Advances in Risk-Oriented Surgery for Multiple Endocrine Neoplasia Type 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

When Is It Minimally Invasive?
ORIGINAL ARTICLE Incision Length for Standard Thyroidectomy and Parathyroidectomy When Is It Minimally Invasive? Laurent Brunaud, MD; Rasa Zarnegar, MD; Nobuyuki Wada, MD; Philip Ituarte, PhD; Orlo H. Clark, MD; Quan-Yang Duh, MD Hypothesis: Current techniques for open conven- parathyroidectomy (PϽ.001). It was 4.1 cm for bilateral tional thyroidectomy or parathyroidectomy have evolved parathyroid exploration, but was reduced to 3.2 and 2.8 to enable a shorter incision (main proposition), and the cm for unilateral (PϽ.001) and focal (PϽ.001) explora- length of the incision is influenced by objective factors. tions, respectively. By multiple regression analysis, thy- roid specimen volume and patient body mass index were Design: Case series. independent predictors of incision length in thyroidec- tomy. Extent of exploration and resident training level Setting: University referral center. were independent predictors of incision length in parathyroidectomy. Patients and Intervention: Retrospective study of the most recent 200 primary consecutive routine thyroid and Conclusions: Current techniques for open conven- parathyroid operations (excluding neck dissections). tional thyroidectomy or parathyroidectomy have evolved to enable a shorter incision. Thyroid volume, patient body Main Outcome Measures: The length of incision was mass index, extent of the planned parathyroid explora- routinely measured with a ruler before the incision. tion, and the resident clinical training stage are impor- Univariate and multivariate analysis was performed to dis- tant variables for incision length in open operation and tinguish variables affecting length of incision. should be taken into account when minimally invasive thyroidectomy and parathyroidectomy are evaluated. Results: Mean length of the incision was 5.5 cm for to- tal thyroidectomy, 4.6 cm for lobectomy, and 3.5 cm for Arch Surg. -

Inadvertent Parathyroidectomy During Thyroid Surgery for Papillary Thyroid Carcinoma and Postoperative Hypocalcemia
ORIGINAL J Korean Thyroid Assoc ARTICLE Vol. 5, No. 1, May 2012 Inadvertent Parathyroidectomy during Thyroid Surgery for Papillary Thyroid Carcinoma and Postoperative Hypocalcemia Dongbin Ahn, MD1, Jin Ho Sohn, MD, PhD1, Jae Hyug Kim, MD1, Ji Young Park, MD2 and Junesik Park, MD, PhD3 Departments of Otolaryngology-Head and Neck Surgery1, Pathology2, School of Medicine, Kyungpook National University, Department of Otolaryngology-Head and Neck Surgery, School of Medicine, Catholic University of Daegu3, Daegu, Korea Background and Objectives: The aim of this article is to report our experience of inadvertent parathyroidectomy during thyroid surgery and to analyze its associated factors and clinical implications. In addition, we attempted to determined causative factors that result in permanent hypocalcemia after thyroid surgery. Materials and Methods: We performed a retrospective review of 500 patients who underwent thyroid surgery for the treatment of papillary thyroid carcinoma from 2004 to 2008. Results: Inadvertent parathyroidectomy was identified in 7.4% of patients and only 1 parathyroid gland was inadvertently removed in most cases. The incidence of inadvertent parathyroidectomy was not associated with gender, age, type of surgical procedure, tumor size, coexisting Hashimoto’s thyroiditis (HT), extra-thyroidal extension (ETE), lymph node (LN) metastasis, and surgeon’s experience. Nor was inadvertent parathyroidectomy associated with permanent postoperative hypocalcemia. Although operating time >120 min, ETE, and total thyroidectomy (TT) with central neck dissection (CND) were found to be related to permanent hypocalcemia on univariate analysis, tumor size ≥1 cm and surgeon’s experience ≤5 years was statistically associated with permanent hypocalcemia on both univariate and multivariate analyses. Conclusion: Although inadvertent parathyroidectomy is not an uncommon complication of thyroid surgery, it appears to have only modest clinical implications. -

