Hemoglobin C
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Hemoglobin C Trait (AC) Hemoglobin Eletrophoresis and a Mean Corpuscular Volume
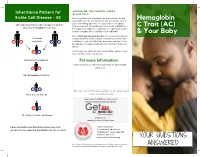
Inheritance Pattern for SHOULD WE, THE PARENTS, TAKE A BLOOD TEST? Sickle Cell Disease - SC Before you have your next baby, we suggest that you and Hemoglobin your partner get special blood test. We all have two sets of genes for hemoglobin. One set is passed on to the baby When one parent has sickle cell trait (AS) and the from each parent. The testing should include, at minimum, a C Trait (AC) other has hemoglobin C trait (AC) hemoglobin eletrophoresis and a mean corpuscular volume. A sickle solubility test (sickledex) is not sufficient! & Your Baby Only if both you and your partner are tested can you know their baby exactly what kind of hemoglobin condition your next child A S may have A C could have. Look carefully at the inheritance pattern for the possibilities of having a baby with the SC form of sickle cell disease. A A A counselor can tell you if any of your future children could have a form of sickle cell disease. AA (normal hemoglobin) For more information or Contact your local SCDAA organization or other health A C agency at: AC (hemoglobin C trait) or A S Or contact the SCDAA National Office at the address and AS (sickle cell trait) or telephone number below. Stay connected with Get Connected the first patient powered registry S C SC (a type of sickle cell disease) Register at www.getconnectedscd.com It does not matter what their other babies have, their Sickle Cell Disease next one has the same four possibilities: AA, AC, AS, or SC. -

The Role of Methemoglobin and Carboxyhemoglobin in COVID-19: a Review
Journal of Clinical Medicine Review The Role of Methemoglobin and Carboxyhemoglobin in COVID-19: A Review Felix Scholkmann 1,2,*, Tanja Restin 2, Marco Ferrari 3 and Valentina Quaresima 3 1 Biomedical Optics Research Laboratory, Department of Neonatology, University Hospital Zurich, University of Zurich, 8091 Zurich, Switzerland 2 Newborn Research Zurich, Department of Neonatology, University Hospital Zurich, University of Zurich, 8091 Zurich, Switzerland; [email protected] 3 Department of Life, Health and Environmental Sciences, University of L’Aquila, 67100 L’Aquila, Italy; [email protected] (M.F.); [email protected] (V.Q.) * Correspondence: [email protected]; Tel.: +41-4-4255-9326 Abstract: Following the outbreak of a novel coronavirus (SARS-CoV-2) associated with pneumonia in China (Corona Virus Disease 2019, COVID-19) at the end of 2019, the world is currently facing a global pandemic of infections with SARS-CoV-2 and cases of COVID-19. Since severely ill patients often show elevated methemoglobin (MetHb) and carboxyhemoglobin (COHb) concentrations in their blood as a marker of disease severity, we aimed to summarize the currently available published study results (case reports and cross-sectional studies) on MetHb and COHb concentrations in the blood of COVID-19 patients. To this end, a systematic literature research was performed. For the case of MetHb, seven publications were identified (five case reports and two cross-sectional studies), and for the case of COHb, three studies were found (two cross-sectional studies and one case report). The findings reported in the publications show that an increase in MetHb and COHb can happen in COVID-19 patients, especially in critically ill ones, and that MetHb and COHb can increase to dangerously high levels during the course of the disease in some patients. -

