Surgical Indications and Techniques for Adrenalectomy Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Expression Pattern of Delta-Like 1 Homolog in Developing Sympathetic Neurons and Chromaffin Cells
Published in "Gene Expression Patterns 30: 49–54, 2018" which should be cited to refer to this work. Expression pattern of delta-like 1 homolog in developing sympathetic neurons and chromaffin cells ∗ Tehani El Faitwria,b, Katrin Hubera,c, a Institute of Anatomy & Cell Biology, Albert-Ludwigs-University Freiburg, Albert-Str. 17, 79104, Freiburg, Germany b Department of Histology and Anatomy, Faculty of Medicine, Benghazi University, Benghazi, Libya c Department of Medicine, University of Fribourg, Route Albert-Gockel 1, 1700, Fribourg, Switzerland ABSTRACT Keywords: Delta-like 1 homolog (DLK1) is a member of the epidermal growth factor (EGF)-like family and an atypical notch Sympathetic neurons ligand that is widely expressed during early mammalian development with putative functions in the regulation Chromaffin cells of cell differentiation and proliferation. During later stages of development, DLK1 is downregulated and becomes DLK1 increasingly restricted to specific cell types, including several types of endocrine cells. DLK1 has been linked to Adrenal gland various tumors and associated with tumor stem cell features. Sympathoadrenal precursors are neural crest de- Organ of Zuckerkandl rived cells that give rise to either sympathetic neurons of the autonomic nervous system or the endocrine Development ffi Neural crest chroma n cells located in the adrenal medulla or extraadrenal positions. As these cells are the putative cellular Phox2B origin of neuroblastoma, one of the most common malignant tumors in early childhood, their molecular char- acterization is of high clinical importance. In this study we have examined the precise spatiotemporal expression of DLK1 in developing sympathoadrenal cells. We show that DLK1 mRNA is highly expressed in early sympa- thetic neuron progenitors and that its expression depends on the presence of Phox2B. -

Radiotherapy of Malignant Pheochromocytoma—A Case Report
Case Report Page 1 of 7 Radiotherapy of malignant pheochromocytoma—a case report Chi-Yuan Yeh Department of Radiation Oncology, Tungs’ Taichung Metroharbor Hospital, Taichung, Taiwan Correspondence to: Department of Radiation Oncology, Tungs’ Taichung Metroharbor Hospital, No.699, Sec. 8, Taiwan Blvd., Taichung City 435, Taiwan. Email: [email protected]. Abstract: Pheochromocytomas (PCC) are rare tumors with an estimated incidence of 0.4 to 9.5 cases per 1 million per year. About 5–26% of PCC are malignant and presents with metastasis, for which there is currently no effective therapy. The treatment of choice is for PCC is radical surgery to reduce tumor burden, to provide symptomatic relief of catecholamine excess although complete eradication of the lesions is often not feasible. A number of case reports have been published on the role of radiotherapy for the treatment of PCC. Here we present a 53-year-old male stage III malignant PCC patient who received postoperative adjuvant radiotherapy. A review of current literature is also presented. Keywords: Radiotherapy; pheochromocytoma (PCC); malignant pheochromocytoma; hypertension Received: 12 December 2018; Accepted: 12 August 2019; Published: 27 August 2019. doi: 10.21037/tro.2019.08.02 View this article at: http://dx.doi.org/10.21037/tro.2019.08.02 Introduction reaction confirmed PCC. The term PCC was derived from the Greek words Pheochromocytomas (PCC) and paragangliomas (PGL) phaios (“dusky”), chroma (“color”), and cytoma (“tumor”). are rare catecholamine-secreting tumors that arise from The dark staining reaction of PCC tumor was caused by the chromaffin cells of the adrenal medulla and the sympathetic oxidation of intracellular catecholamines when stained with ganglia respectively. -

