Poster Presentations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ACTH Stimulation Tests for the Diagnosis of Adrenal Insufficiency: Systematic Review and Meta-Analysis
ORIGINAL ARTICLE ACTH Stimulation Tests for the Diagnosis of Adrenal Insufficiency: Systematic Review and Meta-Analysis Naykky Singh Ospina,* Alaa Al Nofal,* Irina Bancos, Asma Javed, Khalid Benkhadra, Ekta Kapoor, Aida N. Lteif, Neena Natt, and M. Hassan Murad Evidence-Based Practice Research Program (N.S.O., A.A.N., K.B., M.H.M.), Mayo Clinic, Rochester, Downloaded from https://academic.oup.com/jcem/article/101/2/427/2810551 by guest on 29 September 2021 Minnesota; Knowledge and Evaluation Research Unit (N.S.O., K.B., M.H.M.), Mayo Clinic, Rochester, Minnesota; Division of Endocrinology, Diabetes, Metabolism, and Nutrition (N.S.O., N.N., I.B.), Mayo Clinic, Rochester, Minnesota; Division of Pediatric Endocrinology and Metabolism (A.A.N., A.J., A.N.L.), Mayo Clinic, Rochester, Minnesota; Division of General Internal Medicine (E.K.), Mayo Clinic, Rochester, Minnesota 55905 Context: The diagnosis of adrenal insufficiency is clinically challenging and often requires ACTH stimulation tests. Objective: To determine the diagnostic accuracy of the high- (250 mcg) and low- (1 mcg) dose ACTH stimulation tests in the diagnosis of adrenal insufficiency. Methods: We searched six databases through February 2014. Pairs of independent reviewers se- lected studies and appraised the risk of bias. Diagnostic association measures were pooled across studies using a bivariate model. Data Synthesis: For secondary adrenal insufficiency, we included 30 studies enrolling 1209 adults and 228 children. High- and low-dose ACTH stimulation tests had similar diagnostic accuracy in adults and children using different peak serum cortisol cutoffs. In general, both tests had low sensitivity and high specificity resulting in reasonable likelihood ratios for a positive test (adults: high dose, 9.1; low dose, 5.9; children: high dose, 43.5; low dose, 7.7), but a fairly suboptimal likelihood ratio for a negative test (adults: high dose, 0.39; low dose, 0.19; children: high dose, 0.65; low dose, 0.34). -

SNAP Cortisol Testing Guide
SNAP® Cortisol Testing Guide Diagnosing and Treating Cases of Suspected Canine Hyperadrenocorticism or Addison’s Disease IMPORTANT: Review history of any administration of corticosteroids as these may influence the reported results. Diagnose ACTH Stimulation Test Diagnostic Protocol for Cases of Suspected Canine Hyperadrenocorticism or Addison’s Disease History, physical exam, CBC, chemistry panel, electrolytes and urinalysis consistent with Canine Hyperadrenocorticism or Addison’s disease Draw baseline cortisol sample. Perform an ACTH stimulation test with Cortrosyn® 5 µg/kg IV or ACTH gel 2.2 U/kg IM. Draw 1-hour cortisol (Cortrosyn®) or 1 and 2-hour cortisol (ACTH gel). Pre-ACTH: 2–6 µg/dL Pre- and Post-ACTH Post-ACTH Post-ACTH Post-ACTH 2 6 µg/dL >22 µg/dL <2 µg/dL – Post-ACTH: 6–18 µg/dL 18–22 µg/dL If both results are <2 µg/dL, results are Equivocal, Consistent Inconclusive consistent with Normal Cushing’s possible with Cushing’s hypoadrenocorticism Perform high-dose dexamethasone* Begin treatment with suppression to mineralocorticoid discriminate between and/or glucocorticoid PDH and ATH, as appropriate. ACTH level and/or abdominal ultrasound. * Do not exceed 0.1 mg/kg of dexamethasone. Diagnose Low-Dose Dexamethasone Suppression Protocol For Cases of Suspected Canine Hyperadrenocorticism History, physical exam, CBC, chemistry panel, electrolytes and urinalysis consistent with Canine Hyperadrenocorticism Draw baseline cortisol sample. Perform a low-dose dexamethasone suppression test with 0.01 mg/kg of dexamethasone IV. Draw 4-hour -