Adult, Embryonic and Fetal Hemoglobin Are Expressed in Human Glioblastoma Cells
514 INTERNATIONAL JOURNAL OF ONCOLOGY 44: 514-520, 2014 Adult, embryonic and fetal hemoglobin are expressed in human glioblastoma cells MARWAN EMARA1,2, A. ROBERT TURNER1 and JOAN ALLALUNIS-TURNER1 1Department of Oncology, University of Alberta and Alberta Health Services, Cross Cancer Institute, Edmonton, AB T6G 1Z2, Canada; 2Center for Aging and Associated Diseases, Zewail City of Science and Technology, Cairo, Egypt Received September 7, 2013; Accepted October 7, 2013 DOI: 10.3892/ijo.2013.2186 Abstract. Hemoglobin is a hemoprotein, produced mainly in Introduction erythrocytes circulating in the blood. However, non-erythroid hemoglobins have been previously reported in other cell Globins are hemo-containing proteins, have the ability to types including human and rodent neurons of embryonic bind gaseous ligands [oxygen (O2), nitric oxide (NO) and and adult brain, but not astrocytes and oligodendrocytes. carbon monoxide (CO)] reversibly. They have been described Human glioblastoma multiforme (GBM) is the most aggres- in prokaryotes, fungi, plants and animals with an enormous sive tumor among gliomas. However, despite extensive basic diversity of structure and function (1). To date, hemoglobin, and clinical research studies on GBM cells, little is known myoglobin, neuroglobin (Ngb) and cytoglobin (Cygb) repre- about glial defence mechanisms that allow these cells to sent the vertebrate globin family with distinct function and survive and resist various types of treatment. We have tissue distributions (2). During ontogeny, developing erythro- shown previously that the newest members of vertebrate blasts sequentially express embryonic {[Gower 1 (ζ2ε2), globin family, neuroglobin (Ngb) and cytoglobin (Cygb), are Gower 2 (α2ε2), and Portland 1 (ζ2γ2)] to fetal [Hb F(α2γ2)] expressed in human GBM cells. -

Structure and Function of Leghemoglobins*
203 Structure and function of leghemoglobins* by M. BECANA**, J.F. MORAN, I. ITURBE-ORMAETXE, Y. GOGORCENA and P.R. ESCUREDO Departamento de Nutrición Vegetal, Estación Experimental de Aula Dei (C.S.I.C.), Apartado 202, 50080 Zaragoza Received: 31-10-1994 Key words: Free radicals, Iron, Leghemoglobins, Nitrogen fixation, Oxygen, Plant senescence, Root nodules. Abbreviation: Lb, leghemoglobin. ABSTRACT Becana, M., Moran, J.F., Iturbe-Ormaetxe, I., Gogorcena, Y. and Escuredo, P.R. 1995. Structure and function of leghemoglobins. An. Estac. Exp. Aula Dei (Zaragoza) 21(3): 203-208. Leghemoglobin (Lb) is a myoglobin-like protein of about 16 kDa, which occurs in legume root nodules at very high concentra - tions. Usually the heme moiety is synthesized by the bacteroids but mitochondria may provide also heme for Lb when bacteria are defective in heme production or perhaps when Lb is produced in uninfected cells of nodules. Lb plays an essential role in the nitro - gen fixation process, by providing oxygen to the bacteroids at a low, but constant, concentration, which allows for simultaneous bac - teroid respiration and nitrogenase activity. Lb must be in the reduced, ferrous state to carry oxygen. Several factors within the nodu - les are conducive for Lb oxidation to its ferric, inactive form. During these inactivation reactions free radicals are generated. Howe - ver, healthy nodules contain around 80% of ferrous Lb and 20% of oxyferrous Lb, but not ferric Lb, which indicates that mechanisms exist in the nodules to maintain Lb reduced; these are the enzyme ferric Lb reductase and free flavins. Lb degradation is a largely unk - nown process, but several intermediates with modified hemes,presumably by oxidative attack,have been encountered, including modi - fied Lbam, choleglobin, and biliverdin. -

Hemoglobin C Trait What Does This Mean for My Baby, Me and My Family?
My Baby Has Hemoglobin C Trait What does this mean for my baby, me and my family? Your baby's newborn screening test showed tell them their chance to have a baby with a that he or she has hemoglobin C trait (this is hemoglobin disease. also referred to as being a “hemoglobin C carrier”). Babies who have hemoglobin C trait What does having a baby with hemoglobin are no more likely to get sick than any other C trait mean for me, my partner and for baby. They do not need any special medical future pregnancies? treatment. Hemoglobin C trait will not change Since your baby has hemoglobin C trait, this into a disease later on. means that either you or your partner or both of you have hemoglobin C trait. In almost all What causes hemoglobin C trait? cases, ONLY ONE OF YOU will have Hemoglobin C trait happens when the part of hemoglobin C trait. the red blood cell that carries oxygen throughout the body is changed. This part that Most people do not know that they have is changed is called hemoglobin. Hemoglobin hemoglobin C trait. Now that your baby is is important because it picks up oxygen in the known to have hemoglobin C trait, both you lungs and carries it to the other parts of the and your partner have the option of being body. tested. Testing involves a blood test. People usually have one type of hemoglobin. IF ONLY ONE OF YOU HAS HEMOGLOBIN This is called hemoglobin A. Babies with C TRAIT, in every pregnancy there is a: hemoglobin C trait have a second type of • 1 in 2 (50%) chance to have a baby with hemoglobin called hemoglobin C, as well as only the usual hemoglobin A. -

