Use of Dexmedetomidine in a Parturient with Multiple Endocrine Neoplasia Type 2A Undergoing Adrenalectomy and Thyroidectomy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

When Is It Minimally Invasive?
ORIGINAL ARTICLE Incision Length for Standard Thyroidectomy and Parathyroidectomy When Is It Minimally Invasive? Laurent Brunaud, MD; Rasa Zarnegar, MD; Nobuyuki Wada, MD; Philip Ituarte, PhD; Orlo H. Clark, MD; Quan-Yang Duh, MD Hypothesis: Current techniques for open conven- parathyroidectomy (PϽ.001). It was 4.1 cm for bilateral tional thyroidectomy or parathyroidectomy have evolved parathyroid exploration, but was reduced to 3.2 and 2.8 to enable a shorter incision (main proposition), and the cm for unilateral (PϽ.001) and focal (PϽ.001) explora- length of the incision is influenced by objective factors. tions, respectively. By multiple regression analysis, thy- roid specimen volume and patient body mass index were Design: Case series. independent predictors of incision length in thyroidec- tomy. Extent of exploration and resident training level Setting: University referral center. were independent predictors of incision length in parathyroidectomy. Patients and Intervention: Retrospective study of the most recent 200 primary consecutive routine thyroid and Conclusions: Current techniques for open conven- parathyroid operations (excluding neck dissections). tional thyroidectomy or parathyroidectomy have evolved to enable a shorter incision. Thyroid volume, patient body Main Outcome Measures: The length of incision was mass index, extent of the planned parathyroid explora- routinely measured with a ruler before the incision. tion, and the resident clinical training stage are impor- Univariate and multivariate analysis was performed to dis- tant variables for incision length in open operation and tinguish variables affecting length of incision. should be taken into account when minimally invasive thyroidectomy and parathyroidectomy are evaluated. Results: Mean length of the incision was 5.5 cm for to- tal thyroidectomy, 4.6 cm for lobectomy, and 3.5 cm for Arch Surg. -

HP Layout 1-21-04 to Print
Winter 2004 Department of Surgery healthpoints NewYork-Presbyterian ALL THE POSSIBILITIES OF MODERN MEDICINEE DIABETES Knowledge is Power ALSO IN THIS ISSUE: in a Complex Disease Approximately 17 million people in the United States have the disease. While an estimated 11.1 million have been diagnosed, 5.9 million people remain unaware that POSITRON EMISSION they have the condition. It is the fifth leading cause of death by disease in the U.S.— TOMOGRAPHY (PET) contributing to the deaths of more than 210,000 Americans each year. And its origin Approved for the Fight remains a mystery. Against Thyroid Cancer Diabetes is a complex disease which results from the body’s inability to create or page 2 properly use insulin. A hormone produced by the pancreas, insulin helps the body convert sugar, starches, and other food into energy. If the body doesn’t make enough insulin or if the insulin doesn’t work the way it should, glucose (sugar) cannot enter into the body’s cells. Instead, ISLET CELL glucose remains in the TRANSPLANTATION bloodstream, raising the The Search for a Cure blood sugar level and for Type 1 Diabetes ultimately causing page 7 diabetes. The signs of diabetes are often subtle, which can make detection of the disease a greater AIDING THE HEART challenge. Some Medicare Approves common symptoms LVADs as Destination include excessive thirst, Diabetes strikes people of all ages, races, and genders. Therapy frequent urination, page 8 unusual weight loss, increased fatigue, slow wound healing, extreme hunger, and blurry vision. However, individuals who experience none of these signs may still have diabetes. -
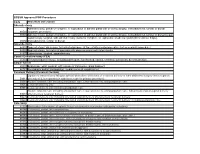
Code Procedure Description Adrenalectomy 60540 Adrenalectomy, Partial Or Complete, Or Exploration of Adrenal Gland with Or Witho
BCBSM Approved POP Procedures Code Procedure Description Adrenalectomy Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal 60540 (separate procedure) 60545 Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal (separate procedure); with excision of adjacent retroperitoneal tumor Laparoscopy, surgical, with adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, 60650 transabdominal, lumbar or dorsal Appendectomy 44955 Appendectomy; when done for indicated purpose at time of other major procedure (not as separate procedure) 44960 Appendectomy; for ruptured appendix with abscess or generalized peritonitis 44970 Laparoscopy, surgical, appendectomy Carotid Endarterectomy (CEA) 35301 Thromboendarterectomy, including patch graft, if performed; carotid, vertebral, subclavian, by neck incision Carpal Tunnel 29848 Endoscopy, wrist, surgical, with release of transverse carpal ligament 64721 Neuroplasty and/or transposition; median nerve at carpal tunnel Cesarean Delivery (Cesarean Section) Ligation or transection of fallopian tube(s) when done at the time of cesarean delivery or intra-abdominal surgery (not a separate 58611 procedure) (List separately in addition to code for primary procedure) 59510 Routine obstetric care including antepartum care, cesarean delivery, and postpartum care 59514 Cesarean delivery only 59515 Cesarean delivery only; including postpartum care -

