Preoperative and Intraoperative Methods of Parathyroid Gland Localization and the Diagnosis of Parathyroid Adenomas
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thyroid Gland Parathyroid Glands
Human Physiology Course Thyroid Gland Parathyroid Glands Assoc. Prof. Mária Pallayová, MD, PhD [email protected] Department of Human Physiology, UPJŠ LF April 13, 2020 (10th week – Summer Semester 2019/2020) Hormones and Functions Thyroid gland Parathyroids Thymus Adrenal glands Endocrine pancreas Ovaries, Testes Pineal Pituitary Hypothalamus-Pituitary Axis GIT, adipose tissue, brain, heart, kidney, ... Hormones and Functions Thyroid gland Parathyroids Thymus Adrenal glands Endocrine pancreas Ovaries, Testes Pineal Pituitary Hypothalamus-Pituitary Axis GIT, adipose tissue, brain, heart, kidney, ... Lecture Outline Functional anatomy of the thyroid gland Synthesis, secretion, and metabolism of the thyroid hormones The mechanism of thyroid action Role of the thyroid hormones in development, growth, and metabolism Thyroid hormone deficiency and excess in adults Physiology of the parathyroids Functional Anatomy of the Thyroid Gland two lobes + isthmus (just below the cricoid cartilage) attached to the trachea by connective tissue A normal THGL in a healthy adult weighs about 15-20 g. Functional Anatomy of the Thyroid Gland arterial blood supply: from a superior and an inferior thyroid a., which arise from the external carotid and subclavian a., respectively. venous blood supply: a series of thyroid veins drain into the ext. jugular and innominate vv. ( a rich blood supply to the thyroid gland w/ a higher rate of blood flow per gram than even that of the kidneys). innervation: adrenergic innervation from the cervical ganglia; cholinergic innervation from the n. vagus (regulation of vasomotor function to increase the delivery of TSH, iodide, and metabolic substrates to the THGL). Functional Anatomy of the Thyroid Gland The colloid (a thick, gel-like substance) is a solution composed primarily of thyroglobulin (10-25% the high viscosity), a large protein that is a storage form of the thyroid hormones. -

The Fine Structure of the Parathyroid Gland*
The Fine Structure of the Parathyroid Gland* BY JERRY STEVEN TRIER, M.D. (From the Department of Anatomy, University of Washington School of Medicine, Seattle) PLATES 3 TO 10 (Received for publication, July 29, 1957) ABSTRACT The fine structure of the parathyroid of the macaque is described, and is cor- related with classical parathyroid cytology as seen in the light microscope. The two parenchymal cell types, the chief cells and the oxyphil cells, have been recognized in electron mierographs. The chief cells contain within their cyto- plasm mitochondria, endoplasmic reticulum, and Golgi bodies similar to those found in other endocrine tissues as well as frequent PAS-positive granules. The juxtanuclear body of the light microscopists is identified with stacks of parallel lamellar elements of the endoplasmic rcticulum of the ergastoplasmic or granular type. Oxyphll cells are characterized by juxtanuclear bodies and by numerous mito- chondria found throughout their cytoplasm. Puzzling lamellar whorls are described in the cytoplasm of some oxyphil cells. The endothelium of parathyroid capillaries is extremely thin in some areas and contains numerous fenestrations as well as an extensive system of vesicles. The possible significance of these structures is discussed. The connective tissue elements found in the perivascular spaces of macaque parathyroid are described. INTRODUCTION Other contributions to the present concepts con cerning the human parathyroid can be found in the It is the purpose of the present paper to report some observations on the fine structure of the reports of Bergstrand (7), Morgan (34), Pappen- parathyroid gland employing the electron micro- heimer and Wilens (45), Castleman and Mallory (10), and Gilmour (20). -
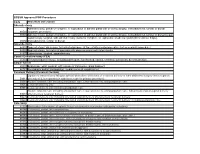
Code Procedure Description Adrenalectomy 60540 Adrenalectomy, Partial Or Complete, Or Exploration of Adrenal Gland with Or Witho
BCBSM Approved POP Procedures Code Procedure Description Adrenalectomy Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal 60540 (separate procedure) 60545 Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal (separate procedure); with excision of adjacent retroperitoneal tumor Laparoscopy, surgical, with adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, 60650 transabdominal, lumbar or dorsal Appendectomy 44955 Appendectomy; when done for indicated purpose at time of other major procedure (not as separate procedure) 44960 Appendectomy; for ruptured appendix with abscess or generalized peritonitis 44970 Laparoscopy, surgical, appendectomy Carotid Endarterectomy (CEA) 35301 Thromboendarterectomy, including patch graft, if performed; carotid, vertebral, subclavian, by neck incision Carpal Tunnel 29848 Endoscopy, wrist, surgical, with release of transverse carpal ligament 64721 Neuroplasty and/or transposition; median nerve at carpal tunnel Cesarean Delivery (Cesarean Section) Ligation or transection of fallopian tube(s) when done at the time of cesarean delivery or intra-abdominal surgery (not a separate 58611 procedure) (List separately in addition to code for primary procedure) 59510 Routine obstetric care including antepartum care, cesarean delivery, and postpartum care 59514 Cesarean delivery only 59515 Cesarean delivery only; including postpartum care -