Adrenal Incidentalomas with Supraphysiologic Response to ACTH Stimulus: a Case Report
Hindawi Publishing Corporation Case Reports in Endocrinology Volume 2012, Article ID 503290, 4 pages doi:10.1155/2012/503290 Case Report Adrenal Incidentalomas with Supraphysiologic Response to ACTH Stimulus: A Case Report Marianna Antonopoulou1 and Asya Perelstein2 1 SUNY Downstate Medical Center, 450 Clarkson Avenue, Box 1205, Brooklyn, NY 11203, USA 2 VA Medical Center, 800 Poly Place, New York, NY 11209, USA Correspondence should be addressed to Marianna Antonopoulou, [email protected] Received 7 August 2012; Accepted 20 September 2012 Academic Editors: I. Broom, C. Capella, and T. Konrad Copyright © 2012 M. Antonopoulou and A. Perelstein. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. We present the diagnostic approach of a patient with adrenal incidentalomas. A 72-year-old African American male had a CT scan of the abdomen showing right and left adrenal masses measuring 5 × 3.5 cm and 3.7 × 2.9 cm, respectively. The patient had negative hormonal workup. The radiologist insisted that the CT findings are consistent with adrenal hyperplasia, and therefore he underwent ACTH stimulation to rule out late-onset congenital adrenal hyperplasia (CAH). The stimulation test revealed that 17-hydroxyprogesterone and 11-deoxycortisol increased to levels high enough to confirm CAH, but cortisol had exaggerated response as well, thus making the diagnosis of CAH unlikely where metabolism is shifted to precursors. Subsequently, the patient underwent screening for Cushing’s syndrome (CS) with a dexamethasone suppression test. Patient failed the suppresion test, raising the issue for subclinical CS (SCS), likely due to ACTH-independent macronodular adrenal hyperplasia. -

A Guide to Obesity and the Metabolic Syndrome
A GUIDE TO OBESITY AND THE METABOLIC SYNDROME ORIGINS AND TREAT MENT GEORG E A. BRA Y Louisiana State University, Baton Rouge, USA Boca Raton London New York CRC Press is an imprint of the Taylor & Francis Group, an informa business © 2011 by Taylor and Francis Group, LLC CRC Press Taylor & Francis Group 6000 Broken Sound Parkway NW, Suite 300 Boca Raton, FL 33487-2742 © 2011 by Taylor and Francis Group, LLC CRC Press is an imprint of Taylor & Francis Group, an Informa business No claim to original U.S. Government works Printed in the United States of America on acid-free paper 10 9 8 7 6 5 4 3 2 1 International Standard Book Number: 978-1-4398-1457-4 (Hardback) This book contains information obtained from authentic and highly regarded sources. Reasonable efforts have been made to publish reliable data and information, but the author and publisher cannot assume responsibility for the valid- ity of all materials or the consequences of their use. The authors and publishers have attempted to trace the copyright holders of all material reproduced in this publication and apologize to copyright holders if permission to publish in this form has not been obtained. If any copyright material has not been acknowledged please write and let us know so we may rectify in any future reprint. Except as permitted under U.S. Copyright Law, no part of this book may be reprinted, reproduced, transmitted, or uti- lized in any form by any electronic, mechanical, or other means, now known or hereafter invented, including photocopy- ing, microfilming, and recording, or in any information storage or retrieval system, without written permission from the publishers. -
The Encyclopedia of Endocrine Diseases and Disorders
THE ENCYCLOPEDIA OF lJ z > 0 z Endocrine < I ~ Diseases UJ< I and Disorders UJ ...J '-'- z 0 V'l 1- u '-'-< WILLIAM P ETIT. JR.. M.0. CHRISTINE ADAMEC THE ENCYCLOPEDIA OF ENDOCRINE DISEASES AND DISORDERS THE ENCYCLOPEDIA OF ENDOCRINE DISEASES AND DISORDERS William Petit Jr., M.D. Christine Adamec The Encyclopedia of Endocrine Diseases and Disorders Copyright © 2005 by William Petit Jr., M.D., and Christine Adamec All rights reserved. No part of this book may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage or retrieval systems, without permission in writing from the publisher. For information contact: Facts On File, Inc. 132 West 31st Street New York NY 10001 Library of Congress Cataloging-in-Publication Data Petit, William. The encyclopedia of endocrine diseases and disorders / William Petit Jr., Christine Adamec. p. ; cm. Includes bibliographical references and index. ISBN 0-8160-5135-6 (hc : alk. paper) 1. Endocrine glands—Diseases—Encyclopedias. [DNLM: 1. Endocrine Diseases—Encyclopedias—English. WK 13 P489ea 2005] I. Adamec, Christine A., 1949– II. Title. RC649.P48 2005 616.4’003—dc22 2004004916 Facts On File books are available at special discounts when purchased in bulk quantities for businesses, associations, institutions, or sales promotions. Please call our Special Sales Department in New York at (212) 967-8800 or (800) 322-8755. You can find Facts On File on the World Wide Web at http://www.factsonfile.com. Text and cover design by Cathy Rincon Printed in the United States of America VB FOF 10 9 8 7 6 5 4 3 2 1 This book is printed on acid-free paper. -