Adrenalectomy Patient Information Leaflet
Adrenalectomy Patient information leaflet UHB is a no smoking Trust To see all of our current patient information leaflets please visit www.uhb.nhs.uk/patient-information-leaflets.htm What is an adrenalectomy? An adrenalectomy (ad-renal-ect-omy) is an operation to remove one or both of the adrenal glands. The adrenal glands sit above the kidneys. Right Left adrenal adrenal gland gland Kidney Kidney The main role of the adrenal glands is to release hormones into the body. The main hormones released are stress related hormones (cortisol, noradrenaline and adrenaline), hormones that regulate metabolism, hormones that affect immune system function, androgens (sex hormones) and hormones for saltwater balance (aldosterone). 2 | PI18/1289/03 Adrenalectomy An adrenalectomy can be done: • ‘Open’ with one large surgical cut below the ribcage • Or ‘laparoscopic’ which involves four smaller cuts being made allowing the inside of the abdomen to be seen using a camera Some laparoscopic operations may have be converted to ‘open’ at the time of the surgery due to the surgeon not being able to see the inside of the abdomen clearly enough (about 5% of cases). The surgery is performed under general anaesthetic so you will be asleep and will not feel any pain. The surgery normally takes 1–2 hours. The adrenal gland(s) will be sent to a pathologist after it is removed for further tests in a laboratory using a microscope. Why is an adrenalectomy performed? The adrenal gland(s) need to be removed if there is a mass/ tumour in the gland(s). An adrenalectomy is performed if: 1. -

Advances in Risk-Oriented Surgery for Multiple Endocrine Neoplasia Type 2
25 2 Endocrine-Related A Machens et al. Advances in risk-oriented 25:2 T41–T52 Cancer surgery for MEN2 THEMATIC REVIEW Advances in risk-oriented surgery for multiple endocrine neoplasia type 2 Andreas Machens1 and Henning Dralle2 1Department of General, Visceral and Vascular Surgery, Martin Luther University Halle-Wittenberg, Halle, Saale, Germany 2Department of General, Visceral and Transplantation Surgery, Section of Endocrine Surgery, University of Duisburg-Essen, Essen, Germany Correspondence should be addressed to A Machens: [email protected] This paper is part of a thematic review section on 25 Years of RET and MEN2. The guest editors for this section were Lois Mulligan and Frank Weber. Abstract Genetic association studies hinge on definite clinical case definitions of the disease of Key Words interest. This is why more penetrant mutations were overrepresented in early multiple f biochemical screening endocrine neoplasia type 2 (MEN2) studies, whereas less penetrant mutations went f DNA-based screening underrepresented. Enrichment of genetic association studies with advanced disease f RET proto-oncogene may produce a flawed understanding of disease evolution, precipitating far-reaching f gene test surgical strategies like bilateral total adrenalectomy and 4-gland parathyroidectomy in f gene carrier MEN2. The insight into the natural course of the disease gleaned over the past 25 years f multiple endocrine caused a paradigm shift in MEN2: from the removal of target organs at the expense of neoplasia type 2A greater operative -

Analysis of the Role of Thyroidectomy and Thymectomy in the Surgical Treatment of Secondary Hyperparathyroidism
Am J Otolaryngol 40 (2019) 67–69 Contents lists available at ScienceDirect Am J Otolaryngol journal homepage: www.elsevier.com/locate/amjoto Analysis of the role of thyroidectomy and thymectomy in the surgical ☆ treatment of secondary hyperparathyroidism T Mateus R. Soares, Graziela V. Cavalcanti, Ricardo Iwakura, Leandro J. Lucca, Elen A. Romão, ⁎ Luiz C. Conti de Freitas Division of Head and Neck Surgery, Department of Ophthalmology, Otolaryngology, Head and Neck Surgery, Ribeirao Preto Medical School, University of Sao Paulo, Brazil ARTICLE INFO ABSTRACT Keywords: Purpose: Parathyroidectomy can be subtotal or total with an autograft for the treatment of renal hyperpar- Parathyroidectomy athyroidism. In both cases, it may be extended with bilateral thymectomy and total or partial thyroidectomy. Hyperparathyroidism Thymectomy may be recommended in combination with parathyroidectomy in order to prevent mediastinal Thymectomy recurrence. Also, the occurrence of thyroid disease observed in patients with hyperparathyroidism is poorly Thyroidectomy understood and the incidence of cancer is controversial. The aim of the present study was to report the ex- perience of a single center in the surgical treatment of renal hyperparathyroidism and to analyse the role of thyroid and thymus surgery in association with parathyroidectomy. Materials and methods: We analysed parathyroid surgery data, considering patient demographics, such as age and gender, and surgical procedure data, such as type of hyperparathyroidism, associated thyroid or thymus surgery, surgical duration and mediastinal recurrence. Histopathological results of thyroid and thymus samples were also analysed. Results: Medical records of 109 patients who underwent parathyroidectomy for secondary hyperparathyroidism were reviewed. On average, thymectomy did not have impact on time of parathyroidectomy (p = 0.62) even when thyroidectomy was included (p = 0.91). -

