Hemoglobin C Trait What Does This Mean for My Baby, Me and My Family?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Hemoglobin C Trait (AC) Hemoglobin Eletrophoresis and a Mean Corpuscular Volume
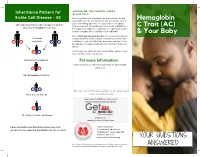
Inheritance Pattern for SHOULD WE, THE PARENTS, TAKE A BLOOD TEST? Sickle Cell Disease - SC Before you have your next baby, we suggest that you and Hemoglobin your partner get special blood test. We all have two sets of genes for hemoglobin. One set is passed on to the baby When one parent has sickle cell trait (AS) and the from each parent. The testing should include, at minimum, a C Trait (AC) other has hemoglobin C trait (AC) hemoglobin eletrophoresis and a mean corpuscular volume. A sickle solubility test (sickledex) is not sufficient! & Your Baby Only if both you and your partner are tested can you know their baby exactly what kind of hemoglobin condition your next child A S may have A C could have. Look carefully at the inheritance pattern for the possibilities of having a baby with the SC form of sickle cell disease. A A A counselor can tell you if any of your future children could have a form of sickle cell disease. AA (normal hemoglobin) For more information or Contact your local SCDAA organization or other health A C agency at: AC (hemoglobin C trait) or A S Or contact the SCDAA National Office at the address and AS (sickle cell trait) or telephone number below. Stay connected with Get Connected the first patient powered registry S C SC (a type of sickle cell disease) Register at www.getconnectedscd.com It does not matter what their other babies have, their Sickle Cell Disease next one has the same four possibilities: AA, AC, AS, or SC. -

Fetal and Embryonic Haemoglobins P
Review Article J Med Genet: first published as 10.1136/jmg.10.1.50 on 1 March 1973. Downloaded from Journal of Medical Genetics (1973). 10, 50. Fetal and Embryonic Haemoglobins P. A. LORKIN MRC Abnormal Haemoglobin Unit, University Department of Biochemistry, Cambridge Haemoglobin has been the subject of intensive form a nearly spherical molecule with extensive research for many years and is one of the most areas of contact between unlike chains; the two thoroughly understood of all protein molecules. main types of contact are denoted alp, and alg2 The amino-acid sequences of haemoglobins from The tetramer exhibits cooperative behaviour or many species of animals have been determined haem-haem interaction. As each haem combines (tabulated by Dayhoff, 1969) and the molecular with oxygen the affinity of successive haems in- structures of horse and human haemoglobins have creases. The oxygen affinity curve of the tetramer been determined in great detail by x-ray crystallo- is sigmoidal and may be represented approximately graphy (Perutz et al, 1968a and b; Perutz 1969). A by the Hill equation:* mechanism of action of haemoglobin has been pro- = kpo2n posed (Perutz, 1970a and b and 1972). The y haemoglobins of higher organisms share a common +kpo2n tetrameric structure built up of two pairs of unlike Oxygen affinity data are usually presented in copyright. chains; the a chains containing 141 amino-acid terms of P102, the partial pressure of oxygen re- residues and the non-a chains containing generally quired to attain half saturation with oxygen, and of 145 or 146 amino acids. In man, five types of n, the exponent of the Hill equation. -

Your Baby Has Hemoglobin E Or Hemoglobin O Trait for Parents
NEW HAMPSHIRE NEWBORN SCREENING PROGRAM Your Baby Has Hemoglobin E or Hemoglobin O Trait For Parents All infants born in New Hampshire are screened for a panel of conditions at birth. A small amount of blood was collected from your baby’s heel and sent to the laboratory for testing. One of the tests looked at the hemoglobin in your baby’s blood. Your baby’s test found that your baby has either hemoglobin E trait or hemoglobin O trait. The newborn screen- ing test cannot tell the difference between hemoglobin E and hemoglobin O so we do not know which one your baby has. Both hemoglobin E trait and hemoglobin O trait are common and do not cause health problems. Hemoglobin E trait and hemoglobin O trait will never develop to disease. What is hemoglobin? Hemoglobin is the part of the blood that carries oxygen to all parts of the body. There are different types of hemoglobin. The type of hemoglobin we have is determined from genes that we inherit from our parents. Genes are the instructions for how our body develops and functions. We have two copies of each gene; one copy is inherited from our mother in the egg and one copy is inherited from our father in the sperm. What are hemoglobin E trait and hemoglobin O trait? The normal, and most common, type of hemoglobin is called hemoglobin A. Hemoglobin E trait is when a baby inherited one gene for hemoglobin A from one parent and one gene for hemoglobin E from the other parent. -