Obituary Prof. Dr. Ruth Illig
International Journal of Neonatal Screening Obituary Obituary Prof. Dr. Ruth Illig Annette Grüters-Kieslich 1,*, Toni Torresani 2 and Daniel Konrad 3 1 Chief Medical Director and Chairwoman of the Board, Heidelberg University Hospital, Im Neuenheimer Feld 672, 69120 Heidelberg, Germany 2 Former Director Swiss Newborn Screening Laboratory, University Children‘s Hospital, Steinwiesstrasse 75, 8032 Zürich, Switzerland; [email protected] 3 Head of the Department of Paediatric Endocrinology and Diabetology, University Children‘s Hospital, Steinwiesstrasse 75, 8032 Zürich, Switzerland; [email protected] * Correspondence: [email protected] Received: 27 July 2017; Accepted: 28 July 2017; Published: 3 August 2017 On 26 June 2017 Prof. Dr. Ruth Illig peacefully passed away after a life fulfilled with an untiring commitment for children with endocrine diseases. She has been an enthusiastic fighter for the improvement of child health not only in Europe, but also with a global perspective. Ruth Illig was born on 12 November 1924 in Nuremberg, Germany. Her childhood and adolescence in Germany was affected by the Second World War. During the war, she was brought from Germany to Switzerland to recover from the stressful situation and physical weakening. After the war, she spent a significant time of her academic training in Bern and Zurich. Following graduation from medical school she was accepted by Prof. Guido Fanconi for a pediatric residency at the University Children’s Hospital (Kinderspital) Zurich, Switzerland. She was promoted to a fellow and tenure position and worked closely with Prof. Andrea Prader. In these early years, she focused on growth disorders and she established the endocrine laboratory using radioimmunoassays for determination of growth hormone and insulin. -

Endocrine Test Selection and Interpretation
The Quest Diagnostics Manual Endocrinology Test Selection and Interpretation Fourth Edition The Quest Diagnostics Manual Endocrinology Test Selection and Interpretation Fourth Edition Edited by: Delbert A. Fisher, MD Senior Science Officer Quest Diagnostics Nichols Institute Professor Emeritus, Pediatrics and Medicine UCLA School of Medicine Consulting Editors: Wael Salameh, MD, FACP Medical Director, Endocrinology/Metabolism Quest Diagnostics Nichols Institute San Juan Capistrano, CA Associate Clinical Professor of Medicine, David Geffen School of Medicine at UCLA Richard W. Furlanetto, MD, PhD Medical Director, Endocrinology/Metabolism Quest Diagnostics Nichols Institute Chantilly, VA ©2007 Quest Diagnostics Incorporated. All rights reserved. Fourth Edition Printed in the United States of America Quest, Quest Diagnostics, the associated logo, Nichols Institute, and all associated Quest Diagnostics marks are the trademarks of Quest Diagnostics. All third party marks − ®' and ™' − are the property of their respective owners. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording, and information storage and retrieval system, without permission in writing from the publisher. Address inquiries to the Medical Information Department, Quest Diagnostics Nichols Institute, 33608 Ortega Highway, San Juan Capistrano, CA 92690-6130. Previous editions copyrighted in 1996, 1998, and 2004. Re-order # IG1984 Forward Quest Diagnostics Nichols Institute has been -