Postoperative Calcium Requirements in 6000 Patients Undergoing
Postoperative Calcium Requirements in 6,000 Patients Undergoing Outpatient Parathyroidectomy: Easily Avoiding Symptomatic Hypocalcemia Marie Vasher, MD, Arnold Goodman, MD, FACS, Douglas Politz, MD, FACS, FACE, James Norman, MD, FACS, FACE BACKGROUND: To determine the amount and duration of supplemental oral calcium for patients with varying clinical presentations discharged immediately after surgery for primary hyperparathyroidism. STUDY DESIGN: A 4-year, prospective, single-institution study of 6,000 patients undergoing parathyroidectomy for primary hyperparathyroidism and discharged within 2.5 hours. Based on our previous studies, patients are started on a sliding scale of oral calcium determined by a number of preoperative measures (ie, serum calcium, body weight, osteoporosis) beginning 3 hours post- operation and decreasing to a maintenance dose by week 3. Patients reported all hypocalcemia symptoms daily for 2 weeks. RESULTS: Seven parameters were found to have a substantial impact on the amount of calcium required to prevent symptomatic hypocalcemia: preoperative serum calcium Ͼ12 mg/dL, Ͼ13 mg/dL, and Ͼ13.5 mg/dL, bone density T score less than Ϫ3, morbid obesity, removal of Ͼ1 parathyroid, and manipulation/biopsy of all remaining glands (all p Ͻ 0.05). Each independent variable increased the daily calcium required by 315 mg/day. Using our scaled protocol, Ͻ8% of patients showed symptoms of hypocalcemia, nearly all of whom were successfully self-treated with additional oral calcium. Only 6 patients (0.1%) required a visit to the emergency room for IV calcium, all occurring on postoperative day 3 or later. CONCLUSION: After outpatient parathyroidectomy, a specific calcium protocol has been verified that elimi- nates development of symptomatic hypocalcemia in Ͼ92% of patients, identifies patients at high risk for hypocalcemia, and allows self-medication with confidence in a predictable fashion for those patients in whom symptoms develop. -

Radioguided Surgery of Primary Hyperparathyroidism Using the Low
Radioguided Surgery of Primary Hyperparathyroidism Using the Low-Dose 99mTc- Sestamibi Protocol: Multiinstitutional Experience from the Italian Study Group on Radioguided Surgery and Immunoscintigraphy (GISCRIS) Domenico Rubello, MD1; Maria Rosa Pelizzo, MD2; Giuseppe Boni, MD3; Riccardo Schiavo, MD4; Luca Vaggelli, MD5; Giuseppe Villa, MD6; Sergio Sandrucci, MD7; Andrea Piotto, MD2; Gianpiero Manca, MD3; Pierluigi Marini, MD8; and Giuliano Mariani, MD3 1Nuclear Medicine Service, “S. Maria della Misericordia” Hospital, Rovigo, Italy; 2Department of Surgery, University of Padua Medical School, Padua, Italy; 3Regional Center of Nuclear Medicine, University of Pisa Medical School, Pisa, Italy; 4Nuclear Medicine Service, “S. Camillo-Forlanini” Hospital, Rome, Italy; 5Nuclear Medicine Service, “Careggi” University Hospital, Florence, Italy; 6Nuclear Medicine Service, “S. Martino” University Hospital, Genoa, Italy; 7Department of Surgery, University of Turin Medical School, Turin, Italy; and 8Division of Surgery, “S. Camillo-Forlanini” Hospital, Rome, Italy (11%) of transient postoperative hypocalcemia. The probe was 99m This study evaluated the accuracy of 99mTc-sestamibi scintigra- of little help in patients with concomitant Tc-sestamibi–avid phy and neck ultrasonography in patients with primary hyper- thyroid nodules and not helpful at all in patients with negative parathyroidism (PHPT) and the role of intraoperative hand-held scan findings preoperatively. IQPTH measurement helped to ␥-probes in minimally invasive radioguided surgery (MIRS) of disclose some cases of multigland parathyroid disease. Con- patients with a high likelihood of a solitary parathyroid adenoma clusion: 99mTc-Sestamibi scintigraphy, especially if combined (PA). The study was undertaken under the aegis of the Italian with neck ultrasonography, is highly accurate in selecting PHPT Study Group on Radioguided Surgery and Immunoscintigraphy candidates for MIRS. -

Minimally Invasive Parathyroidectomy Versus Bilateral Neck Exploration for Primary Hyperparathyroidism
Minimally Invasive Parathyroidectomy Versus Bilateral Neck Exploration for Primary Hyperparathyroidism Amanda M. Laird, MD*, Steven K. Libutti, MD KEYWORDS Primary hyperparathyroidism Parathyroidectomy Intraoperative parathyroid hormone Surgery Minimally invasive parathyroidectomy KEY POINTS The gold-standard surgical management of primary hyperparathyroidism (10HPT) is cer- vical exploration and identification of all 4 parathyroid glands. Imaging techniques, including ultrasound, sestamibi scans, and 4D-CT scans, have made identification of single parathyroid adenomas possible. Intraoperative parathyroid hormone (PTH) monitoring is a method to confirm biochemical cure before a patient leaves the operating room. There is some debate surrounding optimal surgical management of 10HPT because cure rates between minimally invasive parathyroidectomy (MIP) and bilateral neck exploration (BNE) are equivalent. Advantages of MIP include reduced operative time, reduced recovery time, less postop- erative pain, and lower complication rate with respect to injury to parathyroid glands and recurrent laryngeal nerves. INTRODUCTION 10HPT is a common disease, with a prevalence as high as 3%.1 Many advances in the surgical management of 10HPT have been made since the first parathyroidectomy was performed by Felix Mandl in 1925.2 Traditional surgical management consists of identification of all 4 parathyroid glands through a transverse cervical incision.3 Bet- ter understanding of the disease, interest in the practice of endocrine neck surgery, The authors have nothing to disclose. Montefiore Medical Center/Albert Einstein College of Medicine, Greene Medical Arts Pavilion, 3400 Bainbridge Avenue, 4th Floor, Bronx, NY 10467, USA * Corresponding author. E-mail address: [email protected] Surg Oncol Clin N Am 25 (2016) 103–118 http://dx.doi.org/10.1016/j.soc.2015.08.012 surgonc.theclinics.com 1055-3207/16/$ – see front matter Ó 2016 Elsevier Inc. -
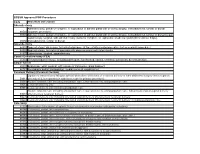
Code Procedure Description Adrenalectomy 60540 Adrenalectomy, Partial Or Complete, Or Exploration of Adrenal Gland with Or Witho
BCBSM Approved POP Procedures Code Procedure Description Adrenalectomy Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal 60540 (separate procedure) 60545 Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal (separate procedure); with excision of adjacent retroperitoneal tumor Laparoscopy, surgical, with adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, 60650 transabdominal, lumbar or dorsal Appendectomy 44955 Appendectomy; when done for indicated purpose at time of other major procedure (not as separate procedure) 44960 Appendectomy; for ruptured appendix with abscess or generalized peritonitis 44970 Laparoscopy, surgical, appendectomy Carotid Endarterectomy (CEA) 35301 Thromboendarterectomy, including patch graft, if performed; carotid, vertebral, subclavian, by neck incision Carpal Tunnel 29848 Endoscopy, wrist, surgical, with release of transverse carpal ligament 64721 Neuroplasty and/or transposition; median nerve at carpal tunnel Cesarean Delivery (Cesarean Section) Ligation or transection of fallopian tube(s) when done at the time of cesarean delivery or intra-abdominal surgery (not a separate 58611 procedure) (List separately in addition to code for primary procedure) 59510 Routine obstetric care including antepartum care, cesarean delivery, and postpartum care 59514 Cesarean delivery only 59515 Cesarean delivery only; including postpartum care -

Adrenalectomy Patient Information Leaflet
Adrenalectomy Patient information leaflet UHB is a no smoking Trust To see all of our current patient information leaflets please visit www.uhb.nhs.uk/patient-information-leaflets.htm What is an adrenalectomy? An adrenalectomy (ad-renal-ect-omy) is an operation to remove one or both of the adrenal glands. The adrenal glands sit above the kidneys. Right Left adrenal adrenal gland gland Kidney Kidney The main role of the adrenal glands is to release hormones into the body. The main hormones released are stress related hormones (cortisol, noradrenaline and adrenaline), hormones that regulate metabolism, hormones that affect immune system function, androgens (sex hormones) and hormones for saltwater balance (aldosterone). 2 | PI18/1289/03 Adrenalectomy An adrenalectomy can be done: • ‘Open’ with one large surgical cut below the ribcage • Or ‘laparoscopic’ which involves four smaller cuts being made allowing the inside of the abdomen to be seen using a camera Some laparoscopic operations may have be converted to ‘open’ at the time of the surgery due to the surgeon not being able to see the inside of the abdomen clearly enough (about 5% of cases). The surgery is performed under general anaesthetic so you will be asleep and will not feel any pain. The surgery normally takes 1–2 hours. The adrenal gland(s) will be sent to a pathologist after it is removed for further tests in a laboratory using a microscope. Why is an adrenalectomy performed? The adrenal gland(s) need to be removed if there is a mass/ tumour in the gland(s). An adrenalectomy is performed if: 1. -

Analysis of the Role of Thyroidectomy and Thymectomy in the Surgical Treatment of Secondary Hyperparathyroidism
Am J Otolaryngol 40 (2019) 67–69 Contents lists available at ScienceDirect Am J Otolaryngol journal homepage: www.elsevier.com/locate/amjoto Analysis of the role of thyroidectomy and thymectomy in the surgical ☆ treatment of secondary hyperparathyroidism T Mateus R. Soares, Graziela V. Cavalcanti, Ricardo Iwakura, Leandro J. Lucca, Elen A. Romão, ⁎ Luiz C. Conti de Freitas Division of Head and Neck Surgery, Department of Ophthalmology, Otolaryngology, Head and Neck Surgery, Ribeirao Preto Medical School, University of Sao Paulo, Brazil ARTICLE INFO ABSTRACT Keywords: Purpose: Parathyroidectomy can be subtotal or total with an autograft for the treatment of renal hyperpar- Parathyroidectomy athyroidism. In both cases, it may be extended with bilateral thymectomy and total or partial thyroidectomy. Hyperparathyroidism Thymectomy may be recommended in combination with parathyroidectomy in order to prevent mediastinal Thymectomy recurrence. Also, the occurrence of thyroid disease observed in patients with hyperparathyroidism is poorly Thyroidectomy understood and the incidence of cancer is controversial. The aim of the present study was to report the ex- perience of a single center in the surgical treatment of renal hyperparathyroidism and to analyse the role of thyroid and thymus surgery in association with parathyroidectomy. Materials and methods: We analysed parathyroid surgery data, considering patient demographics, such as age and gender, and surgical procedure data, such as type of hyperparathyroidism, associated thyroid or thymus surgery, surgical duration and mediastinal recurrence. Histopathological results of thyroid and thymus samples were also analysed. Results: Medical records of 109 patients who underwent parathyroidectomy for secondary hyperparathyroidism were reviewed. On average, thymectomy did not have impact on time of parathyroidectomy (p = 0.62) even when thyroidectomy was included (p = 0.91). -

Use of Dexmedetomidine in a Parturient with Multiple Endocrine Neoplasia Type 2A Undergoing Adrenalectomy and Thyroidectomy
PRACTICE CASE REPORT Use of Dexmedetomidine in a Parturient With Multiple Endocrine Neoplasia Type 2A Undergoing Adrenalectomy and Thyroidectomy: A Case Report Amanda L. Faulkner, MD, Eric Swanson, MD, Thomas L. McLarney, MD, Cortney Y. Lee, MD, and Annette Rebel, MD * * * † * 08/15/2018 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3yRlXg5VZA8uqNuqWFo8dRhJiNZRTFLkCeIa0nEMHM2KbYm37VRaE3A== by https://journals.lww.com/aacr from Downloaded Dexmedetomidine is a selective α2-agonist, frequently used in perioperative medicine as anes- thesia adjunct. The medication carries a Food and Drug Administration pregnancy category C Downloaded designation and is therefore rarely used for parturients undergoing nonobstetric surgery. We are reporting the use of dexmedetomidine in the anesthetic management of a parturient undergoing minimally invasive unilateral adrenalectomy for pheochromocytoma during the second trimester from https://journals.lww.com/aacr of pregnancy. Additionally, because of the multiple endocrine neoplasia type 2A constellation with diagnosis of medullary thyroid cancer, the patient underwent a total thyroidectomy 1 week after the adrenalectomy. (A&A Practice. XXX;XXX:00–00.) exmedetomidine is a selective α2-agonist, fre- CASE REPORT by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3yRlXg5VZA8uqNuqWFo8dRhJiNZRTFLkCeIa0nEMHM2KbYm37VRaE3A== quently used in perioperative medicine. It has A 34-year-old gravida 3 para 2 woman (body weight, 61 Dfound favor in this setting because of its sedative kg; -

