Chapter 03- Diseases of the Blood and Certain Disorders Involving The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Hemoglobin C Trait (AC) Hemoglobin Eletrophoresis and a Mean Corpuscular Volume
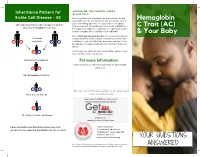
Inheritance Pattern for SHOULD WE, THE PARENTS, TAKE A BLOOD TEST? Sickle Cell Disease - SC Before you have your next baby, we suggest that you and Hemoglobin your partner get special blood test. We all have two sets of genes for hemoglobin. One set is passed on to the baby When one parent has sickle cell trait (AS) and the from each parent. The testing should include, at minimum, a C Trait (AC) other has hemoglobin C trait (AC) hemoglobin eletrophoresis and a mean corpuscular volume. A sickle solubility test (sickledex) is not sufficient! & Your Baby Only if both you and your partner are tested can you know their baby exactly what kind of hemoglobin condition your next child A S may have A C could have. Look carefully at the inheritance pattern for the possibilities of having a baby with the SC form of sickle cell disease. A A A counselor can tell you if any of your future children could have a form of sickle cell disease. AA (normal hemoglobin) For more information or Contact your local SCDAA organization or other health A C agency at: AC (hemoglobin C trait) or A S Or contact the SCDAA National Office at the address and AS (sickle cell trait) or telephone number below. Stay connected with Get Connected the first patient powered registry S C SC (a type of sickle cell disease) Register at www.getconnectedscd.com It does not matter what their other babies have, their Sickle Cell Disease next one has the same four possibilities: AA, AC, AS, or SC. -

Impact of Heterozygous Hemoglobin E on Six Commercial Methods for Hemoglobin A1c Measurement
Impact of heterozygous hemoglobin E on six commercial methods for hemoglobin A1c measurement Sharon Yong1, Hong Liu1, Cindy Lye Teng Lum2, Qian Liu2, Sin Ye Sim3, Felicia Fu Mun Chay3, Wan Ling Cheng4, Siew Fong Neo4, Suru Chew4, Lizhen Ong4, Tze Ping Loh4, Qinde Liu1, Tang Lin Teo1 and Sunil Kumar Sethi4 1 Chemical Metrology Division, Health Sciences Authority, Singapore, Singapore 2 Department of Pathology, Sengkang General Hospital, Singapore, Singapore 3 Department of Laboratory Medicine, Alexandra Hospital, Singapore, Singapore 4 Department of Laboratory Medicine, National University Hospital, Singapore, Singapore ABSTRACT Background: This study examined the impact of heterozygous HbE on HbA1c measurements by six commonly used commercial methods. The results were compared with those from a modified isotope-dilution mass spectrometry (IDMS) reference laboratory method on a liquid chromatograph coupled with tandem mass spectrometer (LC-MS/MS). Methods: Twenty-three leftover samples of patients with heterozygous HbE (HbA1c range: 5.4–11.6%), and nineteen samples with normal hemoglobin (HbA1c range: 5.0–13.7%) were included. The selected commercial methods included the Tina-quant HbA1c Gen. 3 (Roche Diagnostics, Basel, Switzerland), Cobas B 101 (Roche Diagnostics, Basel, Switzerland), D100 (Bio-Rad Laboratories, Hercules, CA, USA), Variant II Turbo HbA1c 2.0 (Bio-Rad Laboratories, Hercules, CA, USA), DCA Vantage (Siemens Healthcare, Erlangen, Germany) and HbA1c Advanced (Beckman Coulter Inc., Brea, CA, USA). Results: With the exception of Cobas B 101 and the Variant II Turbo 2.0, the 95% confidence intervals of the Passing–Bablok regression lines between the results Submitted 25 September 2020 from the six commercial methods and the IDMS method overlapped. -

