Techniques for the Detection of Sickle Cell Disease: a Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Hemoglobin C Trait (AC) Hemoglobin Eletrophoresis and a Mean Corpuscular Volume
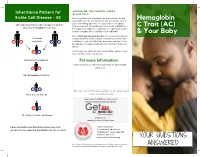
Inheritance Pattern for SHOULD WE, THE PARENTS, TAKE A BLOOD TEST? Sickle Cell Disease - SC Before you have your next baby, we suggest that you and Hemoglobin your partner get special blood test. We all have two sets of genes for hemoglobin. One set is passed on to the baby When one parent has sickle cell trait (AS) and the from each parent. The testing should include, at minimum, a C Trait (AC) other has hemoglobin C trait (AC) hemoglobin eletrophoresis and a mean corpuscular volume. A sickle solubility test (sickledex) is not sufficient! & Your Baby Only if both you and your partner are tested can you know their baby exactly what kind of hemoglobin condition your next child A S may have A C could have. Look carefully at the inheritance pattern for the possibilities of having a baby with the SC form of sickle cell disease. A A A counselor can tell you if any of your future children could have a form of sickle cell disease. AA (normal hemoglobin) For more information or Contact your local SCDAA organization or other health A C agency at: AC (hemoglobin C trait) or A S Or contact the SCDAA National Office at the address and AS (sickle cell trait) or telephone number below. Stay connected with Get Connected the first patient powered registry S C SC (a type of sickle cell disease) Register at www.getconnectedscd.com It does not matter what their other babies have, their Sickle Cell Disease next one has the same four possibilities: AA, AC, AS, or SC. -

Adult, Embryonic and Fetal Hemoglobin Are Expressed in Human Glioblastoma Cells
514 INTERNATIONAL JOURNAL OF ONCOLOGY 44: 514-520, 2014 Adult, embryonic and fetal hemoglobin are expressed in human glioblastoma cells MARWAN EMARA1,2, A. ROBERT TURNER1 and JOAN ALLALUNIS-TURNER1 1Department of Oncology, University of Alberta and Alberta Health Services, Cross Cancer Institute, Edmonton, AB T6G 1Z2, Canada; 2Center for Aging and Associated Diseases, Zewail City of Science and Technology, Cairo, Egypt Received September 7, 2013; Accepted October 7, 2013 DOI: 10.3892/ijo.2013.2186 Abstract. Hemoglobin is a hemoprotein, produced mainly in Introduction erythrocytes circulating in the blood. However, non-erythroid hemoglobins have been previously reported in other cell Globins are hemo-containing proteins, have the ability to types including human and rodent neurons of embryonic bind gaseous ligands [oxygen (O2), nitric oxide (NO) and and adult brain, but not astrocytes and oligodendrocytes. carbon monoxide (CO)] reversibly. They have been described Human glioblastoma multiforme (GBM) is the most aggres- in prokaryotes, fungi, plants and animals with an enormous sive tumor among gliomas. However, despite extensive basic diversity of structure and function (1). To date, hemoglobin, and clinical research studies on GBM cells, little is known myoglobin, neuroglobin (Ngb) and cytoglobin (Cygb) repre- about glial defence mechanisms that allow these cells to sent the vertebrate globin family with distinct function and survive and resist various types of treatment. We have tissue distributions (2). During ontogeny, developing erythro- shown previously that the newest members of vertebrate blasts sequentially express embryonic {[Gower 1 (ζ2ε2), globin family, neuroglobin (Ngb) and cytoglobin (Cygb), are Gower 2 (α2ε2), and Portland 1 (ζ2γ2)] to fetal [Hb F(α2γ2)] expressed in human GBM cells. -

Hemoglobin C Trait What Does This Mean for My Baby, Me and My Family?
My Baby Has Hemoglobin C Trait What does this mean for my baby, me and my family? Your baby's newborn screening test showed tell them their chance to have a baby with a that he or she has hemoglobin C trait (this is hemoglobin disease. also referred to as being a “hemoglobin C carrier”). Babies who have hemoglobin C trait What does having a baby with hemoglobin are no more likely to get sick than any other C trait mean for me, my partner and for baby. They do not need any special medical future pregnancies? treatment. Hemoglobin C trait will not change Since your baby has hemoglobin C trait, this into a disease later on. means that either you or your partner or both of you have hemoglobin C trait. In almost all What causes hemoglobin C trait? cases, ONLY ONE OF YOU will have Hemoglobin C trait happens when the part of hemoglobin C trait. the red blood cell that carries oxygen throughout the body is changed. This part that Most people do not know that they have is changed is called hemoglobin. Hemoglobin hemoglobin C trait. Now that your baby is is important because it picks up oxygen in the known to have hemoglobin C trait, both you lungs and carries it to the other parts of the and your partner have the option of being body. tested. Testing involves a blood test. People usually have one type of hemoglobin. IF ONLY ONE OF YOU HAS HEMOGLOBIN This is called hemoglobin A. Babies with C TRAIT, in every pregnancy there is a: hemoglobin C trait have a second type of • 1 in 2 (50%) chance to have a baby with hemoglobin called hemoglobin C, as well as only the usual hemoglobin A. -