Adult, Embryonic and Fetal Hemoglobin Are Expressed in Human Glioblastoma Cells
514 INTERNATIONAL JOURNAL OF ONCOLOGY 44: 514-520, 2014 Adult, embryonic and fetal hemoglobin are expressed in human glioblastoma cells MARWAN EMARA1,2, A. ROBERT TURNER1 and JOAN ALLALUNIS-TURNER1 1Department of Oncology, University of Alberta and Alberta Health Services, Cross Cancer Institute, Edmonton, AB T6G 1Z2, Canada; 2Center for Aging and Associated Diseases, Zewail City of Science and Technology, Cairo, Egypt Received September 7, 2013; Accepted October 7, 2013 DOI: 10.3892/ijo.2013.2186 Abstract. Hemoglobin is a hemoprotein, produced mainly in Introduction erythrocytes circulating in the blood. However, non-erythroid hemoglobins have been previously reported in other cell Globins are hemo-containing proteins, have the ability to types including human and rodent neurons of embryonic bind gaseous ligands [oxygen (O2), nitric oxide (NO) and and adult brain, but not astrocytes and oligodendrocytes. carbon monoxide (CO)] reversibly. They have been described Human glioblastoma multiforme (GBM) is the most aggres- in prokaryotes, fungi, plants and animals with an enormous sive tumor among gliomas. However, despite extensive basic diversity of structure and function (1). To date, hemoglobin, and clinical research studies on GBM cells, little is known myoglobin, neuroglobin (Ngb) and cytoglobin (Cygb) repre- about glial defence mechanisms that allow these cells to sent the vertebrate globin family with distinct function and survive and resist various types of treatment. We have tissue distributions (2). During ontogeny, developing erythro- shown previously that the newest members of vertebrate blasts sequentially express embryonic {[Gower 1 (ζ2ε2), globin family, neuroglobin (Ngb) and cytoglobin (Cygb), are Gower 2 (α2ε2), and Portland 1 (ζ2γ2)] to fetal [Hb F(α2γ2)] expressed in human GBM cells. -

Alpha Thalassemia Trait
Alpha Thalassemia Trait Alpha Thalassemia Trait Produced by St. Jude Children’s Research Hospital, Departments of Hematology, Patient Education, 1 and Biomedical Communications. Funds were provided by St. Jude Children’s Research Hospital, ALSAC, and a grant from the Plough Foundation. This document is not intended to replace counseling by a trained health care professional or genetic counselor. Our aim is to promote active participation in your care and treatment by providing information and education. Questions about individual health concerns or specific treatment options should be discussed with your doctor. For general information on sickle cell disease and other blood disorders, please visit our Web site at www.stjude.org/sicklecell. Copyright © 2009 St. Jude Children’s Research Hospital Alpha thalassemia trait All red blood cells contain hemoglobin (HEE muh glow bin), which carries oxygen from your lungs to all parts of your body. Alpha thalassemia (thal uh SEE mee uh) trait is a condition that affects the amount of hemo- globin in the red blood cells. • Adult hemoglobin (hemoglobin A) is made of alpha and beta globins. • Normally, people have 4 genes for alpha globin with 2 genes on each chromosome (aa/aa). People with alpha thalassemia trait only have 2 genes for alpha globin, so their bodies make slightly less hemoglobin than normal. This trait was passed on from their parents, like hair color or eye color. A trait is different from a disease 2 Alpha thalassemia trait is not a disease. Normally, a trait will not make you sick. Parents who have alpha thalassemia trait can pass it on to their children. -

