Sickle Cell Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diagnosis of Sickle Cell Disease and HBB Haplotyping in the Era of Personalized Medicine: Role of Next Generation Sequencing
Journal of Personalized Medicine Article Diagnosis of Sickle Cell Disease and HBB Haplotyping in the Era of Personalized Medicine: Role of Next Generation Sequencing Adekunle Adekile 1,*, Nagihan Akbulut-Jeradi 2, Rasha Al Khaldi 2, Maria Jinky Fernandez 2 and Jalaja Sukumaran 1 1 Department of Pediatrics, Faculty of Medicine, Kuwait University, P.O. Box 24923, Safat 13110, Kuwait; jalajasukumaran@hotmail 2 Advanced Technology Company, Hawali 32060, Kuwait; [email protected] (N.A.-J.); [email protected] (R.A.); [email protected] (M.J.F.) * Correspondence: [email protected]; Tel.: +965-253-194-86 Abstract: Hemoglobin genotype and HBB haplotype are established genetic factors that modify the clinical phenotype in sickle cell disease (SCD). Current methods of establishing these two factors are cumbersome and/or prone to errors. The throughput capability of next generation sequencing (NGS) makes it ideal for simultaneous interrogation of the many genes of interest in SCD. This study was designed to confirm the diagnosis in patients with HbSS and Sβ-thalassemia, identify any ß-thal mutations and simultaneously determine the ßS HBB haplotype. Illumina Ampliseq custom DNA panel was used to genotype the DNA samples. Haplotyping was based on the alleles on five haplotype-specific SNPs. The patients studied included 159 HbSS patients and 68 Sβ-thal patients, previously diagnosed using high performance liquid chromatography (HPLC). There was Citation: Adekile, A.; considerable discordance between HPLC and NGS results, giving a false +ve rate of 20.5% with a S Akbulut-Jeradi, N.; Al Khaldi, R.; sensitivity of 79% for the identification of Sβthal. -
Hemoglobin C Trait (AC) Hemoglobin Eletrophoresis and a Mean Corpuscular Volume
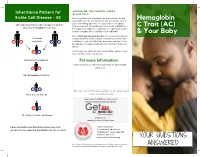
Inheritance Pattern for SHOULD WE, THE PARENTS, TAKE A BLOOD TEST? Sickle Cell Disease - SC Before you have your next baby, we suggest that you and Hemoglobin your partner get special blood test. We all have two sets of genes for hemoglobin. One set is passed on to the baby When one parent has sickle cell trait (AS) and the from each parent. The testing should include, at minimum, a C Trait (AC) other has hemoglobin C trait (AC) hemoglobin eletrophoresis and a mean corpuscular volume. A sickle solubility test (sickledex) is not sufficient! & Your Baby Only if both you and your partner are tested can you know their baby exactly what kind of hemoglobin condition your next child A S may have A C could have. Look carefully at the inheritance pattern for the possibilities of having a baby with the SC form of sickle cell disease. A A A counselor can tell you if any of your future children could have a form of sickle cell disease. AA (normal hemoglobin) For more information or Contact your local SCDAA organization or other health A C agency at: AC (hemoglobin C trait) or A S Or contact the SCDAA National Office at the address and AS (sickle cell trait) or telephone number below. Stay connected with Get Connected the first patient powered registry S C SC (a type of sickle cell disease) Register at www.getconnectedscd.com It does not matter what their other babies have, their Sickle Cell Disease next one has the same four possibilities: AA, AC, AS, or SC. -

The Role of Methemoglobin and Carboxyhemoglobin in COVID-19: a Review
Journal of Clinical Medicine Review The Role of Methemoglobin and Carboxyhemoglobin in COVID-19: A Review Felix Scholkmann 1,2,*, Tanja Restin 2, Marco Ferrari 3 and Valentina Quaresima 3 1 Biomedical Optics Research Laboratory, Department of Neonatology, University Hospital Zurich, University of Zurich, 8091 Zurich, Switzerland 2 Newborn Research Zurich, Department of Neonatology, University Hospital Zurich, University of Zurich, 8091 Zurich, Switzerland; [email protected] 3 Department of Life, Health and Environmental Sciences, University of L’Aquila, 67100 L’Aquila, Italy; [email protected] (M.F.); [email protected] (V.Q.) * Correspondence: [email protected]; Tel.: +41-4-4255-9326 Abstract: Following the outbreak of a novel coronavirus (SARS-CoV-2) associated with pneumonia in China (Corona Virus Disease 2019, COVID-19) at the end of 2019, the world is currently facing a global pandemic of infections with SARS-CoV-2 and cases of COVID-19. Since severely ill patients often show elevated methemoglobin (MetHb) and carboxyhemoglobin (COHb) concentrations in their blood as a marker of disease severity, we aimed to summarize the currently available published study results (case reports and cross-sectional studies) on MetHb and COHb concentrations in the blood of COVID-19 patients. To this end, a systematic literature research was performed. For the case of MetHb, seven publications were identified (five case reports and two cross-sectional studies), and for the case of COHb, three studies were found (two cross-sectional studies and one case report). The findings reported in the publications show that an increase in MetHb and COHb can happen in COVID-19 patients, especially in critically ill ones, and that MetHb and COHb can increase to dangerously high levels during the course of the disease in some patients. -

Thalassemia, Hemophilia & Sickle Cell Disease
10/22/2018 Global Best Practices in Care, Rehabilitation and Research Thalassemia Syndrome Blood Disorders (Thalassemia, Hemophilia & Sickle Cell Disease) Dr. J.S. Arora Thalassemialogist 7% of the world population MSc in Haemoglobinopathy University College London Carry Thalassemia/Hb’pathy gene General secretary: National Thalassemia Welfare Society Federation of Indian Thalassemics Member Ethics Committee: 400 million heterozygous carriers IIT Delhi Lady Hardinge Medical College and Associated Hospitals, New Delhi ITS Dental College Hospital & Research Centre, Greater NOIDA 3,00,000-4,00,000 babies with severe Founder Member: Indian Alliance of Patient Groups haemoglobinopathies born each year. Founding Trustee: Genomics And Public Health Foundation Formerly Coordinator Thalassemia Cell Govt. of Delhi Member Advisory Committee - D D U Hospital Govt. of Delhi INDIA , THAILAND AND INDONESIA “Life Time Service Award” from PHO Chambers of IAP ► 50% OF WORLD’S THALASSAEMIA CARRIERS Patients for Patient Safety (PFPS) Champion India Member: Patients for Patient Safety Advisory Group ► 50% OF THALASSAEMIA MAJORS [email protected] β Thalassemia Who are affected 100 million carriers of β Thalassemia. More than 100,000 Thalassemia Major born/year India • thalassemia : Carrier rate 1% - 17% (mean 3.9%) more prevalent in certain communities. 50 million carriers, Over 12,000 affected born every year. • Sickle Cell Disease : common in tribes carrier rate as high as 40% in some areas • HbE : Highly prevalent in West Bengal & North Eastern -

Section 8: Hematology CHAPTER 47: ANEMIA
Section 8: Hematology CHAPTER 47: ANEMIA Q.1. A 56-year-old man presents with symptoms of severe dyspnea on exertion and fatigue. His laboratory values are as follows: Hemoglobin 6.0 g/dL (normal: 12–15 g/dL) Hematocrit 18% (normal: 36%–46%) RBC count 2 million/L (normal: 4–5.2 million/L) Reticulocyte count 3% (normal: 0.5%–1.5%) Which of the following caused this man’s anemia? A. Decreased red cell production B. Increased red cell destruction C. Acute blood loss (hemorrhage) D. There is insufficient information to make a determination Answer: A. This man presents with anemia and an elevated reticulocyte count which seems to suggest a hemolytic process. His reticulocyte count, however, has not been corrected for the degree of anemia he displays. This can be done by calculating his corrected reticulocyte count ([3% × (18%/45%)] = 1.2%), which is less than 2 and thus suggestive of a hypoproliferative process (decreased red cell production). Q.2. A 25-year-old man with pancytopenia undergoes bone marrow aspiration and biopsy, which reveals profound hypocellularity and virtual absence of hematopoietic cells. Cytogenetic analysis of the bone marrow does not reveal any abnormalities. Despite red blood cell and platelet transfusions, his pancytopenia worsens. Histocompatibility testing of his only sister fails to reveal a match. What would be the most appropriate course of therapy? A. Antithymocyte globulin, cyclosporine, and prednisone B. Prednisone alone C. Supportive therapy with chronic blood and platelet transfusions only D. Methotrexate and prednisone E. Bone marrow transplant Answer: A. Although supportive care with transfusions is necessary for treating this patient with aplastic anemia, most cases are not self-limited. -

Impact of Heterozygous Hemoglobin E on Six Commercial Methods for Hemoglobin A1c Measurement
Impact of heterozygous hemoglobin E on six commercial methods for hemoglobin A1c measurement Sharon Yong1, Hong Liu1, Cindy Lye Teng Lum2, Qian Liu2, Sin Ye Sim3, Felicia Fu Mun Chay3, Wan Ling Cheng4, Siew Fong Neo4, Suru Chew4, Lizhen Ong4, Tze Ping Loh4, Qinde Liu1, Tang Lin Teo1 and Sunil Kumar Sethi4 1 Chemical Metrology Division, Health Sciences Authority, Singapore, Singapore 2 Department of Pathology, Sengkang General Hospital, Singapore, Singapore 3 Department of Laboratory Medicine, Alexandra Hospital, Singapore, Singapore 4 Department of Laboratory Medicine, National University Hospital, Singapore, Singapore ABSTRACT Background: This study examined the impact of heterozygous HbE on HbA1c measurements by six commonly used commercial methods. The results were compared with those from a modified isotope-dilution mass spectrometry (IDMS) reference laboratory method on a liquid chromatograph coupled with tandem mass spectrometer (LC-MS/MS). Methods: Twenty-three leftover samples of patients with heterozygous HbE (HbA1c range: 5.4–11.6%), and nineteen samples with normal hemoglobin (HbA1c range: 5.0–13.7%) were included. The selected commercial methods included the Tina-quant HbA1c Gen. 3 (Roche Diagnostics, Basel, Switzerland), Cobas B 101 (Roche Diagnostics, Basel, Switzerland), D100 (Bio-Rad Laboratories, Hercules, CA, USA), Variant II Turbo HbA1c 2.0 (Bio-Rad Laboratories, Hercules, CA, USA), DCA Vantage (Siemens Healthcare, Erlangen, Germany) and HbA1c Advanced (Beckman Coulter Inc., Brea, CA, USA). Results: With the exception of Cobas B 101 and the Variant II Turbo 2.0, the 95% confidence intervals of the Passing–Bablok regression lines between the results Submitted 25 September 2020 from the six commercial methods and the IDMS method overlapped. -

A Distant Gene Deletion Affects Beta-Globin Gene Function in an Atypical Gamma Delta Beta-Thalassemia
A distant gene deletion affects beta-globin gene function in an atypical gamma delta beta-thalassemia. P Curtin, … , A D Stephens, H Lehmann J Clin Invest. 1985;76(4):1554-1558. https://doi.org/10.1172/JCI112136. Research Article We describe an English family with an atypical gamma delta beta-thalassemia syndrome. Heterozygosity results in a beta-thalassemia phenotype with normal hemoglobin A2. However, unlike previously described cases, no history of neonatal hemolytic anemia requiring blood transfusion was obtained. Gene mapping showed a deletion that extended from the third exon of the G gamma-globin gene upstream for approximately 100 kilobases (kb). The A gamma-globin, psi beta-, delta-, and beta-globin genes in cis remained intact. The malfunction of the beta-globin gene on a chromosome in which the deletion is located 25 kb away suggests that chromatin structure and conformation are important for globin gene expression. Find the latest version: https://jci.me/112136/pdf A Distant Gene Deletion Affects ,8-Globin Gene Function in an Atypical '6y5-Thalassemia Peter Curtin, Mario Pirastu, and Yuet Wai Kan Howard Hughes Medical Institute and Department ofMedicine, University of California, San Francisco, California 94143 John Anderson Gobert-Jones Department ofPathology, West Suffolk County Hospital, Bury St. Edmunds IP33-2QZ, Suffolk, England Adrian David Stephens Department ofHaematology, St. Bartholomew's Hospital, London ECIA-7BE, England Herman Lehmann Department ofBiochemistry, University ofCambridge, Cambridge CB2-lQW, England Abstract tologic picture of f3-thalassemia minor in adult life. Globin syn- thetic studies reveal a ,3 to a ratio of -0.5, but unlike the usual We describe an English family with an atypical 'yS6-thalassemia fl-thalassemia heterozygote, the levels of HbA2 (and HbF) are syndrome. -

Physiology & Biophysics
DEPARTMENTAL RESOURCES The Department of Physiology & Biophysics plays a unique role in biological research. It is in effect a conduit through which the powerful techniques and tools of the physical sciences are brought to bear on significant problems of biological importance. The range of problems being addressed in the Department runs the gamut from understanding functionally important atomic scale motions of proteins to characterizing complex behavior on the cellular through organelle level. The tools being used to pursue these cutting edge problems include state of the art instrumentation for magnetic resonance, laser and synchrotron radiation spectroscopies as well as extensive computer modeling. The strength of the Department stems not only from the significant problems that are being aggressively addressed by the departmental faculty, but also from the resources and the collaborative spirit with the department. The Department houses several world class spectroscopy facilities: Biomolecular Laser Research Center (BLRC) The BLRC is composed of three interrelated laser oriented facilities. The laser spectroscopy facility (LSF) contains an extensive array of state-of-the-art laser spectroscopic tools devoted to studying structure, function and dynamics in isolated biomolecules. The laser imaging and microscopy facility (L1MF) focuses on interfacing laser spectroscopy with microscopy to study complex systems at the molecular level. The third facility, devoted to laser based diagnostic tools for clinical applications, is still in the development stage. Pulsed EPR Facility The EPR facility consists of a number of state-of-the-art spectrometers that have been constructed at Einstein. Both theoretical work and experiments are being carried out to define the structure of metal binding sites in metalloproteins and to determine the orientation and distance of substrates to metal centers at active sites of metalloenzymes. -

Bone Marrow (Stem Cell) Transplant for Sickle Cell Disease Bone Marrow (Stem Cell) Transplant
Bone Marrow (Stem Cell) Transplant for Sickle Cell Disease Bone Marrow (Stem Cell) Transplant for Sickle Cell Disease 1 Produced by St. Jude Children’s Research Hospital Departments of Hematology, Patient Education, and Biomedical Communications. Funds were provided by St. Jude Children’s Research Hospital, ALSAC, and a grant from the Plough Foundation. This document is not intended to take the place of the care and attention of your personal physician. Our goal is to promote active participation in your care and treatment by providing information and education. Questions about individual health concerns or specifi c treatment options should be discussed with your physician. For more general information on sickle cell disease, please visit our Web site at www.stjude.org/sicklecell. Copyright © 2009 St. Jude Children’s Research Hospital How did bone marrow (stem cell) transplants begin for children with sickle cell disease? Bone marrow (stem cell) transplants have been used for the treatment and cure of a variety of cancers, immune system diseases, and blood diseases for many years. Doctors in the United States and other countries have developed studies to treat children who have severe sickle cell disease with bone marrow (stem cell) transplants. How does a bone marrow (stem cell) transplant work? 2 In a person with sickle cell disease, the bone marrow produces red blood cells that contain hemoglobin S. This leads to the complications of sickle cell disease. • To prepare for a bone marrow (stem cell) transplant, strong medicines, called chemotherapy, are used to weaken or destroy the patient’s own bone marrow, stem cells, and infection fi ghting system. -

Anemia in Heart Failure - from Guidelines to Controversies and Challenges
52 Education Anemia in heart failure - from guidelines to controversies and challenges Oana Sîrbu1,*, Mariana Floria1,*, Petru Dascalita*, Alexandra Stoica1,*, Paula Adascalitei, Victorita Sorodoc1,*, Laurentiu Sorodoc1,* *Grigore T. Popa University of Medicine and Pharmacy; Iasi-Romania 1Sf. Spiridon Emergency Hospital; Iasi-Romania ABSTRACT Anemia associated with heart failure is a frequent condition, which may lead to heart function deterioration by the activation of neuro-hormonal mechanisms. Therefore, a vicious circle is present in the relationship of heart failure and anemia. The consequence is reflected upon the pa- tients’ survival, quality of life, and hospital readmissions. Anemia and iron deficiency should be correctly diagnosed and treated in patients with heart failure. The etiology is multifactorial but certainly not fully understood. There is data suggesting that the following factors can cause ane- mia alone or in combination: iron deficiency, inflammation, erythropoietin levels, prescribed medication, hemodilution, and medullar dysfunc- tion. There is data suggesting the association among iron deficiency, inflammation, erythropoietin levels, prescribed medication, hemodilution, and medullar dysfunction. The main pathophysiologic mechanisms, with the strongest evidence-based medicine data, are iron deficiency and inflammation. In clinical practice, the etiology of anemia needs thorough evaluation for determining the best possible therapeutic course. In this context, we must correctly treat the patients’ diseases; according with the current guidelines we have now only one intravenous iron drug. This paper is focused on data about anemia in heart failure, from prevalence to optimal treatment, controversies, and challenges. (Anatol J Cardiol 2018; 20: 52-9) Keywords: anemia, heart failure, intravenous iron, ferric carboxymaltose, quality of life Introduction g/dL in men) (2). -