Chain of Human Neutrophil Cytochrome B CHARLES A
Proc. Nati. Acad. Sci. USA Vol. 85, pp. 3319-3323, May 1988 Biochemistry Primary structure and unique expression of the 22-kilodalton light chain of human neutrophil cytochrome b CHARLES A. PARKOS*, MARY C. DINAUERt, LESLIE E. WALKER*, RODGER A. ALLEN*, ALGIRDAS J. JESAITIS*, AND STUART H. ORKINtt *Department of Immunology, Research Institute of the Scripps Clinic, La Jolla, CA 92037; tDivision of Hematology-Oncology, Children's Hospital, and Dana-Farber Cancer Institute, Department of Pediatrics, Harvard Medical School, Boston, MA 02115; and tHoward Hughes Medical Institute, Children's Hospital, Boston, MA 02115 Communicated by Harvey F. Lodish, January 14, 1988 ABSTRACT Cytochrome b comprising 91-kDa and 22- Cytochrome b purified from neutrophil membranes ap- kDa subunits is a critical component of the membrane-bound pears to be a heterodimer of a glycosylated 91-kDa heavy oxidase of phagocytes that generates superoxide. This impor- chain and a nonglycosylated 22-kDa light chain (10-12). The tant microbicidal system is impaired in inherited disorders 91-kDa subunit is encoded by a gene designated CGD, known as chronic granulomatous disease (CGD). Previously we residing at chromosomal position Xp2l, which originally was determined the sequence of the larger subunit from the cDNA identified on the basis of genetic linkage without reference to of the CGD gene, the X chromosome locus affected in "X- a specific protein product (8). Antisera generated to either a linked" CGD. To complete the primary structure of the synthetic peptide predicted from the cDNA or to a fusion cytochrome b and to assess expression of the smaller subunit, protein produced in E. -

Pathological Conditions Involving Extracellular Hemoglobin
Pathological Conditions Involving Extracellular Hemoglobin: Molecular Mechanisms, Clinical Significance, and Novel Therapeutic Opportunities for alpha(1)-Microglobulin Gram, Magnus; Allhorn, Maria; Bülow, Leif; Hansson, Stefan; Ley, David; Olsson, Martin L; Schmidtchen, Artur; Åkerström, Bo Published in: Antioxidants & Redox Signaling DOI: 10.1089/ars.2011.4282 2012 Link to publication Citation for published version (APA): Gram, M., Allhorn, M., Bülow, L., Hansson, S., Ley, D., Olsson, M. L., Schmidtchen, A., & Åkerström, B. (2012). Pathological Conditions Involving Extracellular Hemoglobin: Molecular Mechanisms, Clinical Significance, and Novel Therapeutic Opportunities for alpha(1)-Microglobulin. Antioxidants & Redox Signaling, 17(5), 813-846. https://doi.org/10.1089/ars.2011.4282 Total number of authors: 8 General rights Unless other specific re-use rights are stated the following general rights apply: Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal Read more about Creative commons licenses: https://creativecommons.org/licenses/ Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. -

Pathogenesis of Hemolytic Anemia in Homozygous Hemoglobin C Disease
Pathogenesis of Hemolytic Anemia in Homozygous Hemoglobin C Disease Samuel Charache, … , Richard J. Ugoretz, J. Richard Spurrell J Clin Invest. 1967;46(11):1795-1811. https://doi.org/10.1172/JCI105670. Research Article Hemoglobin C is less soluble than hemoglobin A in red cells, in hemolysates, and in dilute phosphate buffer. Its relative insolubility may be explained by electrostatic interactions between positively charged β6-lysyl groups and negatively charged groups on adjacent molecules. Red cells from patients with homozygous hemoglobin C (CC) disease exhibit aberrant physical properties which suggest that the cells are more rigid than normal erythrocytes. They pass through membrane filters less readily than normal red cells do, and their viscosity is higher than that of normal cells. Differences from normal cells are exaggerated if mean corpuscular hemoglobin concentration (MCHC) is increased, by suspension in hypertonic salt solution. Increased rigidity of CC cells, by accelerating their fragmentation, may be responsible for formation of microspherocytes. These small dense cells are exceptionally rigid, and probably are even more susceptible to fragmentation and sequestration. Rigidity of CC cells can be attributed to a “precrystalline” state of intracellular hemoglobin, in which crystallization does not occur, although the MCHC exceeds the solubility of hemoglobin in hemolysates. Find the latest version: https://jci.me/105670/pdf The Journal of Clinical Investigation Vol. 46, No. 11, 1967 Pathogenesis of Hemolytic Anemia in Homozygous Hemoglobin C Disease * SAMUEL CHARACHE, C. LOCKARD CONLEY, DAVID F. WAUGH, RICHARD J. UGORETZ,4 AND J. RICHARD SPURRELL WITH THE TECHNICAL ASSISTANCE OF ESTHER GAYLE (From the Department of Medicine, The Johns Hopkins University and Hospital, Baltimore, Maryland, and the Department of Biology, Massachusetts Institute of Technology, Boston, Massachusetts) Abstract. -

Observations on the Minor Basic Hemoglobin Component in the Blood of Normal Individuals and Patients with Thalassemia
Observations on the Minor Basic Hemoglobin Component in the Blood of Normal Individuals and Patients with Thalassemia H. G. Kunkel, … , U. Müller-Eberhard, J. Wolf J Clin Invest. 1957;36(11):1615-1625. https://doi.org/10.1172/JCI103561. Research Article Find the latest version: https://jci.me/103561/pdf OBSERVATIONS ON THE MINOR BASIC HEMOGLOBIN COMPONENT IN THE BLOOD OF NORMAL INDIVIDUALS AND PATIENTS WITH THALASSEMIA BY H. G. KUNKEL, R. CEPPELLINI, U. MULLER-EBERHARD, AND J. WOLF (From the Rockefeller Institute for Medical Research, and Institute for the Study of Human Variation, and the Departmet of Pediatrics, Colunma Uniewsity, N. Y.) (Submitted for publication March 6, 1957; accepted April 11, 1957) In a previous report (1) a second hemoglobin was collected from a number of New York hospitals. was described which was found at a concentration The specimens from patients with thalassemia were ob- of tained from Italian and Greek individuals in the hema- approximately 3 per cent in the blood of normal tology clinic at the Babies Hospital, Columbia-Presby- adult individuals. It was found to resemble he- terian Medical Center, New York. Five individuals with moglobin E in electrophoretic properties, but iden- thalassemia in two families were obtained from index tity with this abnormal hemoglobin was not estab- cases at Bellevue Hospital. The great majority of lished. This same component probably had been thalassemia trait cases were parents of children with observed severe Cooley's anemia. In all instances the diagnosis of by previous investigators employing the thalassemia was based on the hematological picture. classical Tiselius procedure in occasional speci- Several individuals who were suspected of having thalas- mens of blood from normal persons (2, 3) and semia were excluded from the study because of un- thalassemia patients (4), but had not been defined certain hematological findings. -

Chapter 03- Diseases of the Blood and Certain Disorders Involving The
Chapter 3 Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism (D50- D89) Excludes2: autoimmune disease (systemic) NOS (M35.9) certain conditions originating in the perinatal period (P00-P96) complications of pregnancy, childbirth and the puerperium (O00-O9A) congenital malformations, deformations and chromosomal abnormalities (Q00-Q99) endocrine, nutritional and metabolic diseases (E00-E88) human immunodeficiency virus [HIV] disease (B20) injury, poisoning and certain other consequences of external causes (S00-T88) neoplasms (C00-D49) symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (R00-R94) This chapter contains the following blocks: D50-D53 Nutritional anemias D55-D59 Hemolytic anemias D60-D64 Aplastic and other anemias and other bone marrow failure syndromes D65-D69 Coagulation defects, purpura and other hemorrhagic conditions D70-D77 Other disorders of blood and blood-forming organs D78 Intraoperative and postprocedural complications of the spleen D80-D89 Certain disorders involving the immune mechanism Nutritional anemias (D50-D53) D50 Iron deficiency anemia Includes: asiderotic anemia hypochromic anemia D50.0 Iron deficiency anemia secondary to blood loss (chronic) Posthemorrhagic anemia (chronic) Excludes1: acute posthemorrhagic anemia (D62) congenital anemia from fetal blood loss (P61.3) D50.1 Sideropenic dysphagia Kelly-Paterson syndrome Plummer-Vinson syndrome D50.8 Other iron deficiency anemias Iron deficiency anemia due to inadequate dietary -

Sickle Cell Disease
Sickle cell disease Description Sickle cell disease is a group of disorders that affects hemoglobin, the molecule in red blood cells that delivers oxygen to cells throughout the body. People with this disease have atypical hemoglobin molecules called hemoglobin S, which can distort red blood cells into a sickle, or crescent, shape. Signs and symptoms of sickle cell disease usually begin in early childhood. Characteristic features of this disorder include a low number of red blood cells (anemia), repeated infections, and periodic episodes of pain. The severity of symptoms varies from person to person. Some people have mild symptoms, while others are frequently hospitalized for more serious complications. The signs and symptoms of sickle cell disease are caused by the sickling of red blood cells. When red blood cells sickle, they break down prematurely, which can lead to anemia. Anemia can cause shortness of breath, fatigue, and delayed growth and development in children. The rapid breakdown of red blood cells may also cause yellowing of the eyes and skin, which are signs of jaundice. Painful episodes can occur when sickled red blood cells, which are stiff and inflexible, get stuck in small blood vessels. These episodes deprive tissues and organs, such as the lungs, kidneys, spleen, and brain, of oxygen-rich blood and can lead to organ damage. A particularly serious complication of sickle cell disease is high blood pressure in the blood vessels that supply the lungs (pulmonary hypertension), which can lead to heart failure. Pulmonary hypertension occurs in about 10 percent of adults with sickle cell disease. Frequency Sickle cell disease affects millions of people worldwide. -

The Formation of Methemoglobin and Sulfhemoglobin During Sulfanilamide Therapy
THE FORMATION OF METHEMOGLOBIN AND SULFHEMOGLOBIN DURING SULFANILAMIDE THERAPY J. S. Harris, H. O. Michel J Clin Invest. 1939;18(5):507-519. https://doi.org/10.1172/JCI101064. Research Article Find the latest version: https://jci.me/101064/pdf THE FORMATION OF METHEMOGLOBIN AND SULFHEMOGLOBIN DURING SULFANILAMIDE THERAPY By J. S. HARRIS AND H. 0. MICHEL (From the Departments of Pediatrics and Biochemistry, Duke University School of Medicine, Durham) (Received for publication April 8, 1939) Cyanosis almost invariably follows the admin- during the administration of sulfanilamide. Wen- istration of therapeutic amounts of sulfanilamide del (10) found spectroscopic evidence of met- (1). This cyanosis is associated with and is due hemoglobin in every blood sample containing over to a change in the color of the blood. The dark- 4 mgm. per cent sulfanilamide. Evelyn and Mal- ening of the blood is present only in the red cells loy (11) have found that all patients receiving and therefore must be ascribed to one of two sulfanilamide show methemoglobinemia, although causes, a change in the hemoglobin itself or a the intensity is usually very slight. Finally Hart- staining of the red cells with some product formed mann, Perley, and Barnett (12) found cyanosis during the metabolism of sulfanilamide. It is the associated with methemoglobinemia in almost ev- purpose of this paper to assay quantitatively the ery patient receiving over 0.1 gram sulfanilamide effect of sulfanilamide upon the first of these fac- per kilogram of body weight per day. They be- tors-that is, upon the formation of abnormal lieved that the intensity of the methemoglobinemia heme pigments.