1 Annex 2. AHRQ ICD-9 Procedure Codes 0044 PROC-VESSEL
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Late Complications of Hemispherectomy: Report of a Case Relieved by Surgery
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.33.3.372 on 1 June 1970. Downloaded from J. Neurol. Neurosurg. Psychiat., 1970, 33, 372-375 Late complications of hemispherectomy: report of a case relieved by surgery NINAN T. MATHEW, JACOB ABRAHAM, AND JACOB CHANDY From the Department of Neurological Sciences, Christian Medical College Hospital, Vellore, S. India SUM M A RY A case of Sturge-Weber disease treated with left hemispherectomy presented, 11 years later, with complications related to delayed intracranial haemorrhage. A loculation syndrome of the right lateral ventricle was detected and it was corrected by a ventriculoatrial shunt operation. The side of the hemispherectomy was evacuated of all the chronic products of haemorrhage, including the subdural membrane. The patient was relieved of her symptoms. It is considered that compli- cations related to delayed haemorrhage after hemispherectomy are remediable. Immediate and delayed complications occur after 10 July 1969, with persistent headache, vomiting, and hemispherectomy. Early complications include ob- increasing drowsiness of three weeks' duration. She was structive hydrocephalus and herniations of the born with a Sturge-Weber syndrome and had had a leftProtected by copyright. remaining hemisphere (Cabieses, Jeri, and Landa, hemispherectomy performed in another country 11 years before. She was free from seizures and major behavioural 1957; Laine, Pruvot, and Osson, 1964). A syndrome problems and was attending a school for backward of delayed intracranial haemorrhage was reported by children till November 1968, when she developed severe Oppenheimer and Griffith (1966). The essential constant headache, vomiting, and drowsiness. She was features of the syndrome are (I) an infantile hemi- admitted elsewhere in early December 1968, where plegia treated by hemispherectomy; (2) a trouble- browniish yellow fluid with a protein content of 1,150 mg/ free period lasting for some years; (3) a period of 100 nil. -

Laparoscopic Gastropexy As a Preventative Measure for Gastric Dilation Volvulus in Canines
Laparoscopic Gastropexy as a Preventative Measure for Gastric Dilation Volvulus in Canines By: Erin O’Brien Advisors: Dr. Kimberly Boswell Board Certified Surgeon Southwest Michigan Animal Emergency Hospital Kalamazoo, MI Dr. Diane R. Kiino Ph.D. Kalamazoo College Health Science A paper submitted in partial fulfillment of the requirements for the degree of Bachelor of Arts at Kalamazoo College. 2010 ii ACKNOWLEDGEMENTS Over the summer I was able to intern at the Southwest Michigan Animal Emergency Hospital in Kalamazoo, MI. It was there that I was exposed to the emergency setting in veterinary medicine but also had the chance to observe surgeries done by Board Certified Surgeon, Dr. Kimberly Boswell. I would like to thank the entire staff at SWMAEH for teaching me a tremendous amount about veterinary medicine and allowing me to get as much hands on experience as possible. It was such a privilege to complete my internship at a hospital where I was able to learn so much about veterinary medicine in only ten weeks. I would also like to thank Dr. Boswell in particular, it was a gastropexy surgery I saw her perform during my internship that inspired the topic of this paper. Additionally I would like to acknowledge my advisor Dr. Diane Kiino for providing the direction I needed in choosing my paper topic. iii ABSTRACT Gastric Dilation Volvulus (GDV) is a fatal condition in canines especially those that are large or giant breeds. GDV results from the stomach distending and twisting on itself which when left untreated causes shock and ultimately death. The only method of prevention for GDV is a gastropexy, a surgical procedure that sutures the stomach to the abdominal wall to prevent volvulus or twisting. -