Pathological Conditions Involving Extracellular Hemoglobin
Pathological Conditions Involving Extracellular Hemoglobin: Molecular Mechanisms, Clinical Significance, and Novel Therapeutic Opportunities for alpha(1)-Microglobulin Gram, Magnus; Allhorn, Maria; Bülow, Leif; Hansson, Stefan; Ley, David; Olsson, Martin L; Schmidtchen, Artur; Åkerström, Bo Published in: Antioxidants & Redox Signaling DOI: 10.1089/ars.2011.4282 2012 Link to publication Citation for published version (APA): Gram, M., Allhorn, M., Bülow, L., Hansson, S., Ley, D., Olsson, M. L., Schmidtchen, A., & Åkerström, B. (2012). Pathological Conditions Involving Extracellular Hemoglobin: Molecular Mechanisms, Clinical Significance, and Novel Therapeutic Opportunities for alpha(1)-Microglobulin. Antioxidants & Redox Signaling, 17(5), 813-846. https://doi.org/10.1089/ars.2011.4282 Total number of authors: 8 General rights Unless other specific re-use rights are stated the following general rights apply: Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal Read more about Creative commons licenses: https://creativecommons.org/licenses/ Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. -

Pathogenesis of Hemolytic Anemia in Homozygous Hemoglobin C Disease
Pathogenesis of Hemolytic Anemia in Homozygous Hemoglobin C Disease Samuel Charache, … , Richard J. Ugoretz, J. Richard Spurrell J Clin Invest. 1967;46(11):1795-1811. https://doi.org/10.1172/JCI105670. Research Article Hemoglobin C is less soluble than hemoglobin A in red cells, in hemolysates, and in dilute phosphate buffer. Its relative insolubility may be explained by electrostatic interactions between positively charged β6-lysyl groups and negatively charged groups on adjacent molecules. Red cells from patients with homozygous hemoglobin C (CC) disease exhibit aberrant physical properties which suggest that the cells are more rigid than normal erythrocytes. They pass through membrane filters less readily than normal red cells do, and their viscosity is higher than that of normal cells. Differences from normal cells are exaggerated if mean corpuscular hemoglobin concentration (MCHC) is increased, by suspension in hypertonic salt solution. Increased rigidity of CC cells, by accelerating their fragmentation, may be responsible for formation of microspherocytes. These small dense cells are exceptionally rigid, and probably are even more susceptible to fragmentation and sequestration. Rigidity of CC cells can be attributed to a “precrystalline” state of intracellular hemoglobin, in which crystallization does not occur, although the MCHC exceeds the solubility of hemoglobin in hemolysates. Find the latest version: https://jci.me/105670/pdf The Journal of Clinical Investigation Vol. 46, No. 11, 1967 Pathogenesis of Hemolytic Anemia in Homozygous Hemoglobin C Disease * SAMUEL CHARACHE, C. LOCKARD CONLEY, DAVID F. WAUGH, RICHARD J. UGORETZ,4 AND J. RICHARD SPURRELL WITH THE TECHNICAL ASSISTANCE OF ESTHER GAYLE (From the Department of Medicine, The Johns Hopkins University and Hospital, Baltimore, Maryland, and the Department of Biology, Massachusetts Institute of Technology, Boston, Massachusetts) Abstract. -