Adrenalectomy Patient Information Leaflet
Adrenalectomy Patient information leaflet UHB is a no smoking Trust To see all of our current patient information leaflets please visit www.uhb.nhs.uk/patient-information-leaflets.htm What is an adrenalectomy? An adrenalectomy (ad-renal-ect-omy) is an operation to remove one or both of the adrenal glands. The adrenal glands sit above the kidneys. Right Left adrenal adrenal gland gland Kidney Kidney The main role of the adrenal glands is to release hormones into the body. The main hormones released are stress related hormones (cortisol, noradrenaline and adrenaline), hormones that regulate metabolism, hormones that affect immune system function, androgens (sex hormones) and hormones for saltwater balance (aldosterone). 2 | PI18/1289/03 Adrenalectomy An adrenalectomy can be done: • ‘Open’ with one large surgical cut below the ribcage • Or ‘laparoscopic’ which involves four smaller cuts being made allowing the inside of the abdomen to be seen using a camera Some laparoscopic operations may have be converted to ‘open’ at the time of the surgery due to the surgeon not being able to see the inside of the abdomen clearly enough (about 5% of cases). The surgery is performed under general anaesthetic so you will be asleep and will not feel any pain. The surgery normally takes 1–2 hours. The adrenal gland(s) will be sent to a pathologist after it is removed for further tests in a laboratory using a microscope. Why is an adrenalectomy performed? The adrenal gland(s) need to be removed if there is a mass/ tumour in the gland(s). An adrenalectomy is performed if: 1. -

Advances in Risk-Oriented Surgery for Multiple Endocrine Neoplasia Type 2
25 2 Endocrine-Related A Machens et al. Advances in risk-oriented 25:2 T41–T52 Cancer surgery for MEN2 THEMATIC REVIEW Advances in risk-oriented surgery for multiple endocrine neoplasia type 2 Andreas Machens1 and Henning Dralle2 1Department of General, Visceral and Vascular Surgery, Martin Luther University Halle-Wittenberg, Halle, Saale, Germany 2Department of General, Visceral and Transplantation Surgery, Section of Endocrine Surgery, University of Duisburg-Essen, Essen, Germany Correspondence should be addressed to A Machens: [email protected] This paper is part of a thematic review section on 25 Years of RET and MEN2. The guest editors for this section were Lois Mulligan and Frank Weber. Abstract Genetic association studies hinge on definite clinical case definitions of the disease of Key Words interest. This is why more penetrant mutations were overrepresented in early multiple f biochemical screening endocrine neoplasia type 2 (MEN2) studies, whereas less penetrant mutations went f DNA-based screening underrepresented. Enrichment of genetic association studies with advanced disease f RET proto-oncogene may produce a flawed understanding of disease evolution, precipitating far-reaching f gene test surgical strategies like bilateral total adrenalectomy and 4-gland parathyroidectomy in f gene carrier MEN2. The insight into the natural course of the disease gleaned over the past 25 years f multiple endocrine caused a paradigm shift in MEN2: from the removal of target organs at the expense of neoplasia type 2A greater operative -

Use of Dexmedetomidine in a Parturient with Multiple Endocrine Neoplasia Type 2A Undergoing Adrenalectomy and Thyroidectomy
PRACTICE CASE REPORT Use of Dexmedetomidine in a Parturient With Multiple Endocrine Neoplasia Type 2A Undergoing Adrenalectomy and Thyroidectomy: A Case Report Amanda L. Faulkner, MD, Eric Swanson, MD, Thomas L. McLarney, MD, Cortney Y. Lee, MD, and Annette Rebel, MD * * * † * 08/15/2018 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3yRlXg5VZA8uqNuqWFo8dRhJiNZRTFLkCeIa0nEMHM2KbYm37VRaE3A== by https://journals.lww.com/aacr from Downloaded Dexmedetomidine is a selective α2-agonist, frequently used in perioperative medicine as anes- thesia adjunct. The medication carries a Food and Drug Administration pregnancy category C Downloaded designation and is therefore rarely used for parturients undergoing nonobstetric surgery. We are reporting the use of dexmedetomidine in the anesthetic management of a parturient undergoing minimally invasive unilateral adrenalectomy for pheochromocytoma during the second trimester from https://journals.lww.com/aacr of pregnancy. Additionally, because of the multiple endocrine neoplasia type 2A constellation with diagnosis of medullary thyroid cancer, the patient underwent a total thyroidectomy 1 week after the adrenalectomy. (A&A Practice. XXX;XXX:00–00.) exmedetomidine is a selective α2-agonist, fre- CASE REPORT by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3yRlXg5VZA8uqNuqWFo8dRhJiNZRTFLkCeIa0nEMHM2KbYm37VRaE3A== quently used in perioperative medicine. It has A 34-year-old gravida 3 para 2 woman (body weight, 61 Dfound favor in this setting because of its sedative kg; -