This Article Appeared in a Journal Published by Elsevier. the Attached
This article appeared in a journal published by Elsevier. The attached copy is furnished to the author for internal non-commercial research and education use, including for instruction at the authors institution and sharing with colleagues. Other uses, including reproduction and distribution, or selling or licensing copies, or posting to personal, institutional or third party websites are prohibited. In most cases authors are permitted to post their version of the article (e.g. in Word or Tex form) to their personal website or institutional repository. Authors requiring further information regarding Elsevier’s archiving and manuscript policies are encouraged to visit: http://www.elsevier.com/copyright Author's personal copy Neuropsychologia 48 (2010) 1683–1688 Contents lists available at ScienceDirect Neuropsychologia journal homepage: www.elsevier.com/locate/neuropsychologia Cerebral lateralization of vigilance: A function of task difficulty a, b b c William S. Helton ∗, Joel S. Warm , Lloyd D. Tripp , Gerald Matthews , Raja Parasuraman e, Peter A. Hancock d a Department of Psychology, University of Canterbury, Private Bag 4800, Christchurch, New Zealand b Air Force Research Laboratory, Wright Patterson Air Force Base, Dayton, OH, USA c Department of Psychology, University of Cincinnati, OH, USA d Department of Psychology, University of Central Florida, Orlando, FL, USA e Department of Psychology, George Mason University, VA, USA article info a b s t r a c t Article history: Functional near infrared spectroscopy (fNIRS) measures of cerebral oxygenation levels were collected Received 6 July 2009 from participants performing difficult and easy versions of a 12 min vigilance task and for controls who Received in revised form 10 February 2010 merely watched the displays without a work imperative. -

Multisectoral Academic Training Guide on Female Genital Mutilation/Cutting
Multisectoral Academic Training Guide on Female Genital Mutilation/Cutting Directoras Adriana Kaplan y Laura Nuño Gómez Coordinadoras Magaly Thill y Nora Salas Seoane Multisectoral Academic Training Guide on Female Genital Mutilation/Cutting Multisectoral Academic Training Guide on Female Genital Mutilation/Cutting Directoras Adriana Kaplan y Laura Nuño Gómez Coordinadoras Magaly Thill y Nora Salas Seoane Neus Aliaga Sonia Núñez Puente Rut Bermejo Casado Laura Nuño Gómez Clara Carvalho Els Leye Giovanna Cavatorta Carla Moleiro Gily Coene Maya Pellicciari Ricardo Falcão Francesco Pompeo Lidia Fernández Montes Julia Ropero Carrasco Diana Fernández Romero Nora Salas Seoane Sabrina Flamini Cristina Santinho Michela Fusaschi Magaly Thill Cecilia Gallotti Valentina Vitale Adriana Kaplan Edición y revisión de la versión original en inglés Lucy Deegan Leirião This publication has been produced with the financial support of the Rights, Equality and Citizenship Programme 2014-2020 of the European Union. The contents of this publication are the sole responsibility of its authors and can in no way be taken to reflect the views of the European Commission. It is part of the Multisectoral Academic Programme to prevent and combat Female Genital Mutilation (FGM/C). © Los autores Editorial DYKINSON, S.L. Meléndez Valdés, 61 – 28015 Madrid Teléfono (+34) 91544 28 46 – (+34) 91544 28 69 e-mail: [email protected] http://www.dykinson.es http://www.dykinson.com ISBN: Preimpresión: Besing Servicios Gráfi cos, S.L. [email protected] Table of contents List of abbreviations ..................................................................................... 15 Institutions and authors ............................................................................... 17 Chapter I. Introduction to the Multisectoral Academic Training Guide on FGM/C .............................................................................. 25 Laura Nuño Gómez and Adriana Kaplan 1. -

Breast Reduction with Dermoglandular Flaps Tessier’S “Total Dermo-Mastopexy” and the “Yin-Yang Technique”
BREAST SURGERY Breast Reduction With Dermoglandular Flaps Tessier’s “Total Dermo-Mastopexy” and the “Yin-Yang Technique” Francesco Gargano, MD, PhD,* Paul Tessier, MD,† and S. Anthony Wolfe, MD‡ skin and the gland and less “isolation” of the areola from the skin Abstract: The use of dermoglandular flaps in reduction mastopexy was and its vascular and nerve network. Because of this, there was advocated by Paul Tessier, who never published his method, but had actually greater security for the nipple and the skin flaps; but, the most rapid almost finished the following article before his death in June 2008. Dr. method seemed also to be a reason for its choice. Tessier is acknowledged as the “father” of craniofacial surgery, but he had The Ragnell procedure, and particularly the Biesenberger interest in aesthetic surgery, and was quite proud of the technique he procedure, has been criticized because of a lack of vascular security had developed using dermoglandular flaps in reduction mammoplasty. He associated with an extended dissection between the skin and the had literally hundreds of techniques and methods that he had developed but gland. During 1947 or 1948, I observed Mcindoe brilliantly per- which never found their way into print, both because of his enormous forming a Biesenberger procedure, and noted a good shape of the surgical schedule, and perhaps his self-imposed standards for anything that breast at the end of the operation. Thus, I began using the Biesen- he published, which were almost impossibly high. The technique proposed berger procedure in this pure form, but was never satisfied with my by Dr. -