Endocrine Surgery Goals and Objectives
Lenox Hill Hospital Department of Surgery Endocrine Surgery Goals and Objectives Medical Knowledge and Patient Care: Residents must demonstrate knowledge and application of the pathophysiology and epidemiology of the diseases listed below for this rotation, with the pertinent clinical and laboratory findings, differential diagnosis and therapeutic options including preventive measures, and procedural knowledge. They must show that they are able to gather accurate and relevant information using medical interviewing, physical examination, appropriate diagnostic workup, and use of information technology. They must be able to synthesize and apply information in the clinical setting to make informed recommendations about preventive, diagnostic and therapeutic options, based on clinical judgement, scientific evidence, and patient preferences. They should be able to prescribe, perform, and interpret surgical procedures listed below for this rotation. All Residents are expected to understand: 1. Normal physiology and anatomy of the thyroid glands. 2. Normal physiology and anatomy of the parathyroid glands. 3. Normal physiology and anatomy of the adrenal glands 4. Normal physiology of the pancreatic neuroendocrine cells. 5. Normal physiology of the pituitary gland. Disease-Based Learning Objectives: Hyperfunctioning Thyroid and Hypothyroid State: 1. Physiology of Grave’s disease and toxic goiter. 2. Management of a patient in hyperthyroid storm. 3. Medical and surgical treatment options for hyperthyroidism. 4. Physiology of Hashimoto’s thyroiditis and hypothyroidism. Thyroid Neoplasm: 1. Workup of a cold thyroid nodule. 2. Surgical management of papillary, follicular, medullary, and anaplastic thyroid carcinoma. 3. Adjuvant therapy for thyroid neoplasms. 4. Postoperative medical management and long-term follow-up of thyroid cancer. Hyperparathyroidism: 1. Diagnosis and work-up of hypercalcemia and primary, secondary, and tertiary hyperparathyroidism. -
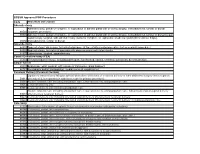
Code Procedure Description Adrenalectomy 60540 Adrenalectomy, Partial Or Complete, Or Exploration of Adrenal Gland with Or Witho
BCBSM Approved POP Procedures Code Procedure Description Adrenalectomy Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal 60540 (separate procedure) 60545 Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal (separate procedure); with excision of adjacent retroperitoneal tumor Laparoscopy, surgical, with adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, 60650 transabdominal, lumbar or dorsal Appendectomy 44955 Appendectomy; when done for indicated purpose at time of other major procedure (not as separate procedure) 44960 Appendectomy; for ruptured appendix with abscess or generalized peritonitis 44970 Laparoscopy, surgical, appendectomy Carotid Endarterectomy (CEA) 35301 Thromboendarterectomy, including patch graft, if performed; carotid, vertebral, subclavian, by neck incision Carpal Tunnel 29848 Endoscopy, wrist, surgical, with release of transverse carpal ligament 64721 Neuroplasty and/or transposition; median nerve at carpal tunnel Cesarean Delivery (Cesarean Section) Ligation or transection of fallopian tube(s) when done at the time of cesarean delivery or intra-abdominal surgery (not a separate 58611 procedure) (List separately in addition to code for primary procedure) 59510 Routine obstetric care including antepartum care, cesarean delivery, and postpartum care 59514 Cesarean delivery only 59515 Cesarean delivery only; including postpartum care -

Adrenalectomy Patient Information Leaflet
Adrenalectomy Patient information leaflet UHB is a no smoking Trust To see all of our current patient information leaflets please visit www.uhb.nhs.uk/patient-information-leaflets.htm What is an adrenalectomy? An adrenalectomy (ad-renal-ect-omy) is an operation to remove one or both of the adrenal glands. The adrenal glands sit above the kidneys. Right Left adrenal adrenal gland gland Kidney Kidney The main role of the adrenal glands is to release hormones into the body. The main hormones released are stress related hormones (cortisol, noradrenaline and adrenaline), hormones that regulate metabolism, hormones that affect immune system function, androgens (sex hormones) and hormones for saltwater balance (aldosterone). 2 | PI18/1289/03 Adrenalectomy An adrenalectomy can be done: • ‘Open’ with one large surgical cut below the ribcage • Or ‘laparoscopic’ which involves four smaller cuts being made allowing the inside of the abdomen to be seen using a camera Some laparoscopic operations may have be converted to ‘open’ at the time of the surgery due to the surgeon not being able to see the inside of the abdomen clearly enough (about 5% of cases). The surgery is performed under general anaesthetic so you will be asleep and will not feel any pain. The surgery normally takes 1–2 hours. The adrenal gland(s) will be sent to a pathologist after it is removed for further tests in a laboratory using a microscope. Why is an adrenalectomy performed? The adrenal gland(s) need to be removed if there is a mass/ tumour in the gland(s). An adrenalectomy is performed if: 1. -