Pediatric Endocrinology
Books & journals books Adrenal: Fluck, C. E. (ed.) & Miler, W. L. (ed.) . Disorders of the human adrenal cortex. Basel: Karger; 2018. Krieger, D. T. Cushing's syndrome. Berlin: Springer; 1982. Lajic, Svetlana . Molecular analysis of mutated P450c21 in congenital adrenal hyperplasia. Stockholm: Department of Women and Child Health Pediatr; 1998. Lehnert, Hendrik (ed.) . Pheochromocytoma; pathophysiology and clinical management. Basel: Karger; 2004. New, Maria . Advances in steroid disorders in children. Parma: Universita' Degli Studi di Parma; 2000. New, Maria I. (ed.) & Levine, Lenore S. (ed.) . Adrenal diseases in childhood. Basel: Karger; 1984. Vinson, G. P. (ed.) & Anderson, D. C. (ed.) . Adrenal glands, vascular system and hypertension. Bristol: Journal of Endocrinology; 1996. Aging: Brunner,D Jokl, E Eds. Physical activity and aging Basel: Karger,S; 1970. Corpas, Emiliano (ed.) . Endocrinology of Aging ; clinical aspects in diagrams and images. Amsterdam: Elsevier; 2021. Morrison, Mary F. (ed.) . Hormones, gender and the aging brain ; the endocrine basis of geriatric psychiatry. Cambridge: Cambridge University Press; 2000. Olshansky, S. Jay & Carnes, Bruce A. The Quest for immortality ; science at the frontiers of aging. New York: W. W. Norton & Company; 2001. Sinnott, Jan D. Sex roles and Aging : theory and research from a systems perspective. Basel: Karger; 1986. Werner Kohler, Jena (ed.) . Altern und lebenszeit ; vortrage anlablich der jahresversammlung vom 26. bis 29. ; marz 1999 zu halle (saale). Halle: Deutsche Akademie der Naurforscher Leopoldin; 1999. Auto-Immunity: Altman, Amnon (ed.) . Signal transducation pathways in autoimmunity. Basel: Karger; 2002. Bastenie, P. A. (ed.) & Gept, W. (ed.) & Addison, G. M. (ed.) . Immunity and autoimmunity in diabetes mellitus ; proceedings of the francqui foundation colloquium, ; brussels, april 30- may 1, 1973. -

Diagnosis and Management of the Patient with Non-Classic CAH Due to 21-Hydroxylase Deficiency
3 180 A Nordenström and Diagnosis and management of 180:3 R127–R145 Review H Falhammar NCAH MANAGEMENT OF ENDOCRINE DISEASE Diagnosis and management of the patient with non-classic CAH due to 21-hydroxylase deficiency Anna Nordenström1,2 and Henrik Falhammar3,4 1Department of Women’s and Children’s Health, Karolinska Institutet, 2Department of Paediatric Endocrinology, Correspondence Astrid Lindgren Children Hospital, Karolinska University Hospital, 3Department of Endocrinology, Metabolism and should be addressed Diabetes, Karolinska University Hospital, and 4Department of Molecular Medicine and Surgery, Karolinska Institutet, to A Nordenström Stockholm, Sweden Email [email protected] Abstract Non-classic congenital adrenal hyperplasia (NCAH) is a relatively common disorder regardless of ethnicity, but most cases are never diagnosed, especially in males. A baseline 17-hydroxyprogesterone measurement may be used for screening, but 17-hydroxyprogesterone measurement after ACTH stimulation is the gold standard. We advocate a CYP21A2 mutation analysis to verify the diagnosis, for genetic counselling and for better prognostic and treatment guidance. Most patients are diagnosed in adolescence and adult life with hirsutism, acne, a PCOS-like picture and fertility issues. Many men with NCAH never seek medical attention and escape diagnosis. Although treatment is somewhat controversial, an early diagnosis and start of treatment may have positive implications on growth and be relevant for preventing and ameliorating the symptoms and consequences of androgen excess that develop over time, including fertility issues. Long-term treatment with glucocorticoids will improve the androgen symptoms but may result in long-term complications, such as obesity, insulin resistance, hypertension, osteoporosis and fractures. European Journal of Endocrinology The glucocorticoid doses should be kept low. -

Scientific Proceedings 2018 CVMA Convention
Scientific Proceedings 2018 CVMA Convention Table of Contents THURSDAY, JULY 5, 2018. .................................................................................................................................................... 5 Business Management Track .............................................................................................................................................. 5 How to Train Your Millennial ................................................................................................................................................... 5 Show Me the Money! ................................................................................................................................................................ 7 Don’t Fear the Feedback .......................................................................................................................................................... 11 It’s All in the Family: Creating a Team Culture ...................................................................................................................... 15 Becoming a Loving Leader ..................................................................................................................................................... 17 FRIDAY, JULY 6, 2018. ......................................................................................................................................................... 22 Companion Animal: Dentistry ........................................................................................................................................ -