Observations on the Minor Basic Hemoglobin Component in the Blood of Normal Individuals and Patients with Thalassemia
Observations on the Minor Basic Hemoglobin Component in the Blood of Normal Individuals and Patients with Thalassemia H. G. Kunkel, … , U. Müller-Eberhard, J. Wolf J Clin Invest. 1957;36(11):1615-1625. https://doi.org/10.1172/JCI103561. Research Article Find the latest version: https://jci.me/103561/pdf OBSERVATIONS ON THE MINOR BASIC HEMOGLOBIN COMPONENT IN THE BLOOD OF NORMAL INDIVIDUALS AND PATIENTS WITH THALASSEMIA BY H. G. KUNKEL, R. CEPPELLINI, U. MULLER-EBERHARD, AND J. WOLF (From the Rockefeller Institute for Medical Research, and Institute for the Study of Human Variation, and the Departmet of Pediatrics, Colunma Uniewsity, N. Y.) (Submitted for publication March 6, 1957; accepted April 11, 1957) In a previous report (1) a second hemoglobin was collected from a number of New York hospitals. was described which was found at a concentration The specimens from patients with thalassemia were ob- of tained from Italian and Greek individuals in the hema- approximately 3 per cent in the blood of normal tology clinic at the Babies Hospital, Columbia-Presby- adult individuals. It was found to resemble he- terian Medical Center, New York. Five individuals with moglobin E in electrophoretic properties, but iden- thalassemia in two families were obtained from index tity with this abnormal hemoglobin was not estab- cases at Bellevue Hospital. The great majority of lished. This same component probably had been thalassemia trait cases were parents of children with observed severe Cooley's anemia. In all instances the diagnosis of by previous investigators employing the thalassemia was based on the hematological picture. classical Tiselius procedure in occasional speci- Several individuals who were suspected of having thalas- mens of blood from normal persons (2, 3) and semia were excluded from the study because of un- thalassemia patients (4), but had not been defined certain hematological findings. -

Chapter 03- Diseases of the Blood and Certain Disorders Involving The
Chapter 3 Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism (D50- D89) Excludes2: autoimmune disease (systemic) NOS (M35.9) certain conditions originating in the perinatal period (P00-P96) complications of pregnancy, childbirth and the puerperium (O00-O9A) congenital malformations, deformations and chromosomal abnormalities (Q00-Q99) endocrine, nutritional and metabolic diseases (E00-E88) human immunodeficiency virus [HIV] disease (B20) injury, poisoning and certain other consequences of external causes (S00-T88) neoplasms (C00-D49) symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (R00-R94) This chapter contains the following blocks: D50-D53 Nutritional anemias D55-D59 Hemolytic anemias D60-D64 Aplastic and other anemias and other bone marrow failure syndromes D65-D69 Coagulation defects, purpura and other hemorrhagic conditions D70-D77 Other disorders of blood and blood-forming organs D78 Intraoperative and postprocedural complications of the spleen D80-D89 Certain disorders involving the immune mechanism Nutritional anemias (D50-D53) D50 Iron deficiency anemia Includes: asiderotic anemia hypochromic anemia D50.0 Iron deficiency anemia secondary to blood loss (chronic) Posthemorrhagic anemia (chronic) Excludes1: acute posthemorrhagic anemia (D62) congenital anemia from fetal blood loss (P61.3) D50.1 Sideropenic dysphagia Kelly-Paterson syndrome Plummer-Vinson syndrome D50.8 Other iron deficiency anemias Iron deficiency anemia due to inadequate dietary -

Sickle Cell Disease
Sickle cell disease Description Sickle cell disease is a group of disorders that affects hemoglobin, the molecule in red blood cells that delivers oxygen to cells throughout the body. People with this disease have atypical hemoglobin molecules called hemoglobin S, which can distort red blood cells into a sickle, or crescent, shape. Signs and symptoms of sickle cell disease usually begin in early childhood. Characteristic features of this disorder include a low number of red blood cells (anemia), repeated infections, and periodic episodes of pain. The severity of symptoms varies from person to person. Some people have mild symptoms, while others are frequently hospitalized for more serious complications. The signs and symptoms of sickle cell disease are caused by the sickling of red blood cells. When red blood cells sickle, they break down prematurely, which can lead to anemia. Anemia can cause shortness of breath, fatigue, and delayed growth and development in children. The rapid breakdown of red blood cells may also cause yellowing of the eyes and skin, which are signs of jaundice. Painful episodes can occur when sickled red blood cells, which are stiff and inflexible, get stuck in small blood vessels. These episodes deprive tissues and organs, such as the lungs, kidneys, spleen, and brain, of oxygen-rich blood and can lead to organ damage. A particularly serious complication of sickle cell disease is high blood pressure in the blood vessels that supply the lungs (pulmonary hypertension), which can lead to heart failure. Pulmonary hypertension occurs in about 10 percent of adults with sickle cell disease. Frequency Sickle cell disease affects millions of people worldwide. -