Tareq Al-Adaily Ibrahim Elhaj Ayah Fraihat Dana Alnasra Sheet
Anemia of decreased production II Sheet 3 – + Hemolytic anemia Dana Alnasra Ayah Fraihat Ibrahim Elhaj Tareq Al-adaily 0 **Flashback to previous lectures: − Anemia is the reduction of oxygen carrying capacity of blood secondary to a decrease in red cell mass. − We classified anemia according to cause into: 1. Anemia of blood loss (chronic and acute) 2. Anemia of decreased production 3. Hemolytic anemia − Then, we mentioned general causes for the anemia of decreased production, which are: nutritional deficiency, chronic inflammation, and bone marrow failure. We’ve already discussed the first two and now we will proceed to the last one. Anemias resulting from bone marrow failure: 1. Aplastic anemia 2. Pure red cell aplasia 3. Myelophthisic anemia 4. Myelodysplastic syndrome Other anemias of decreased production: 1. Anemia of renal failure 2. Anemia of liver disease 3. Anemia of hypothyroidism 00:00 1. Aplastic anemia Is a condition where the multipotent myeloid stem cells produced by the bone marrow are damaged. Remember: the bone marrow has stem cells called myeloid stem cells which eventually differentiate into erythrocytes, megakaryocytes (platelets), and myeloblasts (white blood cells). Notice that lymphocytes are not produced from the myeloid progenitor, therefore, they are not affected. depleted normal 1 | P a g e As a result, the bone marrow becomes depleted of hematopoietic cells. And this is reflected as peripheral blood pancytopenia (all blood cells -including reticulocytes- are decreased, with the exception of lymphocytes). Pathogenesis There are two forms of aplastic anemia according to pathogenesis: a. Acquired aplastic anemia It happens because of an extrinsic factor e.g. -

Physiology & Biophysics
DEPARTMENTAL RESOURCES The Department of Physiology & Biophysics plays a unique role in biological research. It is in effect a conduit through which the powerful techniques and tools of the physical sciences are brought to bear on significant problems of biological importance. The range of problems being addressed in the Department runs the gamut from understanding functionally important atomic scale motions of proteins to characterizing complex behavior on the cellular through organelle level. The tools being used to pursue these cutting edge problems include state of the art instrumentation for magnetic resonance, laser and synchrotron radiation spectroscopies as well as extensive computer modeling. The strength of the Department stems not only from the significant problems that are being aggressively addressed by the departmental faculty, but also from the resources and the collaborative spirit with the department. The Department houses several world class spectroscopy facilities: Biomolecular Laser Research Center (BLRC) The BLRC is composed of three interrelated laser oriented facilities. The laser spectroscopy facility (LSF) contains an extensive array of state-of-the-art laser spectroscopic tools devoted to studying structure, function and dynamics in isolated biomolecules. The laser imaging and microscopy facility (L1MF) focuses on interfacing laser spectroscopy with microscopy to study complex systems at the molecular level. The third facility, devoted to laser based diagnostic tools for clinical applications, is still in the development stage. Pulsed EPR Facility The EPR facility consists of a number of state-of-the-art spectrometers that have been constructed at Einstein. Both theoretical work and experiments are being carried out to define the structure of metal binding sites in metalloproteins and to determine the orientation and distance of substrates to metal centers at active sites of metalloenzymes. -

Your Baby Has Hemoglobin E Or Hemoglobin O Trait for Parents
NEW HAMPSHIRE NEWBORN SCREENING PROGRAM Your Baby Has Hemoglobin E or Hemoglobin O Trait For Parents All infants born in New Hampshire are screened for a panel of conditions at birth. A small amount of blood was collected from your baby’s heel and sent to the laboratory for testing. One of the tests looked at the hemoglobin in your baby’s blood. Your baby’s test found that your baby has either hemoglobin E trait or hemoglobin O trait. The newborn screen- ing test cannot tell the difference between hemoglobin E and hemoglobin O so we do not know which one your baby has. Both hemoglobin E trait and hemoglobin O trait are common and do not cause health problems. Hemoglobin E trait and hemoglobin O trait will never develop to disease. What is hemoglobin? Hemoglobin is the part of the blood that carries oxygen to all parts of the body. There are different types of hemoglobin. The type of hemoglobin we have is determined from genes that we inherit from our parents. Genes are the instructions for how our body develops and functions. We have two copies of each gene; one copy is inherited from our mother in the egg and one copy is inherited from our father in the sperm. What are hemoglobin E trait and hemoglobin O trait? The normal, and most common, type of hemoglobin is called hemoglobin A. Hemoglobin E trait is when a baby inherited one gene for hemoglobin A from one parent and one gene for hemoglobin E from the other parent. -