Advances in Risk-Oriented Surgery for Multiple Endocrine Neoplasia Type 2
25 2 Endocrine-Related A Machens et al. Advances in risk-oriented 25:2 T41–T52 Cancer surgery for MEN2 THEMATIC REVIEW Advances in risk-oriented surgery for multiple endocrine neoplasia type 2 Andreas Machens1 and Henning Dralle2 1Department of General, Visceral and Vascular Surgery, Martin Luther University Halle-Wittenberg, Halle, Saale, Germany 2Department of General, Visceral and Transplantation Surgery, Section of Endocrine Surgery, University of Duisburg-Essen, Essen, Germany Correspondence should be addressed to A Machens: [email protected] This paper is part of a thematic review section on 25 Years of RET and MEN2. The guest editors for this section were Lois Mulligan and Frank Weber. Abstract Genetic association studies hinge on definite clinical case definitions of the disease of Key Words interest. This is why more penetrant mutations were overrepresented in early multiple f biochemical screening endocrine neoplasia type 2 (MEN2) studies, whereas less penetrant mutations went f DNA-based screening underrepresented. Enrichment of genetic association studies with advanced disease f RET proto-oncogene may produce a flawed understanding of disease evolution, precipitating far-reaching f gene test surgical strategies like bilateral total adrenalectomy and 4-gland parathyroidectomy in f gene carrier MEN2. The insight into the natural course of the disease gleaned over the past 25 years f multiple endocrine caused a paradigm shift in MEN2: from the removal of target organs at the expense of neoplasia type 2A greater operative -

Use of Dexmedetomidine in a Parturient with Multiple Endocrine Neoplasia Type 2A Undergoing Adrenalectomy and Thyroidectomy
PRACTICE CASE REPORT Use of Dexmedetomidine in a Parturient With Multiple Endocrine Neoplasia Type 2A Undergoing Adrenalectomy and Thyroidectomy: A Case Report Amanda L. Faulkner, MD, Eric Swanson, MD, Thomas L. McLarney, MD, Cortney Y. Lee, MD, and Annette Rebel, MD * * * † * 08/15/2018 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3yRlXg5VZA8uqNuqWFo8dRhJiNZRTFLkCeIa0nEMHM2KbYm37VRaE3A== by https://journals.lww.com/aacr from Downloaded Dexmedetomidine is a selective α2-agonist, frequently used in perioperative medicine as anes- thesia adjunct. The medication carries a Food and Drug Administration pregnancy category C Downloaded designation and is therefore rarely used for parturients undergoing nonobstetric surgery. We are reporting the use of dexmedetomidine in the anesthetic management of a parturient undergoing minimally invasive unilateral adrenalectomy for pheochromocytoma during the second trimester from https://journals.lww.com/aacr of pregnancy. Additionally, because of the multiple endocrine neoplasia type 2A constellation with diagnosis of medullary thyroid cancer, the patient underwent a total thyroidectomy 1 week after the adrenalectomy. (A&A Practice. XXX;XXX:00–00.) exmedetomidine is a selective α2-agonist, fre- CASE REPORT by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3yRlXg5VZA8uqNuqWFo8dRhJiNZRTFLkCeIa0nEMHM2KbYm37VRaE3A== quently used in perioperative medicine. It has A 34-year-old gravida 3 para 2 woman (body weight, 61 Dfound favor in this setting because of its sedative kg; -