Female Genital Cosmetic Surgery Exceptional
FEMALE GENITAL COSMETIC SURGERY EXCEPTIONAL FUNDING REQUIRED BaNES, Swindon and Wiltshire CCG (BSW) does not normally fund elective vaginal labial surgery, vaginoplasty or hymenorrhaphy. Clinicians must ensure there is a clear clinical rationale for any potential intervention, as all procedures that involve partial or total removal of the external female genitalia for non-clinical reasons are defined as Female Genital Mutilation and as such are against the law. (The Female Genital Mutilation Act of 2003) Clinicians must be alert to the possibility that some patients who seek revision surgery may do so as a result of previous interventions which are classed as unlawful under the Act. Background Labiaplasty A labiaplasty is a surgical procedure to reduce the size of the labia minora. Labiaplasty is generally a cosmetic procedure to change appearance alone and common consequence of childbirth is not sufficient reason to apply for funding. Labiaplasty is not normally supported or funded by the CCG. Vaginoplasty Non-reconstructive vaginoplasty or "vaginal rejuvenation" is used to restore vaginal tone and appearance. As this is generally considered a cosmetic procedure, vaginoplasty is not normally supported or funded by the CCG. Hymenorrhaphy Hymenorrhaphy, or hymen reconstruction surgery, is a cosmetic procedure and is not normally supported or funded by the CCG. This policy does not relate to reversal of female genital mutilation. This policy is informed by the NHS England (2013) Interim Clinical Commissioning Policy Labiaplasty, Vaginoplasty & Hymenorrhaphy. (Armed Forces Commissioning Policy Task and Finish Group) Reference: Policy Name Review Date Version BSW-CP046 Female Genital Cosmetic Surgery March 2023 4.1 . -

Laparoscopic Fundoplication with Double Sided Posterior Gastropexy: a Different Surgical Technique
View metadata, citation and similar papers at core.ac.uk ORIGINAL RESEARCH brought to you by CORE provided by Elsevier - Publisher Connector International Journal of Surgery 10 (2012) 532e536 Contents lists available at SciVerse ScienceDirect International Journal of Surgery journal homepage: www.theijs.com Original research Laparoscopic fundoplication with double sided posterior gastropexy: A different surgical technique Fahri Yetis¸ira,*, A. Ebru Salman b,Dogukan Durak a, Mehmet Kiliç c a Ataturk Research and Training Hospital, General Surgery Department, Turkey b Ataturk Research and Training Hospital, Anesthesiology and Reanimation Department, Turkey c Yildirim Beyazit University, General Surgery Department, Turkey article info abstract Article history: Background: Laparoscopic Nissen Fundoplication has become the gold standard surgical procedure for Received 18 April 2012 management of gastroesophageal reflux disease. Nissen fundoplication provides an effective barrier Received in revised form against reflux. The aim of this study was to evaluate early postoperative outcomes of a different surgical 3 August 2012 technique, laparoscopic fundoplication with double sided posterior gastropexy. Accepted 6 August 2012 Methods: Data of 46 patients who underwent laparoscopic fundoplication with double sided posterior Available online 21 August 2012 gastropexy between February 2010 and December 2011 were collected. Surgically, after Nissen fundoplication was completed, 2e4 sutures were passed through the uppermost parts of the posterior Keywords: Gastropexy and anterior wall of the gastric wrap and then passed gently 1 cm above the celiac artery from the denser fi Nissen fundoplication bers of uppermost part of the arcuate ligament. Demographic data, preoperative and postoperative Gastroesophageal reflux assesments of sympthomatic and functional outcomes of patients were recorded. -