Your Baby Has Hemoglobin E Or Hemoglobin O Trait for Parents
NEW HAMPSHIRE NEWBORN SCREENING PROGRAM Your Baby Has Hemoglobin E or Hemoglobin O Trait For Parents All infants born in New Hampshire are screened for a panel of conditions at birth. A small amount of blood was collected from your baby’s heel and sent to the laboratory for testing. One of the tests looked at the hemoglobin in your baby’s blood. Your baby’s test found that your baby has either hemoglobin E trait or hemoglobin O trait. The newborn screen- ing test cannot tell the difference between hemoglobin E and hemoglobin O so we do not know which one your baby has. Both hemoglobin E trait and hemoglobin O trait are common and do not cause health problems. Hemoglobin E trait and hemoglobin O trait will never develop to disease. What is hemoglobin? Hemoglobin is the part of the blood that carries oxygen to all parts of the body. There are different types of hemoglobin. The type of hemoglobin we have is determined from genes that we inherit from our parents. Genes are the instructions for how our body develops and functions. We have two copies of each gene; one copy is inherited from our mother in the egg and one copy is inherited from our father in the sperm. What are hemoglobin E trait and hemoglobin O trait? The normal, and most common, type of hemoglobin is called hemoglobin A. Hemoglobin E trait is when a baby inherited one gene for hemoglobin A from one parent and one gene for hemoglobin E from the other parent. -

Eosinophilic Gastroenteritis Presenting with Severe Anemia and Near Syncope
J Am Board Fam Med: first published as 10.3122/jabfm.2012.06.110269 on 7 November 2012. Downloaded from BRIEF REPORT Eosinophilic Gastroenteritis Presenting with Severe Anemia and Near Syncope Nneka Ekunno, DO, MPH, Kirk Munsayac, DO, Allen Pelletier, MD, and Thad Wilkins, MD Eosinophilic gastrointestinal disorders or eosinophilic digestive disorders encompass a spectrum of rare gastrointestinal disorders that includes eosinophilic esophagitis, eosinophilic gastroenteritis, and eosinophilic colitis. Eosinophilic gastroenteritis is a rare inflammatory disease characterized by eosino- philic infiltration of the gastrointestinal tract. The clinical manifestations include anemia, dyspepsia, and diarrhea. Endoscopy with biopsy showing histologic evidence of eosinophilic infiltration is consid- ered definitive for diagnosis. Corticosteroid therapy, food allergen testing, elimination diets, and ele- mental diets are considered effective treatments for eosinophilic gastroenteritis. The treatment and prognosis of eosinophilic gastroenteritis is determined by the severity of the clinical manifestations. We describe a 24-year-old woman with eosinophilic gastroenteritis presenting as epigastric pain with a history of severe iron deficiency anemia, asthma, eczema, and allergic rhinitis, and we review the litera- ture regarding presentation, diagnostic testing, pathophysiology, predisposing factors, and treatment recommendations. (J Am Board Fam Med 2012;25:913–918.) Keywords: Case Reports, Eosinophilic Gastroenteritis, Gastrointestinal Disorders copyright. A 24-year-old nulliparous African-American woman During examination, her height was 62 inches, was admitted after an episode of near syncope asso- weight 117 lb, and body mass index 21.44 kg/m2. Her ciated with 2 days of fatigue and dizziness. She re- heart rate was 111 beats per minute, blood pressure ported gradual onset of dyspepsia over 2 to 3 121/57 mm Hg, respiratory rate 20 breaths per minute, months.