Redalyc.Anemia in Mexican Women: a Public Health Problem
Salud Pública de México ISSN: 0036-3634 [email protected] Instituto Nacional de Salud Pública México Shamah, Teresa; Villalpando, Salvador; Rivera, Juan A.; Mejía, Fabiola; Camacho, Martha; Monterrubio, Eric A. Anemia in Mexican women: A public health problem Salud Pública de México, vol. 45, núm. Su4, 2003, pp. S499-S507 Instituto Nacional de Salud Pública Cuernavaca, México Available in: http://www.redalyc.org/articulo.oa?id=10609806 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Anemia in Mexican women ORIGINAL ARTICLE Anemia in Mexican women: A public health problem Teresa Shamah-Levy, MSc,(1) Salvador Villalpando, MD, Sc. Dr,(1) Juan A. Rivera, MS, PhD,(1) Fabiola Mejía-Rodríguez, BSc,(1) Martha Camacho-Cisneros, BSc,(1) Eric A Monterrubio, BSc.(1) Shamah-Levy T, Villalpando S, Rivera JA, Shamah-Levy T, Villalpando S, Rivera JA, Mejía-Rodríguez F, Camacho-Cisneros M, Monterrubio EA. Mejía-Rodríguez F, Camacho-Cisneros M, Monterrubio EA. Anemia in Mexican women: A public health problem. Anemia en mujeres mexicanas: un problema de salud pública. Salud Publica Mex 2003;45 suppl 4:S499-S507. Salud Publica Mex 2003;45 supl 4:S499-S507. The English version of this paper is available too at: El texto completo en inglés de este artículo también http://www.insp.mx/salud/index.html está disponible en: http://www.insp.mx/salud/index.html Abstract Resumen Objective. The purpose of this study is to quantify the prev- Objetivo. -

Megaloblastic Anemia Associated with Small Bowel Resection in an Adult Patient
Case Report Megaloblastic Anemia Associated with Small Bowel Resection in an Adult Patient Ajayi Adeleke Ibijola1, Abiodun Idowu Okunlola2 Departments of 1Haematology and 2Surgery, Federal Teaching Hospital, Ido‑Ekiti/Afe Babalola University, Ado‑Ekiti, Nigeria Abstract Megaloblastic anemia is characterized by macro-ovalocytosis, cytopenias, and nucleocytoplasmic maturation asynchrony of marrow erythroblast. The development of megaloblastic anemia is usually insidious in onset, and symptoms are present only in severely anemic patients. We managed a 57-year-old male who presented at the Hematology clinic on account of recurrent anemia associated with paraesthesia involving the lower limbs, 4‑years‑post small bowel resection. Peripheral blood film and bone marrow cytology revealed megaloblastic changes. The anemia and paraesthesia resolved with parenteral cyanocobalamin. Keywords: Bowel resection, megaloblastic anemia, neuropathy, paraesthesia INTRODUCTION affecting mainly the lower extremities which may mimic symptoms of spinal canal stenosis.[1] Megaloblastic anemia Megaloblastic anemia is due to deficiencies of Vitamin B12 and has been reported following small bowel resection in infants or Folic acid. The primary dietary sources of Vitamin B12 are and children but a rare complication of small bowel resection meat, eggs, fish, and dairy products.[1] A normal adult has about in adults.[4,6,7] We highlighted our experience with the clinical 2 to 3 mg of vitamin B12, sufficient for 2–4 years stored in the presentation and management of megaloblastic anemia liver.[2] Pernicious anemia is the most frequent cause of Vitamin secondary to bowel resection. B12 deficiency and it is associated with autoimmune gastric atrophy leading to a reduction in intrinsic factor production. -