AN UPDATE on ATYPICAL HYPERADRENOCORTICISM Doug Mason, DVM, Dvsc, DACVIM (Small Animal Internal Medicine)
South Clinic: 920 Yonge St, Toronto ON – (416) 920-2002 North Clinic: 280 Sheppard Ave. E., Toronto ON - (416) 226-3663 AN UPDATE ON ATYPICAL HYPERADRENOCORTICISM Doug Mason, DVM, DVSc, DACVIM (Small Animal Internal Medicine) Atypical hyperadrenocorticism is defined as a syndrome in which a dog appears to have hyperadrenocorticism based on history, physical examination and clinicopathologic findings but a low dose dexamethasone suppression test, urine cortisol creatinine ratio test and ACTH stimulation tests fall into the currently accepted reference range. This is an uncommon endocrine disorder, which affects middle aged to older dogs and clinically may mimic the signs of hyperadrenocorticism. This disease is thought to be a result of overproduction of estradiol, androstenedione, progesterone, and 17‐hydroxyprogesterone in addition to cortisol. The disease process may be a result of adrenal hyperplasia, adrenal tumours or a functional pituitary microadenoma. It is more common to have the adrenal form of the disease; however both forms have been documented. Clinical signs may be include polyuria, polydipsia, polyphagia, lethargy, abdominal distension, muscle weakness, or recurrent urinary tract infections. Dogs may also present with dermatological signs as their primary complaint. These dermatological abnormalities may include truncal alopecia, thin skin, comedones, bruising, cutaneous hyperpigmentation, calcinosis cutis, pyoderma, dermal atrophy, secondary demodicosis and seborrhea. Abnormalities to a dogs reproductive status may also be noted and include perianal adenoma in females or castrated males, clitoral hypertrophy in female dogs, behavioural estrus in spayed females, testicular atrophy in intact males, prostomegaly in castrated males or behavioural or physical signs of testosterone excess. Common laboratory abnormalities include an elevated alkaline phosphatise, an elevated ALT, hypercholesterolemia, hyperglycemia, and a decreased BUN. -
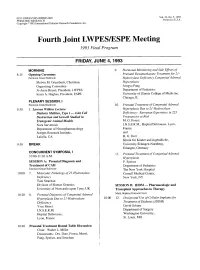
Fourth Joint LWPESJESPE Meeting 1993 Final Program
003 1-399819313305-0000$03.00/0 Vol. 33, No. 5, 1993 PEDIATRIC RESEARCH Printed in U.S.A. Copyright O 1993 International Pediatric Research Foundation, Inc. Fourth Joint LWPESJESPE Meeting 1993 Final Program FRIDAY, JUNE 4,1993 MORNING 9. Hormonal Monitoring and Side Effects of 8: 15 Opening ceremony Prenatal Dexamethasone Treatment for 21 - Fairmont Grand Ballroom Hydroxylase Deficiency Congenital Adrenal Melvin M. Grumbach, Chairman, Hyperplasia Organizing Committee SongyaPang Jo Anne Brasel, President, LWPES Department of Pediatrics Ieuan A. Hughes, President, ESPE University of Illinois College of Medicine, Chicago, IL PLENARY SESSION, I Fairmont Grand Ballroom 10. Prenatal Treatment of Congenital Adrenal 8:30 1. Lawson Wilkins Lecture: Hyperplasia Due to 21 -Hydroxylase Diabetes Mellitus, Type I - Islet Cell Deficiency: European Experience in 223 Destruction and Growth Studied in Pregnancies at Risk Transgenic Animal Models M. G. Forest Nora Sarvetnick I.N.S.E.R.M., Hopital Debrousse, Lyon, Department of Neuropharmacology France Scripps Research Institute, and LaJolla, CA H. G. Dorr Klinik fur Kinder and Jugendliche, 9:30 BREAK University Erlangen-Nurnberg, Erlangen, Germany CONCURRENT SYMPOSIA, I 11. Prenatal Treatment of Congenital Adrenal 10:OO-11:30 A.M. Hyperplasia SESSION A: Prenatal Diagnosis and P. Speiser Treatment of CAH Department of Pediatrics Fairmont Grand Ballroom The New York Hospital 10:OO 7. Molecular Pathology of 21 -Hydroxylase Cornell Medical Center, Deficiency New York, NY Tom Strachan Division of Human Genetics SESSION B: IDDM - Pharmacologic and University of Newcastle upon Tyne, UK Transplant Approaches to Therapy 10:20 8. Prenatal Diagnosis of Congenital Adrenal Mark Hopkins Peacock Court Hyperplasia Due to 21 -Hydroxylase 10:OO 12.