Ese-Ensat-Acc-Guidelines-13-5-2018
European Society of Endocrinology Clinical Practice Guidelines on the Management of Adrenocortical Carcinoma in Adults, in collaboration with the European Network for the Study of Adrenal Tumors Martin Fassnacht1,2*, Olaf M. Dekkers3,4,5, Tobias Else5, Eric Baudin7,8, Alfredo Berruti9, Ronald R. de Krijger10, 11, 12, 13, Harm R. Haak14,15, 16, Radu Mihai17, Guillaume Assie19, 20, Massimo Terzolo20* 1 Dept. of Internal Medicine I, Div. of Endocrinology and Diabetes, University Hospital, University of Würzburg, Würzburg, Germany 2 Comprehensive Cancer Center Mainfranken, University of Würzburg, Würzburg, Germany 3 Department of Clinical Epidemiology, Leiden University Medical Centre, Leiden, the Netherlands 4 Department of Clinical Endocrinology and Metabolism, Leiden University Medical Centre, Leiden, the Netherlands 5 Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus, Denmark 6 Department of Internal Medicine, Division of Metabolism, Endocrinology and Diabetes, University of Michigan, Ann Arbor, MI, USA 7 Endocrine Oncology and Nuclear Medicine, Institut Gustave Roussy, Villejuif, France 8 INSERM UMR 1185, Faculté de Médecine, Le Kremlin-Bicêtre, Université Paris Sud, Paris, France 9 Department of Medical and Surgical Specialties, Radiological Sciences, and Public Health, Medical Oncology, University of Brescia at ASST Spedali Civili, Brescia, Italy. 10 Dept. of Pathology, Erasmus MC University Medical Center, Rotterdam, The Netherlands 11 Dept. of Pathology, University Medical Center Utrecht, Utrecht, The Netherlands 12 Dept. of Pathology, Reinier de Graaf Hospital, Delft, The Netherlands 13 Princess Maxima Center for Pediatric Oncology, Utrecht, The Netherlands 14 Department of Internal Medicine, Máxima Medical Centre, Eindhoven/Veldhoven, the Netherlands 15 Maastricht University, CAPHRI School for Public Health and Primary Care, Ageing and Long-Term Care, Maastricht, the Netherlands 16 Department of Internal Medicine, Division of General Internal Medicine, Maastricht University Medical Centre+, Maastricht, the Netherlands. -

Haemorrhagic Retroperitoneal Paraganglioma
Yang et al. BMC Surg (2020) 20:304 https://doi.org/10.1186/s12893-020-00953-y CASE REPORT Open Access Haemorrhagic retroperitoneal paraganglioma initially manifesting as acute abdomen: a rare case report and literature review Yanliang Yang1, Guangzhi Wang2, Haofeng Lu1, Yaqing Liu2, Shili Ning2† and Fuwen Luo2*† Abstract Background: Paragangliomas (PGLs) are extremely rare neuroendocrine tumours arising from extra-adrenal chro- mafn cells. PGLs are clinically rare, difcult to diagnose and usually require surgical intervention. PGLs mostly present catecholamine-related symptoms. We report a case of Acute abdomen as the initial manifestation of haemorrhagic retroperitoneal PGL. There has been only one similar case reported in literature. Case presentation: We present a unique case of a 52-year-old female with acute abdomen induced by haemor- rhagic retroperitoneal PGL. The patient had a 5-h history of sudden onset of serve right lower quadrant abdominal pain radiating to the right fank and right lumbar region. Patient had classic symptoms of acute abdomen. Abdominal ultrasound revealed a large abdominal mass with a clear boundary. A Computed Tomography Angiography (CTA) of superior mesenteric artery was also performed to in the emergency department. The CTA demonstrated a large retro- peritoneal mass measured 9.0 7.3 cm with higher density inside. A provisional diagnosis of retroperitoneal tumour with haemorrhage was made. ×The patient received intravenous fuids, broad-spectrum antibiotics and somatostatin. On the 3rd day of admission, her abdominal pain was slightly relieved, but haemoglobin decreased from 10.9 to 9.4 g/ dL in 12 h suggesting that there might be active bleeding in the abdominal cavity. -