Surgical Indications and Techniques for Adrenalectomy Review
THE MEDICAL BULLETIN OF SISLI ETFAL HOSPITAL DOI: 10.14744/SEMB.2019.05578 Med Bull Sisli Etfal Hosp 2020;54(1):8–22 Review Surgical Indications and Techniques for Adrenalectomy Mehmet Uludağ,1 Nurcihan Aygün,1 Adnan İşgör2 1Department of General Surgery, Sisli Hamidiye Etfal Training and Research Hospital, Istanbul, Turkey 2Department of General Surgery, Bahcesehir University Faculty of Medicine, Istanbul, Turkey Abstract Indications for adrenalectomy are malignancy suspicion or malignant tumors, non-functional tumors with the risk of malignancy and functional adrenal tumors. Regardless of the size of functional tumors, they have surgical indications. The hormone-secreting adrenal tumors in which adrenalectomy is indicated are as follows: Cushing’s syndrome, arises from hypersecretion of glucocorticoids produced in fasciculata adrenal cortex, Conn’s syndrome, arises from an hypersecretion of aldosterone produced by glomerulosa adrenal cortex, and Pheochromocytomas that arise from adrenal medulla and produce catecholamines. Sometimes, bilateral adre- nalectomy may be required in Cushing's disease due to pituitary or ectopic ACTH secretion. Adenomas arise from the reticularis layer of the adrenal cortex, which rarely releases too much adrenal androgen and estrogen, may also develop and have an indication for adrenalectomy. Adrenal surgery can be performed by laparoscopic or open technique. Today, laparoscopic adrenalectomy is the gold standard treatment in selected patients. Laparoscopic adrenalectomy can be performed transperitoneally or retroperitoneoscopi- cally. Both approaches have their advantages and disadvantages. In the selection of the surgery type, the experience and habits of the surgeon are also important, along with the patient’s characteristics. The most common type of surgery performed in the world is laparoscopic transabdominal lateral adrenalectomy, which most surgeons are more familiar with. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

1 Annex 2. AHRQ ICD-9 Procedure Codes 0044 PROC-VESSEL
Annex 2. AHRQ ICD-9 Procedure Codes 0044 PROC-VESSEL BIFURCATION OCT06- 0201 LINEAR CRANIECTOMY 0050 IMPL CRT PACEMAKER SYS 0202 ELEVATE SKULL FX FRAGMNT 0051 IMPL CRT DEFIBRILLAT SYS 0203 SKULL FLAP FORMATION 0052 IMP/REP LEAD LF VEN SYS 0204 BONE GRAFT TO SKULL 0053 IMP/REP CRT PACEMAKR GEN 0205 SKULL PLATE INSERTION 0054 IMP/REP CRT DEFIB GENAT 0206 CRANIAL OSTEOPLASTY NEC 0056 INS/REP IMPL SENSOR LEAD OCT06- 0207 SKULL PLATE REMOVAL 0057 IMP/REP SUBCUE CARD DEV OCT06- 0211 SIMPLE SUTURE OF DURA 0061 PERC ANGIO PRECEREB VES (OCT 04) 0212 BRAIN MENINGE REPAIR NEC 0062 PERC ANGIO INTRACRAN VES (OCT 04) 0213 MENINGE VESSEL LIGATION 0066 PTCA OR CORONARY ATHER OCT05- 0214 CHOROID PLEXECTOMY 0070 REV HIP REPL-ACETAB/FEM OCT05- 022 VENTRICULOSTOMY 0071 REV HIP REPL-ACETAB COMP OCT05- 0231 VENTRICL SHUNT-HEAD/NECK 0072 REV HIP REPL-FEM COMP OCT05- 0232 VENTRI SHUNT-CIRCULA SYS 0073 REV HIP REPL-LINER/HEAD OCT05- 0233 VENTRICL SHUNT-THORAX 0074 HIP REPL SURF-METAL/POLY OCT05- 0234 VENTRICL SHUNT-ABDOMEN 0075 HIP REP SURF-METAL/METAL OCT05- 0235 VENTRI SHUNT-UNINARY SYS 0076 HIP REP SURF-CERMC/CERMC OCT05- 0239 OTHER VENTRICULAR SHUNT 0077 HIP REPL SURF-CERMC/POLY OCT06- 0242 REPLACE VENTRICLE SHUNT 0080 REV KNEE REPLACEMT-TOTAL OCT05- 0243 REMOVE VENTRICLE SHUNT 0081 REV KNEE REPL-TIBIA COMP OCT05- 0291 LYSIS CORTICAL ADHESION 0082 REV KNEE REPL-FEMUR COMP OCT05- 0292 BRAIN REPAIR 0083 REV KNEE REPLACE-PATELLA OCT05- 0293 IMPLANT BRAIN STIMULATOR 0084 REV KNEE REPL-TIBIA LIN OCT05- 0294 INSERT/REPLAC SKULL TONG 0085 RESRF HIPTOTAL-ACET/FEM