The Formation of Methemoglobin and Sulfhemoglobin During Sulfanilamide Therapy
THE FORMATION OF METHEMOGLOBIN AND SULFHEMOGLOBIN DURING SULFANILAMIDE THERAPY J. S. Harris, H. O. Michel J Clin Invest. 1939;18(5):507-519. https://doi.org/10.1172/JCI101064. Research Article Find the latest version: https://jci.me/101064/pdf THE FORMATION OF METHEMOGLOBIN AND SULFHEMOGLOBIN DURING SULFANILAMIDE THERAPY By J. S. HARRIS AND H. 0. MICHEL (From the Departments of Pediatrics and Biochemistry, Duke University School of Medicine, Durham) (Received for publication April 8, 1939) Cyanosis almost invariably follows the admin- during the administration of sulfanilamide. Wen- istration of therapeutic amounts of sulfanilamide del (10) found spectroscopic evidence of met- (1). This cyanosis is associated with and is due hemoglobin in every blood sample containing over to a change in the color of the blood. The dark- 4 mgm. per cent sulfanilamide. Evelyn and Mal- ening of the blood is present only in the red cells loy (11) have found that all patients receiving and therefore must be ascribed to one of two sulfanilamide show methemoglobinemia, although causes, a change in the hemoglobin itself or a the intensity is usually very slight. Finally Hart- staining of the red cells with some product formed mann, Perley, and Barnett (12) found cyanosis during the metabolism of sulfanilamide. It is the associated with methemoglobinemia in almost ev- purpose of this paper to assay quantitatively the ery patient receiving over 0.1 gram sulfanilamide effect of sulfanilamide upon the first of these fac- per kilogram of body weight per day. They be- tors-that is, upon the formation of abnormal lieved that the intensity of the methemoglobinemia heme pigments. -

Hemoglobin C
Hemoglobin C Hemoglobin C trait is an inherited blood trait. It is most make plenty of hemoglobin A, but you also make often found in people whose ancestors came from a less common type of hemoglobin, called Africa, Italy, Greece, Latin America, and the Caribbean hemoglobin C. This is not a disease and does region, but it can also be found in people with ancestry not affect your health. This trait can cause the from other parts of the world. To understand this red blood cells to be slightly smaller than usual. condition, it helps to know more about how your blood Sometimes, this is mistaken for low iron levels is made. (iron-deficiency anemia). However, taking an iron supplement does not change the size of the Hemoglobin red blood cells. Your blood contains millions of red blood cells. Each of your red blood cells has hemoglobin, which gives Hemoglobin C trait does not change into a blood blood its red color and carries oxygen throughout your disease. The importance of identifying body. Hemoglobin is made by combining a “heme” hemoglobin C trait is that it helps find couples portion (iron) and a “globin” portion (protein). The iron whose children may be born with a related blood comes from the food you eat and your body makes the disease. Your chance for having a child with a globins. blood disease depends on whether or not your partner has a blood trait, and, if so, which trait There are different kinds of hemoglobin that the body they have. can make. The most common kind in an adult is hemoglobin A. -

(Hba1c) in the Diagnosis of Diabetes Mellitus
WHO/NMH/CHP/CPM/11.1 Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes Mellitus Abbreviated Report of a WHO Consultation © World Health Organization 2011 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected] ). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected] ). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. -

Heme Degradation in Pathophysiology of and Countermeasures to Inflammation-Associated Disease
International Journal of Molecular Sciences Review Heme Degradation in Pathophysiology of and Countermeasures to Inflammation-Associated Disease Donald David Haines 1,2 and Arpad Tosaki 2,* 1 Advanced Biotherapeutics, London W2 1EB, UK; [email protected] 2 Department of Pharmacology, Faculty of Pharmacy, University of Debrecen, 4032 Debrecen, Hungary * Correspondence: [email protected]; Tel./Fax: +36-52-255586 Received: 27 October 2020; Accepted: 16 December 2020; Published: 18 December 2020 Abstract: The class of tetrapyrrol “coordination complexes” called hemes are prosthetic group components of metalloproteins including hemoglobin, which provide functionality to these physiologically essential macromolecules by reversibly binding diatomic gasses, notably O2, which complexes to ferrous (reduced/Fe(II)) iron within the heme porphyrin ring of hemoglobin in a pH- and PCO2-dependent manner—thus allowing their transport and delivery to anatomic sites of their function. Here, pathologies associated with aberrant heme degradation are explored in the context of their underlying mechanisms and emerging medical countermeasures developed using heme oxygenase (HO), its major degradative enzyme and bioactive metabolites produced by HO activity. Tissue deposits of heme accumulate as a result of the removal of senescent or damaged erythrocytes from circulation by splenic macrophages, which destroy the cells and internal proteins, including hemoglobin, leaving free heme to accumulate, posing a significant toxicogenic challenge. In humans, HO uses NADPH as a reducing agent, along with molecular oxygen, to degrade heme into carbon monoxide (CO), free ferrous iron (FeII), which is sequestered by ferritin protein, and biliverdin, subsequently metabolized to bilirubin, a potent inhibitor of oxidative stress-mediated tissue damage. CO acts as a cellular messenger and augments vasodilation.