Surgical Indications and Techniques for Adrenalectomy Review
THE MEDICAL BULLETIN OF SISLI ETFAL HOSPITAL DOI: 10.14744/SEMB.2019.05578 Med Bull Sisli Etfal Hosp 2020;54(1):8–22 Review Surgical Indications and Techniques for Adrenalectomy Mehmet Uludağ,1 Nurcihan Aygün,1 Adnan İşgör2 1Department of General Surgery, Sisli Hamidiye Etfal Training and Research Hospital, Istanbul, Turkey 2Department of General Surgery, Bahcesehir University Faculty of Medicine, Istanbul, Turkey Abstract Indications for adrenalectomy are malignancy suspicion or malignant tumors, non-functional tumors with the risk of malignancy and functional adrenal tumors. Regardless of the size of functional tumors, they have surgical indications. The hormone-secreting adrenal tumors in which adrenalectomy is indicated are as follows: Cushing’s syndrome, arises from hypersecretion of glucocorticoids produced in fasciculata adrenal cortex, Conn’s syndrome, arises from an hypersecretion of aldosterone produced by glomerulosa adrenal cortex, and Pheochromocytomas that arise from adrenal medulla and produce catecholamines. Sometimes, bilateral adre- nalectomy may be required in Cushing's disease due to pituitary or ectopic ACTH secretion. Adenomas arise from the reticularis layer of the adrenal cortex, which rarely releases too much adrenal androgen and estrogen, may also develop and have an indication for adrenalectomy. Adrenal surgery can be performed by laparoscopic or open technique. Today, laparoscopic adrenalectomy is the gold standard treatment in selected patients. Laparoscopic adrenalectomy can be performed transperitoneally or retroperitoneoscopi- cally. Both approaches have their advantages and disadvantages. In the selection of the surgery type, the experience and habits of the surgeon are also important, along with the patient’s characteristics. The most common type of surgery performed in the world is laparoscopic transabdominal lateral adrenalectomy, which most surgeons are more familiar with. -

Thyroid & Parathyroid Glands
THYROID & PARATHYROID GLANDS Objectives: ◧ Editing file • Describe the histological structure of ◧ thyroid & parathyroid glands. Important • Identify and correlate between the different ◧ Doctor notes / Extra endocrine cells in thyroid gland and their functions. • Describe the functional structure of the parathyroid cells. 438 Histology Team Endocrine Block THYROID GLAND STROMA 1- Capsule: dense irregular collagenous C.T. 2- Septa (Interlobular septa) 3- Reticular fibers: Thin C.T. composed mostly of reticular fibers with rich capillary plexus surrounds each thyroid follicle. PARENCHYMA Are the structural and functional units of the thyroid gland. 1- Simple cuboidal epithelium: 2- Colloid: central colloid-filled lumen. a- Follicular (principal) cells b- Parafollicular cells (C cells) (Clear cells) - Pale-stained cells (Clear Cells). (Polygonal/pyramidal cells) N.B. Each follicle is - Simple cuboidal cells. - Found singly or in clusters in between the follicular cells. - Round nucleus with prominent nucleoli. surrounded by thin - Their apices do not reach the lumen of the follicle. L/M: - Basophilic cytoplasm. basal lamina. - Are larger than follicular cells (2-3 times).(larger but less in number) - Apical surface reaches the lumen of the (Acidophilic) - Only 0.1% of the epithelial cells. thyroid follicle. - Have round nucleus - Mitochondria. - RER. (synthesis of thyroglobulin) - Supranuclear Golgi Complex. - Mitochondria. E/M: - Numerous apically-located lysosomes. - RER (moderate). - Numerous dispersed small vesicles - Well-developed Golgi. - The vesicles contain newly formed thyroglobulin. - Numerous apical short microvilli. Function: Synthesis of thyroid hormones (T4 & T3). Secrete calcitonin. 438 Histology Team - Endocrine Block 2 PARATHYROID GLAND They are 4 glands on the posterior of thyroid gland. STROMA 1- Capsule: Each gland has its Thin capsule. -

Primary Hyperparathyroidism
Primary Hyperparathyroidism The parathyroid glands are 4 glands that reside within the thyroid glands: there are two parathyroid glands attached to each thyroid gland. The thyroid/parathyroid glands lie on either side of the trachea (wind pipe) about midway down the neck. The job of the parathyroid glands is to regulate calcium in the body. They secrete a hormone called parathyroid hormone (PTH), and this hormone draws calcium out of the bone where it is stored, as well as acting on the kidney and intestine to increase blood calcium. This is a normal process in response to fluctuations in blood calcium levels. The calcium in the blood is regulated by PTH (increases blood calcium) and calcitonin (a hormone secreted by the thyroid gland to decrease calcium) in order to keep it within a normal range. When the calcium gets too high or too low, symptoms arise. The most common symptoms of high calcium are increased thirst and urination. Other signs include: lethargy, weakness, diarrhea, inappetance, weight loss, tremors or stiffness. In about 50% of dogs with high calcium, urinary stones +/- urinary tract infection is present. Tumors (enlargement) of the parathyroid gland are typically not malignant, but they do over-secrete PTH. In 90% of cases only one of the four glands is enlarged. By one gland enlarging and over-secreting PTH, the three other glands typically shrink and temporarily stop functioning. Parathyroid tumors are suspected based on consistent blood work that shows elevated or normal PTH in the face of elevated calcium (the normal feedback mechanism would mean that when calcium is high, PTH is not needed and therefore is low). -

Parathyroid Disorders THOMAS C
Parathyroid Disorders THOMAS C. MICHELS, MD, MPH, Madigan Army Medical Center, Tacoma, Washington KEVIN M. KELLY, MD, MBA, Carl R. Darnall Army Community Hospital, Fort Hood, Texas Disorders of the parathyroid glands most commonly present with abnormalities of serum calcium. Patients with primary hyperparathyroidism, the most common cause of hypercalcemia in outpatients, are often asymptomatic or may have bone disease, nephrolithiasis, or neuromuscular symptoms. Patients with chronic kidney disease may develop secondary hyperparathyroidism with resultant chronic kidney disease-mineral and bone disorder. Hypo- parathyroidism most often occurs after neck surgery; it can also be caused by autoimmune destruction of the glands and other less common problems. Evaluation of patients with abnormal serum calcium levels includes a history and physical examination; repeat measurement of serum calcium level; and measurement of creatinine, magne- sium, vitamin D, and parathyroid hormone levels. The treatment for symptomatic primary hyperparathyroidism is parathyroidectomy. Management of asymptomatic primary hyperparathyroidism includes monitoring symptoms; serum calcium and creatinine levels; and bone mineral density. Patients with hypoparathyroidism require close monitoring and vitamin D (e.g., calcitriol) replacement. (Am Fam Physician. 2013;88(4):249-257. Copyright © 2013 American Academy of Family Physicians.) CME This clinical content he four parathyroid glands, located 84-amino acid peptide. PTH increases serum conforms to AAFP criteria posterior to the thyroid gland, reg- calcium levels through direct action on bone for continuing medical education (CME). See CME ulate calcium homeostasis through and the kidneys. It stimulates osteoclasts to Quiz on page 227. release of parathyroid hormone resorb bone and mobilize calcium into the T (PTH). Because most parathyroid disorders blood. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Primary Hyperparathyroidism
Primary Hyperparathyroidism National Endocrine and Metabolic Diseases Information Service What is primary What are the parathyroid hyperparathyroidism? glands? Primary hyperparathyroidism is a disorder The parathyroid glands are four pea-sized U.S. Department of the parathyroid glands, also called glands located on or near the thyroid gland of Health and parathyroids. “Primary” means this disorder in the neck. Occasionally, a person is born Human Services originates in the parathyroid glands. In with one or more of the parathyroid glands primary hyperparathyroidism, one or more in another location. For example, a gland NATIONAL INSTITUTES of the parathyroid glands are overactive. may be embedded in the thyroid, in the OF HEALTH As a result, the gland releases too much thymus—an immune system organ located parathyroid hormone (PTH). The disorder in the chest—or elsewhere around this area. includes the problems that occur in the rest In most such cases, however, the parathyroid of the body as a result of too much PTH—for glands function normally. example, loss of calcium from bones. In the United States, about 100,000 people develop primary hyperparathyroidism each year.1 The disorder is diagnosed most often in people between age 50 and 60, and women are affected about three times as often as men.2 Secondary, or reactive, hyperparathyroidism can occur if a problem such as kidney failure causes the parathyroid glands to be overactive. Parathyroid glands Thyroid gland The parathyroid glands are located on or near the thyroid gland in the neck. 1Bilezikian JP. Primary hyperparathyroidism. In: DeGroot LJ, ed.; Arnold A, section editor.