Surgical Indications and Techniques for Adrenalectomy Review
THE MEDICAL BULLETIN OF SISLI ETFAL HOSPITAL DOI: 10.14744/SEMB.2019.05578 Med Bull Sisli Etfal Hosp 2020;54(1):8–22 Review Surgical Indications and Techniques for Adrenalectomy Mehmet Uludağ,1 Nurcihan Aygün,1 Adnan İşgör2 1Department of General Surgery, Sisli Hamidiye Etfal Training and Research Hospital, Istanbul, Turkey 2Department of General Surgery, Bahcesehir University Faculty of Medicine, Istanbul, Turkey Abstract Indications for adrenalectomy are malignancy suspicion or malignant tumors, non-functional tumors with the risk of malignancy and functional adrenal tumors. Regardless of the size of functional tumors, they have surgical indications. The hormone-secreting adrenal tumors in which adrenalectomy is indicated are as follows: Cushing’s syndrome, arises from hypersecretion of glucocorticoids produced in fasciculata adrenal cortex, Conn’s syndrome, arises from an hypersecretion of aldosterone produced by glomerulosa adrenal cortex, and Pheochromocytomas that arise from adrenal medulla and produce catecholamines. Sometimes, bilateral adre- nalectomy may be required in Cushing's disease due to pituitary or ectopic ACTH secretion. Adenomas arise from the reticularis layer of the adrenal cortex, which rarely releases too much adrenal androgen and estrogen, may also develop and have an indication for adrenalectomy. Adrenal surgery can be performed by laparoscopic or open technique. Today, laparoscopic adrenalectomy is the gold standard treatment in selected patients. Laparoscopic adrenalectomy can be performed transperitoneally or retroperitoneoscopi- cally. Both approaches have their advantages and disadvantages. In the selection of the surgery type, the experience and habits of the surgeon are also important, along with the patient’s characteristics. The most common type of surgery performed in the world is laparoscopic transabdominal lateral adrenalectomy, which most surgeons are more familiar with. -