Improved Preservation of Human Corneal Basement Membrane
BritishJournal ofOphthalmology 1994; 78: 863-870 863 Improved preservation ofhuman corneal basement membrane following freezing of donor tissue for Br J Ophthalmol: first published as 10.1136/bjo.78.11.863 on 1 November 1994. Downloaded from epikeratophakia Robert D Young, W John Armitage, Paul Bowerman, Stuart D Cook, David L Easty Abstract States, good results continue to be achieved by Current methods for the production of the small number ofBritish surgeons performing lenticules for epikeratophakia involve rapid the technique.4 However, no comprehensive freezing, cryolathing, and slow warming of the account of its long term outcome has yet been donor cornea. We have found that this pro- published. cedure causes structural damage to the Several complications resulting in the failure epithelial basement membrane in the donor of epikeratophakia have been reported, includ- cornea which may subsequently contribute to ing infection, graft dehiscence, persistent inter- poor postoperative re-epithelialisation of the face haze or opacity, ulceration, and imperfect implant, leading to graft failure. Endeavouring re-epithelialisation. Among these, the failure of to overcome these problems, the effects of host epithelial cells to migrate over and re- cryoprotection of donor cornea were investi- surface the anterior face of the grafted tissue gated, using dimethyl sulphoxide, in conjunc- continues to be the major reason for the removal tion with different cooling and warming rates ofepikeratophakia lenticules.'-'0 as part of the protocol for cryolathing. The Epithelial healing is itselfa complex phenome- structural integrity of the epithelial basement non involving mitosis of host cells at the graft membrane zone (BMZ) was then assessed by periphery, centripetal migration, and attach- electron microscopy and by immunofluores- ment. -
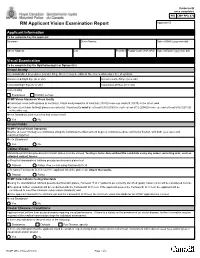
RCMP GRC 2180E (2017-10) Page 1 of 2 Protected B RM Applicant Vision Examination Report Once Completed Applicant ID
Protected B once completed PIB CMP PPU 070 RM Applicant Vision Examination Report Applicant ID Applicant Information To be completed by the applicant Surname Given Names Date of Birth (yyyy-mm-dd) Street Address City Province Postal Code (A9A 9A9) Date of Exam (yyyy-mm-dd) Visual Examination To be completed by the Ophthalmologist or Optometrist Visual Acuity Any standardized procedures (Landoit Ring, Snellen) may be utilized. No error is allowed per line of symbols. Uncorrected Right Eye (6/ or 20/) Uncorrected Left Eye (6/ or 20/) Corrected Right Eye (6/ or 20/) Corrected Left Eye (6/ or 20/) Corrected by Eyeglasses Contact Lenses RCMP Vision Standards Visual Acuity Corrected vision (with glasses or contacts): Visual acuity must be at least 6/6 (20/20) in one eye and 6/9 (20/30) in the other; and Uncorrected vision (without glasses or contacts): Visual acuity must be at least 6/18 (20/60) in each eye or 6/12 (20/40) in one eye and at least 6/30 (20/100) in the other eye. Meets Standards, both corrected and uncorrected? Yes No Visual Fields RCMP Field of Vision Standards Must be at least 150 degrees continuous along the horizontal meridian and 20 degrees continuous above and below fixation, with both eyes open and examined together. Meets Standards? Yes No Colour-Vision Standardized Ishihara pseudo-isochromatic plates must be utilized. Testing is to be done without the candidate using any colour correcting aids, such as coloured contact lenses. a) Result of standardized Ishihara pseudo-isochromatic plates test Passed Failed. If so, re-test using Farnsworth D-15. -