Fact Sheettrait Result: Screening Program Blood Spot Screen Result Notification
Family Minnesota Newborn Fact SheetTRAIT Result: Screening program Blood Spot Screen Result Notification FAC - Hemoglobin C Trait What was found on the newborn screen? How do you know if your baby actually has The newborn screen that was collected at birth hemoglobin C trait? found that your baby has fetal hemoglobin (F), adult A simple blood test called a hemoglobin electrophoresis hemoglobin (A), and abnormal hemoglobin (C). can tell if your baby has hemoglobin C trait. This test will likely be performed when your baby is between nine and What does this mean? twelve months of age. Talk with your baby’s doctor about This means your baby likely has hemoglobin C trait (AC). plans for testing and any questions you have about it. The fetal hemoglobin goes away as babies get older. Why is it important to know? What is hemoglobin C trait? When a baby has hemoglobin C trait, we know that Hemoglobin C trait is not a disease and can never at least one parent has it too. Trait is passed on from become a disease. Hemoglobin C trait does not cause parent to child like other genes for eye color and height. health problems. You may have hemoglobin C trait and If only one parent has trait, it is not a problem. However, not know it. People with hemoglobin C trait will always if one parent has hemoglobin C trait and the other has have it; you cannot grow out of it. hemoglobin C trait or sickle cell (S) trait, each pregnancy can result in the child having sickle cell disease. -

Pathological Conditions Involving Extracellular Hemoglobin
Pathological Conditions Involving Extracellular Hemoglobin: Molecular Mechanisms, Clinical Significance, and Novel Therapeutic Opportunities for alpha(1)-Microglobulin Gram, Magnus; Allhorn, Maria; Bülow, Leif; Hansson, Stefan; Ley, David; Olsson, Martin L; Schmidtchen, Artur; Åkerström, Bo Published in: Antioxidants & Redox Signaling DOI: 10.1089/ars.2011.4282 2012 Link to publication Citation for published version (APA): Gram, M., Allhorn, M., Bülow, L., Hansson, S., Ley, D., Olsson, M. L., Schmidtchen, A., & Åkerström, B. (2012). Pathological Conditions Involving Extracellular Hemoglobin: Molecular Mechanisms, Clinical Significance, and Novel Therapeutic Opportunities for alpha(1)-Microglobulin. Antioxidants & Redox Signaling, 17(5), 813-846. https://doi.org/10.1089/ars.2011.4282 Total number of authors: 8 General rights Unless other specific re-use rights are stated the following general rights apply: Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal Read more about Creative commons licenses: https://creativecommons.org/licenses/ Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. -

Increasing Fetal Hemoglobin As a Possible Key for Improvement of Hypoxia and Saving Last Breath in COVID-19 Patient: “Postulating a Hypothesis” Muhamed A
Abdelzaher et al. The Egyptian Journal of Bronchology (2021) 15:33 The Egyptian Journal https://doi.org/10.1186/s43168-021-00078-7 of Bronchology COMMENTARY Open Access Increasing fetal hemoglobin as a possible key for improvement of hypoxia and saving last breath in COVID-19 patient: “postulating a hypothesis” Muhamed A. Abdelzaher1, Ashraf E. S. Ibrahim2 and Essamedin M. Negm3* Abstract Background: COVID-19 patients normally experience mild cold-like symptoms that progress from the early viral response phase through the lung phase to the hyper-inflammation phase. Acute respiratory distress syndrome (ARDS) characterizes the most critical stage of the illness with progressive respiratory failure. Hypoxemia is the most dangerous and challenging problem. We suggest an inductive study approach to postulate a hypothesis and synthesis of supporting evidence as a trial to resolve hypoxia in patients with COVID-19 by increasing the volume of fetal hemoglobin which has a high affinity for oxygen using methods for hypothesis related research evidence synthesis. Conclusion: We recommend involving umbilical cord fetal blood transfusion or the use of hydroxyl urea as a clinical trial on COVID-19 patients and also for all other types of ARDS to determine its efficacy in correction of hypoxemia, controlling progression of the disease, and increasing survival rate. Keywords: COVID-19, Hypoxia, Fetal hemoglobin, Fetal blood, Hydroxyurea Background Mortality are as high as 46% in critically ill patients re- In December 2019, a sudden public health incident (the quiring intensive care unit admission and oxygen ther- corona virus disease [COVID-19] epidemic) occurred in apy [4], suggesting an urgent need to try therapeutic Wuhan, China [1]. -

Pathogenesis of Hemolytic Anemia in Homozygous Hemoglobin C Disease
Pathogenesis of Hemolytic Anemia in Homozygous Hemoglobin C Disease Samuel Charache, … , Richard J. Ugoretz, J. Richard Spurrell J Clin Invest. 1967;46(11):1795-1811. https://doi.org/10.1172/JCI105670. Research Article Hemoglobin C is less soluble than hemoglobin A in red cells, in hemolysates, and in dilute phosphate buffer. Its relative insolubility may be explained by electrostatic interactions between positively charged β6-lysyl groups and negatively charged groups on adjacent molecules. Red cells from patients with homozygous hemoglobin C (CC) disease exhibit aberrant physical properties which suggest that the cells are more rigid than normal erythrocytes. They pass through membrane filters less readily than normal red cells do, and their viscosity is higher than that of normal cells. Differences from normal cells are exaggerated if mean corpuscular hemoglobin concentration (MCHC) is increased, by suspension in hypertonic salt solution. Increased rigidity of CC cells, by accelerating their fragmentation, may be responsible for formation of microspherocytes. These small dense cells are exceptionally rigid, and probably are even more susceptible to fragmentation and sequestration. Rigidity of CC cells can be attributed to a “precrystalline” state of intracellular hemoglobin, in which crystallization does not occur, although the MCHC exceeds the solubility of hemoglobin in hemolysates. Find the latest version: https://jci.me/105670/pdf The Journal of Clinical Investigation Vol. 46, No. 11, 1967 Pathogenesis of Hemolytic Anemia in Homozygous Hemoglobin C Disease * SAMUEL CHARACHE, C. LOCKARD CONLEY, DAVID F. WAUGH, RICHARD J. UGORETZ,4 AND J. RICHARD SPURRELL WITH THE TECHNICAL ASSISTANCE OF ESTHER GAYLE (From the Department of Medicine, The Johns Hopkins University and Hospital, Baltimore, Maryland, and the Department of Biology, Massachusetts Institute of Technology, Boston, Massachusetts) Abstract. -

Observations on the Minor Basic Hemoglobin Component in the Blood of Normal Individuals and Patients with Thalassemia
Observations on the Minor Basic Hemoglobin Component in the Blood of Normal Individuals and Patients with Thalassemia H. G. Kunkel, … , U. Müller-Eberhard, J. Wolf J Clin Invest. 1957;36(11):1615-1625. https://doi.org/10.1172/JCI103561. Research Article Find the latest version: https://jci.me/103561/pdf OBSERVATIONS ON THE MINOR BASIC HEMOGLOBIN COMPONENT IN THE BLOOD OF NORMAL INDIVIDUALS AND PATIENTS WITH THALASSEMIA BY H. G. KUNKEL, R. CEPPELLINI, U. MULLER-EBERHARD, AND J. WOLF (From the Rockefeller Institute for Medical Research, and Institute for the Study of Human Variation, and the Departmet of Pediatrics, Colunma Uniewsity, N. Y.) (Submitted for publication March 6, 1957; accepted April 11, 1957) In a previous report (1) a second hemoglobin was collected from a number of New York hospitals. was described which was found at a concentration The specimens from patients with thalassemia were ob- of tained from Italian and Greek individuals in the hema- approximately 3 per cent in the blood of normal tology clinic at the Babies Hospital, Columbia-Presby- adult individuals. It was found to resemble he- terian Medical Center, New York. Five individuals with moglobin E in electrophoretic properties, but iden- thalassemia in two families were obtained from index tity with this abnormal hemoglobin was not estab- cases at Bellevue Hospital. The great majority of lished. This same component probably had been thalassemia trait cases were parents of children with observed severe Cooley's anemia. In all instances the diagnosis of by previous investigators employing the thalassemia was based on the hematological picture. classical Tiselius procedure in occasional speci- Several individuals who were suspected of having thalas- mens of blood from normal persons (2, 3) and semia were excluded from the study because of un- thalassemia patients (4), but had not been defined certain hematological findings. -