Pituitary Apoplexy After Subtotal Thyroidectomy In
CASE REPORT Pituitary Apoplexy after Subtotal Thyroidectomy in an Acromegalic Patient with a Large Goiter Kazunobu Kato, Masakazu Nobori*, Yoshihiro Miyauchi, Motoki Ohnisi, Shyoji Yoshida, Shigeru Oya**, Shin Tomita** and Tomoshige Kino*** A case of pituitary apoplexy occurring after subtotal thyroidectomy in an acromegalic woman with a large adenomatous goiter is described. The patient had severe apnea because the large goiter was causing airway compression. Prior to the planned hypophysectomy, a subtotal thyroidectomy was performed to relieve tracheal stenosis. Shortly after the operation, the patient developed a headache that lasted for several days. The serum levels of growth hormoneand somatomedin-C spontaneously normalized seventeen days after this episode and have remained normal for two years. Pituitary apoplexy was thought to have caused the observed results without deterioration of the pituitary function. (Internal Medicine 35: 472-477, 1996) Key words: acromegaly, thyroid goiter, airway obstruction, diabetes mellitus Introduction and noticed enlargement of her hands. In February 1991, thirst and general fatigue developed and she consulted a local physi- Pituitary apoplexy is an uncommonevent, sometimes fatal, cian and was found to have diabetes mellitus and an abnormal but sometimes it induces complete reversal of acromegaly. It mass adjacent to the right side of the trachea, according to chest occurs in various situations, such as during the course of drug X-ray films. The patient, an unmarried desk clerk, was referred therapy for pituitary adenoma,during pregnancy, or after to us, with the complaint ofdyspnea that was moresevere lying cholecystectomy. However,there are no reports documenting down than in the sitting position. She had excessive nocturnal pituitary apoplexy after thyroidectomy. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Volume-Based Trends in Thyroid Surgery
ORIGINAL ARTICLE Volume-Based Trends in Thyroid Surgery Christine G. Gourin, MD; Ralph P. Tufano, MD; Arlene A. Forastiere, MD; Wayne M. Koch, MD; Timothy M. Pawlik, MD, MPH; Robert E. Bristow, MD Objective: To characterize contemporary patterns of thy- pitalization (0.44; PϽ.001), and had a lower incidence roid surgical care and variables associated with access to of recurrent laryngeal nerve injury (0.46; P=.002), hy- high-volume care. pocalcemia (0.62; PϽ.001), and thyroid cancer surgery (0.89; P=.01). After controlling for other variables, thy- Design: Cross-sectional analysis. roid surgery in 2000-2009 was associated with high- volume surgeons (OR, 1.76; PϽ.001), high-volume hos- Setting: Maryland Health Service Cost Review Com- pitals (2.93; P Ͻ .001), total thyroidectomy (2.67; mission database. PϽ.001), and neck dissection (1.28; P=.02) but was less likely to be performed for cancer (0.83; PϽ.001). Patients: Adults who underwent surgery for thyroid dis- ease in Maryland between January 1, 1990, and July 1, Conclusions: The proportion of thyroid surgical pro- 2009. cedures performed by high-volume surgeons and in high- volume hospitals increased significantly from 1990- Results: Overall, 21 270 thyroid surgical procedures were 1999 to 2000-2009, with an increase in total performed by 1034 surgeons at 51 hospitals. Proce- thyroidectomy and neck dissection. Surgeon volume was dures performed by high-volume surgeons increased from significantly associated with complication rates. Thy- 15.7% in 1990-1999 to 30.9% in 2000-2009 (odds ratio roid cancer surgery was less likely to be performed by [OR], 3.69; PϽ.001), while procedures performed at high- high-volume surgeons and in 2000-2009 despite an in- volume hospitals increased from 11.9% to 22.7% (3.46; crease in surgical cases. -

Thyroid & Parathyroid Surgery
Thyroid & Parathyroid Surgery – Frequently Asked Questions How long will the operation take? What about neck stiffness and exercises? Thyroid and parathyroid operations generally take between one to Some neck stiffness is common as a result of the prolonged three hours. extension (backward tilting) of the head under the anaesthetic. The exercises recommended will reduce it but it may last for some Will I need a general anaesthetic? weeks and require physiotherapy as well. This type of surgery requires a general anaesthetic in order to stop Will my parathyroid glands be taken out with my thyroid? muscle movement during the delicate dissection. Often the anaesthetic is supplemented by local anaesthetic or a nerve block, If you are having thyroid surgery ("thyroidectomy") then every this may result in you having a numb face and ear for 24 hours attempt is made to preserve all your parathyroid glands. Mostly afterwards. they are left in place with their blood supply attached but, if that is not technically possible, they may need to be removed and How long will my incision be and where will it be placed? transplanted into the adjacent muscle. Sometimes very small parathyroid glands are buried under the thyroid capsule and For open thyroid or parathyroid surgery the scar is a curved line in cannot be identified at operation and so get taken out with the the "collar" position, about 2cm above the collar bone. The length thyroid specimen. Transplanted parathyroid glands take between varies depending on the size of the lump removed. For minimally 6 weeks to 6 months to recover, however the body can generally invasive surgery the scar is only 2 to 3cm long and is placed on get by with just part of one parathyroid gland if necessary. -
Thyroidectomy –
Thyroidectomy – an operation to remove all or part of the thyroid gland Information for patients page 2 What is the thyroid gland? The thyroid gland is an endocrine gland which makes hormones that are released into the bloodstream. These hormones affect cells and tissues in other parts of the body and help them to function normally. The thyroid is made up of two lobes, each about half the size of a plum. The two lobes lie on either side of your windpipe, with the gland as a whole lying just below your Adam’s apple. The thyroid gland produces three hormones, that are released into the bloodstream: • thyroxine, often called T4 • triiodothyronine, often called T3. In the body, T4 is converted into T3 and this is what influences the way cells and tissues work. • calcitonin – this is involved in controlling calcium levels in the blood. With medullary thyroid cancer (MTC), too much calcitonin is produced, however this does not lead to any significant change in calcium levels. Thyroxine and T3 can both be replaced by medication and the body can function perfectly well with little or no calcitonin. Thyroid hormones T3 and T4 help to control the speed of body processes – otherwise known as your metabolic rate. If too much of these thyroid hormones is released, your body starts to work faster than normal and you develop ‘hyperthyroidism’. This would make you feel overactive and anxious, hungrier than usual, and you would lose weight. However, if too little of these thyroid hormones is produced, your body will start to work slower than normal and you develop ‘hypothyroidism’.