Modern Laser in Situ Keratomileusis Outcomes
REVIEW/UPDATE Modern laser in situ keratomileusis outcomes Helga P. Sandoval, MD, MSCR, Eric D. Donnenfeld, MD, Thomas Kohnen, MD, PhD, FEBO, Richard L. Lindstrom, MD, Richard Potvin, OD, David M. Tremblay, MD, Kerry D. Solomon, MD Laser in situ keratomileusis (LASIK) articles published between 2008 and 2015 that contain clin- ical outcomes data were reviewed and graded for quality, impression, and potential bias. All 97 relevant articles (representing 67 893 eyes) provided a positive or neutral impression of LASIK. Industry bias was not evident. The aggregate loss of 2 or more lines of corrected distance visual acuity was 0.61% (359/58 653). The overall percentage of eyes with uncorrected distance visual acuity better than 20/40 was 99.5% (59 503/59 825). The spherical equivalent refraction was within G1.0 diopter (D) of the target refraction in 98.6% (59 476/60 329) of eyes, with 90.9% (59 954/65 974) within G0.5 D. In studies reporting patient satisfaction, 1.2% (129/9726) of pa- tients were dissatisfied with LASIK. Aggregate outcomes appear better than those reported in summaries of the safety and effectiveness of earlier laser refractive surgery systems approved by the U.S. Food and Drug Administration. Modern results support the safety, efficacy, and patient satisfaction of the procedure. Financial Disclosure: Proprietary or commercial disclosures are listed after the references. J Cataract Refract Surg 2016; 42:1224–1234 Q 2016 ASCRS and ESCRS Laser in situ keratomileusis (LASIK) is one of the most have been performed globally.1 Laser in situ keratomil- commonly performed elective procedures in the United eusis was introduced by Pallikaris et al.2 in 1990. -

Diagnostic Nasal/Sinus Endoscopy, Functional Endoscopic Sinus Surgery (FESS) and Turbinectomy
Medical Coverage Policy Effective Date ............................................. 7/10/2021 Next Review Date ....................................... 3/15/2022 Coverage Policy Number .................................. 0554 Diagnostic Nasal/Sinus Endoscopy, Functional Endoscopic Sinus Surgery (FESS) and Turbinectomy Table of Contents Related Coverage Resources Overview .............................................................. 1 Balloon Sinus Ostial Dilation for Chronic Sinusitis and Coverage Policy ................................................... 2 Eustachian Tube Dilation General Background ............................................ 3 Drug-Eluting Devices for Use Following Endoscopic Medicare Coverage Determinations .................. 10 Sinus Surgery Coding/Billing Information .................................. 10 Rhinoplasty, Vestibular Stenosis Repair and Septoplasty References ........................................................ 28 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence -

Photorefractive Keratectomy for Correction of Epikeratophakia
CASE REPORTS AND SMALL CASE SERIES high myopia resulting from poste- results might be related to the pre- Photorefractive Keratectomy rior lenticonus. Postsurgical refrac- existing corneal stromal abnormali- for Correction of tion was stable for 8 years, then a ties in their patients, which were not Epikeratophakia Regression rapid myopic regression of the epi- observed in our group. Thus, PRK keratophakic lenses was observed can effectively be used to treat epi- Excimer laser photorefractive kera- the following year (Table). In- keratophakic regressed lenses in a se- tectomy (PRK) is widely used for the stead of removing the failed epikera- lected group of patients in whom correction of myopia, astigmatism, tophakic lenses, we performed PRK both the epikeratograft and the sur- and hyperopia.1,2 It has also been on the eyes. rounding cornea are clear. This used for correction of astigmatism method eliminates the need for re- after penetrating keratoplasty.3 Results. Two and a half years after moval of the epikeratograft and ex- Epikeratophakia has been used PRK, the refraction in all 4 eyes is posing the patient to the risks of suc- in the treatment of nontolerant con- stable and the epigrafts are clear. The cessive penetrating keratoplasty. tact lens keratoconous patients.4,5 Table presents the refraction and vi- The epigrafts were made from ma- sual acuity results for the eyes be- Hirsh Ami, MD chined corneal tissue that was found fore PRK and at 3 months, 1 year, Solberg Yoram, MD, PhD unsuitable for penetrating kerato- and 21⁄2 years after PRK. No haze has Cahana Michael, MD plasty.