physiological phenomenon stress turned into an object of psychological discourse and individual coping strategies. Keywords: Stress, general adaptation syndrome, hormones of the adrenal cortex, corti- sone therapy, coping Schlüsselwörter: Stress, Allgemeines Adaptationssyndrom, Nebennierenrindenhormone, Cortisontherapie, Stressbewältigung ,,No concept in the modern psychological, sociological, or psychiatric literature is more extensively studied than stress.’’ Stevan E. -

Use of Dexmedetomidine in a Parturient with Multiple Endocrine Neoplasia Type 2A Undergoing Adrenalectomy and Thyroidectomy
PRACTICE CASE REPORT Use of Dexmedetomidine in a Parturient With Multiple Endocrine Neoplasia Type 2A Undergoing Adrenalectomy and Thyroidectomy: A Case Report Amanda L. Faulkner, MD, Eric Swanson, MD, Thomas L. McLarney, MD, Cortney Y. Lee, MD, and Annette Rebel, MD * * * † * 08/15/2018 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3yRlXg5VZA8uqNuqWFo8dRhJiNZRTFLkCeIa0nEMHM2KbYm37VRaE3A== by https://journals.lww.com/aacr from Downloaded Dexmedetomidine is a selective α2-agonist, frequently used in perioperative medicine as anes- thesia adjunct. The medication carries a Food and Drug Administration pregnancy category C Downloaded designation and is therefore rarely used for parturients undergoing nonobstetric surgery. We are reporting the use of dexmedetomidine in the anesthetic management of a parturient undergoing minimally invasive unilateral adrenalectomy for pheochromocytoma during the second trimester from https://journals.lww.com/aacr of pregnancy. Additionally, because of the multiple endocrine neoplasia type 2A constellation with diagnosis of medullary thyroid cancer, the patient underwent a total thyroidectomy 1 week after the adrenalectomy. (A&A Practice. XXX;XXX:00–00.) exmedetomidine is a selective α2-agonist, fre- CASE REPORT by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3yRlXg5VZA8uqNuqWFo8dRhJiNZRTFLkCeIa0nEMHM2KbYm37VRaE3A== quently used in perioperative medicine. It has A 34-year-old gravida 3 para 2 woman (body weight, 61 Dfound favor in this setting because of its sedative kg; -

Cinemeducation Movies Have Long Been Utilized to Highlight Varied
Cinemeducation Movies have long been utilized to highlight varied areas in the field of psychiatry, including the role of the psychiatrist, issues in medical ethics, and the stigma toward people with mental illness. Furthermore, courses designed to teach psychopathology to trainees have traditionally used examples from art and literature to emphasize major teaching points. The integration of creative methods to teach psychiatry residents is essential as course directors are met with the challenge of captivating trainees with increasing demands on time and resources. Teachers must continue to strive to create learning environments that give residents opportunities to apply, analyze, synthesize, and evaluate information (1). To reach this goal, the use of film for teaching may have advantages over traditional didactics. Films are efficient, as they present a controlled patient scenario that can be used repeatedly from year to year. Psychiatry residency curricula that have incorporated viewing contemporary films were found to be useful and enjoyable pertaining to the field of psychiatry in general (2) as well as specific issues within psychiatry, such as acculturation (3). The construction of a formal movie club has also been shown to be a novel way to teach psychiatry residents various aspects of psychiatry (4). Introducing REDRUMTM Building on Kalra et al. (4), we created REDRUMTM (Reviewing [Mental] Disorders with a Reverent Understanding of the Macabre), a Psychopathology curriculum for PGY-1 and -2 residents at Rutgers Robert Wood Johnson Medical School. REDRUMTM teaches topics in mental illnesses by use of the horror genre. We chose this genre in part because of its immense popularity; the tropes that are portrayed resonate with people at an unconscious level. -

Surgical Indications and Techniques for Adrenalectomy Review
THE MEDICAL BULLETIN OF SISLI ETFAL HOSPITAL DOI: 10.14744/SEMB.2019.05578 Med Bull Sisli Etfal Hosp 2020;54(1):8–22 Review Surgical Indications and Techniques for Adrenalectomy Mehmet Uludağ,1 Nurcihan Aygün,1 Adnan İşgör2 1Department of General Surgery, Sisli Hamidiye Etfal Training and Research Hospital, Istanbul, Turkey 2Department of General Surgery, Bahcesehir University Faculty of Medicine, Istanbul, Turkey Abstract Indications for adrenalectomy are malignancy suspicion or malignant tumors, non-functional tumors with the risk of malignancy and functional adrenal tumors. Regardless of the size of functional tumors, they have surgical indications. The hormone-secreting adrenal tumors in which adrenalectomy is indicated are as follows: Cushing’s syndrome, arises from hypersecretion of glucocorticoids produced in fasciculata adrenal cortex, Conn’s syndrome, arises from an hypersecretion of aldosterone produced by glomerulosa adrenal cortex, and Pheochromocytomas that arise from adrenal medulla and produce catecholamines. Sometimes, bilateral adre- nalectomy may be required in Cushing's disease due to pituitary or ectopic ACTH secretion. Adenomas arise from the reticularis layer of the adrenal cortex, which rarely releases too much adrenal androgen and estrogen, may also develop and have an indication for adrenalectomy. Adrenal surgery can be performed by laparoscopic or open technique. Today, laparoscopic adrenalectomy is the gold standard treatment in selected patients. Laparoscopic adrenalectomy can be performed transperitoneally or retroperitoneoscopi- cally. Both approaches have their advantages and disadvantages. In the selection of the surgery type, the experience and habits of the surgeon are also important, along with the patient’s characteristics. The most common type of surgery performed in the world is laparoscopic transabdominal lateral adrenalectomy, which most surgeons are more familiar with. -

Commemorating a Classic, and Its Creator Walter Bradford Cannon
Indian J Physiol Pharmacol 1998; 42(4) : 437-439 Editorial Commemorating a Classic, and its Creator Walter Bradford Cannon Some papers are born great, some become great, and some have greatness thrust upon them. We have decided to thrust greatness on a paper published 100 years ago in Volume 1 of the American Journal of Physiology (1). Not that the paper is not good, but of far greater interest to us is its author. But first, the paper: it described for the first time the use of X-rays for the study of gastric motility. The study was done on cats who had been given food mixed with the radio-opaque material, 'bismuth subnitrate. By following the changes in shape of the shadows on a f1uorescent screen, Cannon deduced a wealth of information. He described the shape of the stomach, the frequency and nature of contractions, possible function of contractions and the rate and pattern of gastric emptying. By observing that food cornered in the fundus remains undisturbed for quite some time, he concluded that digestion by salivary amylase may continue in the fundus. He confirmed it by measuring the pH of different 'layers' of food in the fundus. The pH was alkaline in the food extracted from a dept of two and half centimetres one and a half hour after ingestion. He also described the differences in handling of foods of different consistencies by the stomach. Further, by observing absence of peristalsis in cats that went into rage during recording (generally, male cats !), he concluded that anger inhibits gastric emptying.