Hyperparathyroidism
HYPERPARATHYROIDISM Edited by Gonzalo Díaz-Soto and Manuel Puig-Domingo Hyperparathyroidism Edited by Gonzalo Díaz-Soto and Manuel Puig-Domingo Published by InTech Janeza Trdine 9, 51000 Rijeka, Croatia Copyright © 2012 InTech All chapters are Open Access distributed under the Creative Commons Attribution 3.0 license, which allows users to download, copy and build upon published articles even for commercial purposes, as long as the author and publisher are properly credited, which ensures maximum dissemination and a wider impact of our publications. After this work has been published by InTech, authors have the right to republish it, in whole or part, in any publication of which they are the author, and to make other personal use of the work. Any republication, referencing or personal use of the work must explicitly identify the original source. As for readers, this license allows users to download, copy and build upon published chapters even for commercial purposes, as long as the author and publisher are properly credited, which ensures maximum dissemination and a wider impact of our publications. Notice Statements and opinions expressed in the chapters are these of the individual contributors and not necessarily those of the editors or publisher. No responsibility is accepted for the accuracy of information contained in the published chapters. The publisher assumes no responsibility for any damage or injury to persons or property arising out of the use of any materials, instructions, methods or ideas contained in the book. Publishing Process Manager Romana Vukelic Technical Editor Teodora Smiljanic Cover Designer InTech Design Team First published April, 2012 Printed in Croatia A free online edition of this book is available at www.intechopen.com Additional hard copies can be obtained from [email protected] Hyperparathyroidism, Edited by Gonzalo Díaz-Soto and Manuel Puig-Domingo p. -

Hormonally Active Adrenocortical Carcinoma in a 24-Year Old Woman
ACS Case Reviews in Surgery Vol. 1, No. 1 Hormonally active adrenocortical carcinoma in a 24-year old woman AUTHORS: CORRESPONDENCE AUTHOR: AUTHOR AFFILIATIONS: Wachtel H1-4, Sadow PM2,4, Stathatos N3,4, Dr. Carrie Lubitz, MD, FACS 1 Massachusetts General Hospital, Dept. of Surgery, Lubitz CC1,4 Massachusetts General Hospital Div. of General & Endocrine Surgery, Boston, MA Yawkey Center for Outpatient Care, 7B 2 Massachusetts General Hospital, Dept. of 55 Fruit Street Pathology, Boston, MA Boston, MA 02114 3 Massachusetts General Hospital, Dept. of Phone: 617-643-9473 Medicine, Div. of Endocrinology, Boston, MA Fax: 617-724-3895 4 Harvard Medical School, Boston, MA Email: [email protected] Background Adrenal tumors are common and frequently identified incidentally; adrenalectomy is indicated for functional tumors, masses ≥4 cm, and cases where malignancy is suspected. Summary A 24-year old previously healthy woman presented with a six-month history of weight gain, amenorrhea, hirsutism, acne, and hypertension. Biochemical evaluation revealed hypercortisolism and elevated DHEA-S. Abdominal imaging demonstrated an 11 cm right adrenal mass, abutting the right hepatic lobe, right kidney, and inferior vena cava. The patient underwent open right adrenalectomy for the presumptive diagnosis of hormonally active adrenocortical carcinoma (ACC). The tumor was able to be mobilized from surrounding structures without requiring resection of adjacent organs. Pathological exam demonstrated a 728 g, 16.5 cm ACC with extensive necrosis, and Ki67 proliferation index of 35% and large vessel vascular invasion. Postoperatively, the symptoms of hypercortisolism, virilization, and hypertension resolved. The patient is currently undergoing adjuvant mitotane therapy and has no evidence of disease six months after surgery. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular