Heme Degradation in Pathophysiology of and Countermeasures to Inflammation-Associated Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hemoglobin Variants: Biochemical Properties and Clinical Correlates
Downloaded from http://perspectivesinmedicine.cshlp.org/ on September 29, 2021 - Published by Cold Spring Harbor Laboratory Press Hemoglobin Variants: Biochemical Properties and Clinical Correlates Christopher S. Thom1,2, Claire F. Dickson3, David A. Gell3, and Mitchell J. Weiss2 1Cell and Molecular Biology Graduate Group, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania 19104 2Hematology Department, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania 19104 3Menzies Research Institute, University of Tasmania, Hobart, Australia Correspondence: [email protected] Diseases affecting hemoglobin synthesis and function are extremely common worldwide. More than 1000 naturally occurring human hemoglobin variants with single amino acid substitutions throughout the molecule have been discovered, mainly through their clinical and/or laboratory manifestations. These variants alter hemoglobin structure and biochem- ical properties with physiological effects ranging from insignificant to severe. Studies of these mutations in patients and in the laboratory have produced a wealth of information on he- moglobin biochemistry and biology with significant implications for hematology practice. More generally, landmark studies of hemoglobin performed over the past 60 years have established important paradigms for the disciplines of structural biology, genetics, biochem- istry, and medicine. Here we review the major classes of hemoglobin variants, emphasizing general concepts and illustrative examples. lobin gene mutations affecting hemoglobin stitutions, antitermination mutations, and al- G(Hb), the major blood oxygen (O2) carrier, tered posttranslational processing (Table 1). are common, affecting an estimated 7% of the Naturally occurring Hb mutations cause a world’s population (Weatherall and Clegg 2001; range of biochemical abnormalities, some of Kohne 2011). These mutations are broadly sub- which produce clinically significant symptoms. -

Spectroscopy of Porphyrins
BORIS F. KIM and JOSEPH BOHANDY SPECTROSCOPY OF PORPHYRINS Porphyrins are an important class of compounds that are of interest in molecular biology because of the important roles they play in vital biochemical systems such as biochemical energy conversion in animals, oxygen transport in blood, and photosynthetic energy conversion in plants. We are studying the physical properties of the energy states of porphyrins using the techniques of ex perimental and theoretical spectroscopy with the aim of contributing to a basic understanding of their biochemical behavior. INTRODUCTION Metalloporphin Porphyrins are a class of complex organic chemical compounds found in such diverse places as crude oil, plants, and human beings. They are, in most cases, tailored to carry out vital chemical transformations in intricate biochemical or biophysical systems. They are the key constituents of chlorophyll in plants and of hemoglobin in animals. Without them, life would y be impossible. t Free base porphin These molecules display a wide range of chemical and physical properties that depend on the structural details of the particular porphyrin molecule. All por ~x phyrins are vividly colored and absorb light in the visible and ultraviolet regions of the spectrum. Some exhibit luminescence, paramagnetism, photoconduc tion, or semiconduction. Spme are photosensitizers Wavelength (nanometers) or catalysts. Scientists from several disciplines have been interested in unraveling the principles that cause Fig. 1-The chemical structures for the two forms of por· this diversity of properties. phin are shown on the left. A carbon atom and a hydrogen The simplest compound of all porphyrins is por atom are understood to be at each apex not attached to a nitrogen atom. -

Hemoglobinopathies: Clinical & Hematologic Features And
Hemoglobinopathies: Clinical & Hematologic Features and Molecular Basis Abdullah Kutlar, MD Professor of Medicine Director, Sickle Cell Center Georgia Health Sciences University Types of Normal Human Hemoglobins ADULT FETAL Hb A ( 2 2) 96-98% 15-20% Hb A2 ( 2 2) 2.5-3.5% undetectable Hb F ( 2 2) < 1.0% 80-85% Embryonic Hbs: Hb Gower-1 ( 2 2) Hb Gower-2 ( 2 2) Hb Portland-1( 2 2) Hemoglobinopathies . Qualitative – Hb Variants (missense mutations) Hb S, C, E, others . Quantitative – Thalassemias Decrease or absence of production of one or more globin chains Functional Properties of Hemoglobin Variants . Increased O2 affinity . Decreased O2 affinity . Unstable variants . Methemoglobinemia Clinical Outcomes of Substitutions at Particular Sites on the Hb Molecule . On the surface: Sickle Hb . Near the Heme Pocket: Hemolytic anemia (Heinz bodies) Methemoglobinemia (cyanosis) . Interchain contacts: 1 1 contact: unstable Hbs 1 2 contact: High O2 affinity: erythrocytosis Low O2 affinity: anemia Clinically Significant Hb Variants . Altered physical/chemical properties: Hb S (deoxyhemoglobin S polymerization): sickle syndromes Hb C (crystallization): hemolytic anemia; microcytosis . Unstable Hb Variants: Congenital Heinz body hemolytic anemia (N=141) . Variants with altered Oxygen affinity High affinity variants: erythrocytosis (N=93) Low affinity variants: anemia, cyanosis (N=65) . M-Hemoglobins Methemoglobinemia, cyanosis (N=9) . Variants causing a thalassemic phenotype (N=51) -thalassemia Hb Lepore ( ) fusion Aberrant RNA processing (Hb E, Hb Knossos, Hb Malay) Hyperunstable globins (Hb Geneva, Hb Westdale, etc.) -thalassemia Chain termination mutants (Hb Constant Spring) Hyperunstable variants (Hb Quong Sze) Modified and updated from Bunn & Forget: Hemoglobin: Molecular, Genetic, and Clinical Aspects. WB Saunders, 1986. -
Hemoglobin C Trait (AC) Hemoglobin Eletrophoresis and a Mean Corpuscular Volume
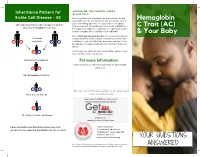
Inheritance Pattern for SHOULD WE, THE PARENTS, TAKE A BLOOD TEST? Sickle Cell Disease - SC Before you have your next baby, we suggest that you and Hemoglobin your partner get special blood test. We all have two sets of genes for hemoglobin. One set is passed on to the baby When one parent has sickle cell trait (AS) and the from each parent. The testing should include, at minimum, a C Trait (AC) other has hemoglobin C trait (AC) hemoglobin eletrophoresis and a mean corpuscular volume. A sickle solubility test (sickledex) is not sufficient! & Your Baby Only if both you and your partner are tested can you know their baby exactly what kind of hemoglobin condition your next child A S may have A C could have. Look carefully at the inheritance pattern for the possibilities of having a baby with the SC form of sickle cell disease. A A A counselor can tell you if any of your future children could have a form of sickle cell disease. AA (normal hemoglobin) For more information or Contact your local SCDAA organization or other health A C agency at: AC (hemoglobin C trait) or A S Or contact the SCDAA National Office at the address and AS (sickle cell trait) or telephone number below. Stay connected with Get Connected the first patient powered registry S C SC (a type of sickle cell disease) Register at www.getconnectedscd.com It does not matter what their other babies have, their Sickle Cell Disease next one has the same four possibilities: AA, AC, AS, or SC. -

Phd Thesis Tjaard Pijning
University of Groningen Divergent or just different Rozeboom, Henriette IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2014 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Rozeboom, H. (2014). Divergent or just different: Structural studies on six different enzymes. [S.n.]. Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). The publication may also be distributed here under the terms of Article 25fa of the Dutch Copyright Act, indicated by the “Taverne” license. More information can be found on the University of Groningen website: https://www.rug.nl/library/open-access/self-archiving-pure/taverne- amendment. Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons the number of authors shown on this cover page is limited to 10 maximum. Download date: 29-09-2021 Divergent or just different Structural studies on six different enzymes Henriëtte Rozeboom Printed by Ipskamp Drukkers, Enschede The research presented in this thesis was carried out in the Protein Crystallography group at the Groningen Biomolecular Sciences and Biotechnology Institute. -

Electronic Spectroscopy of Free Base Porphyrins and Metalloporphyrins
Absorption and Fluorescence Spectroscopy of Tetraphenylporphyrin§ and Metallo-Tetraphenylporphyrin Introduction The word porphyrin is derived from the Greek porphura meaning purple, and all porphyrins are intensely coloured1. Porphyrins comprise an important class of molecules that serve nature in a variety of ways. The Metalloporphyrin ring is found in a variety of important biological system where it is the active component of the system or in some ways intimately connected with the activity of the system. Many of these porphyrins synthesized are the basic structure of biological porphyrins which are the active sites of numerous proteins, whose functions range from oxygen transfer and storage (hemoglobin and myoglobin) to electron transfer (cytochrome c, cytochrome oxidase) to energy conversion (chlorophyll). They also have been proven to be efficient sensitizers and catalyst in a number of chemical and photochemical processes especially photodynamic therapy (PDT). The diversity of their functions is due in part to the variety of metals that bind in the “pocket” of the porphyrin ring system (Fig. 1). Figure 1. Metallated Tetraphenylporphyrin Upon metalation the porphyrin ring system deprotonates, forming a dianionic ligand (Fig. 2). The metal ions behave as Lewis acids, accepting lone pairs of electrons ________________________________ § We all need to thank Jay Stephens for synthesizing the H2TPP 2 from the dianionic porphyrin ligand. Unlike most transition metal complexes, their color is due to absorption(s) within the porphyrin ligand involving the excitation of electrons from π to π* porphyrin ring orbitals. Figure 2. Synthesis of Zn(TPP) The electronic absorption spectrum of a typical porphyrin consists of a strong transition to the second excited state (S0 S2) at about 400 nm (the Soret or B band) and a weak transition to the first excited state (S0 S1) at about 550 nm (the Q band). -

Genetic Modifiers at the Crossroads of Personalised Medicine for Haemoglobinopathies
Journal of Clinical Medicine Article Genetic Modifiers at the Crossroads of Personalised Medicine for Haemoglobinopathies Coralea Stephanou, Stella Tamana , Anna Minaidou, Panayiota Papasavva, , , Marina Kleanthous * y and Petros Kountouris * y Molecular Genetics Thalassaemia Department, The Cyprus Institute of Neurology and Genetics, Nicosia 2371, Cyprus; [email protected] (C.S.); [email protected] (S.T.); [email protected] (A.M.); [email protected] (P.P.) * Correspondence: [email protected] (M.K.); [email protected] (P.K.); Tel.:+357-2239-2652 (M.K.); +357-2239-2623 (P.K.) Equal contribution; Joint last authorship. y Received: 20 September 2019; Accepted: 5 November 2019; Published: 9 November 2019 Abstract: Haemoglobinopathies are common monogenic disorders with diverse clinical manifestations, partly attributed to the influence of modifier genes. Recent years have seen enormous growth in the amount of genetic data, instigating the need for ranking methods to identify candidate genes with strong modifying effects. Here, we present the first evidence-based gene ranking metric (IthaScore) for haemoglobinopathy-specific phenotypes by utilising curated data in the IthaGenes database. IthaScore successfully reflects current knowledge for well-established disease modifiers, while it can be dynamically updated with emerging evidence. Protein–protein interaction (PPI) network analysis and functional enrichment analysis were employed to identify new potential disease modifiers and to evaluate the biological profiles of selected phenotypes. The most relevant gene ontology (GO) and pathway gene annotations for (a) haemoglobin (Hb) F levels/Hb F response to hydroxyurea included urea cycle, arginine metabolism and vascular endothelial growth factor receptor (VEGFR) signalling, (b) response to iron chelators included xenobiotic metabolism and glucuronidation, and (c) stroke included cytokine signalling and inflammatory reactions. -

Tricarboxylic Acid (TCA) Cycle Intermediates: Regulators of Immune Responses
life Review Tricarboxylic Acid (TCA) Cycle Intermediates: Regulators of Immune Responses Inseok Choi , Hyewon Son and Jea-Hyun Baek * School of Life Science, Handong Global University, Pohang, Gyeongbuk 37554, Korea; [email protected] (I.C.); [email protected] (H.S.) * Correspondence: [email protected]; Tel.: +82-54-260-1347 Abstract: The tricarboxylic acid cycle (TCA) is a series of chemical reactions used in aerobic organisms to generate energy via the oxidation of acetylcoenzyme A (CoA) derived from carbohydrates, fatty acids and proteins. In the eukaryotic system, the TCA cycle occurs completely in mitochondria, while the intermediates of the TCA cycle are retained inside mitochondria due to their polarity and hydrophilicity. Under cell stress conditions, mitochondria can become disrupted and release their contents, which act as danger signals in the cytosol. Of note, the TCA cycle intermediates may also leak from dysfunctioning mitochondria and regulate cellular processes. Increasing evidence shows that the metabolites of the TCA cycle are substantially involved in the regulation of immune responses. In this review, we aimed to provide a comprehensive systematic overview of the molecular mechanisms of each TCA cycle intermediate that may play key roles in regulating cellular immunity in cell stress and discuss its implication for immune activation and suppression. Keywords: Krebs cycle; tricarboxylic acid cycle; cellular immunity; immunometabolism 1. Introduction The tricarboxylic acid cycle (TCA, also known as the Krebs cycle or the citric acid Citation: Choi, I.; Son, H.; Baek, J.-H. Tricarboxylic Acid (TCA) Cycle cycle) is a series of chemical reactions used in aerobic organisms (pro- and eukaryotes) to Intermediates: Regulators of Immune generate energy via the oxidation of acetyl-coenzyme A (CoA) derived from carbohydrates, Responses. -

Citric Acid Cycle
CHEM464 / Medh, J.D. The Citric Acid Cycle Citric Acid Cycle: Central Role in Catabolism • Stage II of catabolism involves the conversion of carbohydrates, fats and aminoacids into acetylCoA • In aerobic organisms, citric acid cycle makes up the final stage of catabolism when acetyl CoA is completely oxidized to CO2. • Also called Krebs cycle or tricarboxylic acid (TCA) cycle. • It is a central integrative pathway that harvests chemical energy from biological fuel in the form of electrons in NADH and FADH2 (oxidation is loss of electrons). • NADH and FADH2 transfer electrons via the electron transport chain to final electron acceptor, O2, to form H2O. Entry of Pyruvate into the TCA cycle • Pyruvate is formed in the cytosol as a product of glycolysis • For entry into the TCA cycle, it has to be converted to Acetyl CoA. • Oxidation of pyruvate to acetyl CoA is catalyzed by the pyruvate dehydrogenase complex in the mitochondria • Mitochondria consist of inner and outer membranes and the matrix • Enzymes of the PDH complex and the TCA cycle (except succinate dehydrogenase) are in the matrix • Pyruvate translocase is an antiporter present in the inner mitochondrial membrane that allows entry of a molecule of pyruvate in exchange for a hydroxide ion. 1 CHEM464 / Medh, J.D. The Citric Acid Cycle The Pyruvate Dehydrogenase (PDH) complex • The PDH complex consists of 3 enzymes. They are: pyruvate dehydrogenase (E1), Dihydrolipoyl transacetylase (E2) and dihydrolipoyl dehydrogenase (E3). • It has 5 cofactors: CoASH, NAD+, lipoamide, TPP and FAD. CoASH and NAD+ participate stoichiometrically in the reaction, the other 3 cofactors have catalytic functions. -

Adult, Embryonic and Fetal Hemoglobin Are Expressed in Human Glioblastoma Cells
514 INTERNATIONAL JOURNAL OF ONCOLOGY 44: 514-520, 2014 Adult, embryonic and fetal hemoglobin are expressed in human glioblastoma cells MARWAN EMARA1,2, A. ROBERT TURNER1 and JOAN ALLALUNIS-TURNER1 1Department of Oncology, University of Alberta and Alberta Health Services, Cross Cancer Institute, Edmonton, AB T6G 1Z2, Canada; 2Center for Aging and Associated Diseases, Zewail City of Science and Technology, Cairo, Egypt Received September 7, 2013; Accepted October 7, 2013 DOI: 10.3892/ijo.2013.2186 Abstract. Hemoglobin is a hemoprotein, produced mainly in Introduction erythrocytes circulating in the blood. However, non-erythroid hemoglobins have been previously reported in other cell Globins are hemo-containing proteins, have the ability to types including human and rodent neurons of embryonic bind gaseous ligands [oxygen (O2), nitric oxide (NO) and and adult brain, but not astrocytes and oligodendrocytes. carbon monoxide (CO)] reversibly. They have been described Human glioblastoma multiforme (GBM) is the most aggres- in prokaryotes, fungi, plants and animals with an enormous sive tumor among gliomas. However, despite extensive basic diversity of structure and function (1). To date, hemoglobin, and clinical research studies on GBM cells, little is known myoglobin, neuroglobin (Ngb) and cytoglobin (Cygb) repre- about glial defence mechanisms that allow these cells to sent the vertebrate globin family with distinct function and survive and resist various types of treatment. We have tissue distributions (2). During ontogeny, developing erythro- shown previously that the newest members of vertebrate blasts sequentially express embryonic {[Gower 1 (ζ2ε2), globin family, neuroglobin (Ngb) and cytoglobin (Cygb), are Gower 2 (α2ε2), and Portland 1 (ζ2γ2)] to fetal [Hb F(α2γ2)] expressed in human GBM cells. -

Nobel Lecture by Roger Y. Tsien
CONSTRUCTING AND EXPLOITING THE FLUORESCENT PROTEIN PAINTBOX Nobel Lecture, December 8, 2008 by Roger Y. Tsien Howard Hughes Medical Institute, University of California San Diego, 9500 Gilman Drive, La Jolla, CA 92093-0647, USA. MOTIVATION My first exposure to visibly fluorescent proteins (FPs) was near the end of my time as a faculty member at the University of California, Berkeley. Prof. Alexander Glazer, a friend and colleague there, was the world’s expert on phycobiliproteins, the brilliantly colored and intensely fluorescent proteins that serve as light-harvesting antennae for the photosynthetic apparatus of blue-green algae or cyanobacteria. One day, probably around 1987–88, Glazer told me that his lab had cloned the gene for one of the phycobilipro- teins. Furthermore, he said, the apoprotein produced from this gene became fluorescent when mixed with its chromophore, a small molecule cofactor that could be extracted from dried cyanobacteria under conditions that cleaved its bond to the phycobiliprotein. I remember becoming very excited about the prospect that an arbitrary protein could be fluorescently tagged in situ by genetically fusing it to the phycobiliprotein, then administering the chromophore, which I hoped would be able to cross membranes and get inside cells. Unfortunately, Glazer’s lab then found out that the spontane- ous reaction between the apoprotein and the chromophore produced the “wrong” product, whose fluorescence was red-shifted and five-fold lower than that of the native phycobiliprotein1–3. An enzyme from the cyanobacteria was required to insert the chromophore correctly into the apoprotein. This en- zyme was a heterodimer of two gene products, so at least three cyanobacterial genes would have to be introduced into any other organism, not counting any gene products needed to synthesize the chromophore4. -

Hemoglobin C Trait What Does This Mean for My Baby, Me and My Family?
My Baby Has Hemoglobin C Trait What does this mean for my baby, me and my family? Your baby's newborn screening test showed tell them their chance to have a baby with a that he or she has hemoglobin C trait (this is hemoglobin disease. also referred to as being a “hemoglobin C carrier”). Babies who have hemoglobin C trait What does having a baby with hemoglobin are no more likely to get sick than any other C trait mean for me, my partner and for baby. They do not need any special medical future pregnancies? treatment. Hemoglobin C trait will not change Since your baby has hemoglobin C trait, this into a disease later on. means that either you or your partner or both of you have hemoglobin C trait. In almost all What causes hemoglobin C trait? cases, ONLY ONE OF YOU will have Hemoglobin C trait happens when the part of hemoglobin C trait. the red blood cell that carries oxygen throughout the body is changed. This part that Most people do not know that they have is changed is called hemoglobin. Hemoglobin hemoglobin C trait. Now that your baby is is important because it picks up oxygen in the known to have hemoglobin C trait, both you lungs and carries it to the other parts of the and your partner have the option of being body. tested. Testing involves a blood test. People usually have one type of hemoglobin. IF ONLY ONE OF YOU HAS HEMOGLOBIN This is called hemoglobin A. Babies with C TRAIT, in every pregnancy there is a: hemoglobin C trait have a second type of • 1 in 2 (50%) chance to have a baby with hemoglobin called hemoglobin C, as well as only the usual hemoglobin A.