Chapter 03- Diseases of the Blood and Certain Disorders Involving The
Chapter 3 Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism (D50- D89) Excludes2: autoimmune disease (systemic) NOS (M35.9) certain conditions originating in the perinatal period (P00-P96) complications of pregnancy, childbirth and the puerperium (O00-O9A) congenital malformations, deformations and chromosomal abnormalities (Q00-Q99) endocrine, nutritional and metabolic diseases (E00-E88) human immunodeficiency virus [HIV] disease (B20) injury, poisoning and certain other consequences of external causes (S00-T88) neoplasms (C00-D49) symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (R00-R94) This chapter contains the following blocks: D50-D53 Nutritional anemias D55-D59 Hemolytic anemias D60-D64 Aplastic and other anemias and other bone marrow failure syndromes D65-D69 Coagulation defects, purpura and other hemorrhagic conditions D70-D77 Other disorders of blood and blood-forming organs D78 Intraoperative and postprocedural complications of the spleen D80-D89 Certain disorders involving the immune mechanism Nutritional anemias (D50-D53) D50 Iron deficiency anemia Includes: asiderotic anemia hypochromic anemia D50.0 Iron deficiency anemia secondary to blood loss (chronic) Posthemorrhagic anemia (chronic) Excludes1: acute posthemorrhagic anemia (D62) congenital anemia from fetal blood loss (P61.3) D50.1 Sideropenic dysphagia Kelly-Paterson syndrome Plummer-Vinson syndrome D50.8 Other iron deficiency anemias Iron deficiency anemia due to inadequate dietary -

Sickle Cell Disease
Sickle cell disease Description Sickle cell disease is a group of disorders that affects hemoglobin, the molecule in red blood cells that delivers oxygen to cells throughout the body. People with this disease have atypical hemoglobin molecules called hemoglobin S, which can distort red blood cells into a sickle, or crescent, shape. Signs and symptoms of sickle cell disease usually begin in early childhood. Characteristic features of this disorder include a low number of red blood cells (anemia), repeated infections, and periodic episodes of pain. The severity of symptoms varies from person to person. Some people have mild symptoms, while others are frequently hospitalized for more serious complications. The signs and symptoms of sickle cell disease are caused by the sickling of red blood cells. When red blood cells sickle, they break down prematurely, which can lead to anemia. Anemia can cause shortness of breath, fatigue, and delayed growth and development in children. The rapid breakdown of red blood cells may also cause yellowing of the eyes and skin, which are signs of jaundice. Painful episodes can occur when sickled red blood cells, which are stiff and inflexible, get stuck in small blood vessels. These episodes deprive tissues and organs, such as the lungs, kidneys, spleen, and brain, of oxygen-rich blood and can lead to organ damage. A particularly serious complication of sickle cell disease is high blood pressure in the blood vessels that supply the lungs (pulmonary hypertension), which can lead to heart failure. Pulmonary hypertension occurs in about 10 percent of adults with sickle cell disease. Frequency Sickle cell disease affects millions of people worldwide.