Kawasaki Disease with Glucose-6-Phosphate Dehydrogenase Deficiency, Case Report
Saudi Pharmaceutical Journal (2014) xxx, xxx–xxx King Saud University Saudi Pharmaceutical Journal www.ksu.edu.sa www.sciencedirect.com CASE REPORT Kawasaki disease with Glucose-6-Phosphate Dehydrogenase deficiency, case report Hesham Radi Obeidat a,*, Sahar Al-Dossary b, Abdulsalam Asseri a a Pharmacy Department, Saad Specialist Hospital, Alkhobar 31952, Saudi Arabia b Pediatric and Neonatology Department, Saad Specialist Hospital, Alkhobar 31952, Saudi Arabia Received 28 August 2014; accepted 11 November 2014 KEYWORDS Abstract Kawasaki disease (KD) is an acute, self-limited vasculitis of unknown etiology that Kawasaki disease; occurs predominantly in infants and children younger than 5 years of age. Coronary artery abnor- G6PD; malities are the most serious complication. Aspirin Based on the literatures infusion of Intravenous Immunoglobulin of 2 g/kg and a high dose of oral aspirin up to 100 mg/kg/day are the standard treatment for Kawasaki disease in the acute stage, and should be followed by antiplatelet dose of aspirin for thrombocytosis. Glucose-6-Phos- phate Dehydrogenase (G6PD) deficiency is an inherited X-linked hereditary disorder, and aspirin can induce hemolysis in patients with G6PD deficiency. We report a case of a 5 year and 8 month old male with KD and G6PD deficiency. ª 2014 The Authors. Production and hosting by Elsevier B.V. on behalf of King Saud University. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/3.0/). 1. Introduction genetic predisposition or infectious agents are likely to be the cause. Kawasaki disease was first described in 1967 by Tomisaku Recently, guidelines were published by the American Heart Kawasaki and has replaced acute rheumatic fever as the lead- Association (AHA) to aid in the diagnosis and management of ing cause of acquired heart disease among children in devel- Kawasaki disease. -

Iron Supplementation Influence on the Gut Microbiota and Probiotic Intake
nutrients Review Iron Supplementation Influence on the Gut Microbiota and Probiotic Intake Effect in Iron Deficiency—A Literature-Based Review 1, 1 1 Ioana Gabriela Rusu y, Ramona Suharoschi , Dan Cristian Vodnar , 1 1 2,3, 4 Carmen Rodica Pop , Sonia Ancut, a Socaci , Romana Vulturar y, Magdalena Istrati , 5 1 1 1 Ioana Moros, an , Anca Corina Fărcas, , Andreea Diana Kerezsi , Carmen Ioana Mures, an and Oana Lelia Pop 1,* 1 Department of Food Science, University of Agricultural Science and Veterinary Medicine, 400372 Cluj-Napoca, Romania; [email protected] (I.G.R.); [email protected] (R.S.); [email protected] (D.C.V.); [email protected] (C.R.P.); [email protected] (S.A.S.); [email protected] (A.C.F.); [email protected] (A.D.K.); [email protected] (C.I.M.) 2 Department of Molecular Sciences, University of Medicine and Pharmacy Iuliu Hatieganu, 400349 Cluj-Napoca, Romania; [email protected] 3 Cognitive Neuroscience Laboratory, University Babes-Bolyai, 400327 Cluj-Napoca, Romania 4 Regional Institute of Gastroenterology and Hepatology “Prof. Dr. Octavian Fodor”, 400158 Cluj-Napoca, Romania; [email protected] 5 Faculty of Medicine, University of Medicine and Pharmacy “Iuliu Hatieganu”, 400349 Cluj-Napoca, Romania; [email protected] * Correspondence: [email protected]; Tel.: +40-748488933 These authors contributed equally to this work. y Received: 2 June 2020; Accepted: 1 July 2020; Published: 4 July 2020 Abstract: Iron deficiency in the human body is a global issue with an impact on more than two billion individuals worldwide. The most important functions ensured by adequate amounts of iron in the body are related to transport and storage of oxygen, electron transfer, mediation of oxidation-reduction reactions, synthesis of hormones, the replication of DNA, cell cycle restoration and control, fixation of nitrogen, and antioxidant effects. -

Hemolytic Anemia Caused by Hereditary Pyruvate Kinase Deficiency in a West Highland White Terrier Dog
Arch Med Vet 44, 195-200 (2012) COMMUNICATION Hemolytic anemia caused by hereditary pyruvate kinase deficiency in a West Highland White Terrier dog Anemia hemolítica causada por la deficiencia de piruvato quinasa hereditaria en un perro West Highland White Terrier NRC Hlavaca, LA Lacerdaa*, FO Conradob, PS Hünninga, M Seibertc, FHD Gonzálezd, U Gigere aPostgraduate Program in Veterinary Sciences, Universidade Federal Rio Grande do Sul, Porto Alegre, RS, Brasil. bVeterinary Clinic Pathology, Universidade Federal Rio Grande do Sul, Porto Alegre, RS, Brasil. cClinic Pathology, PetLab Ltda, Porto Alegre, Brasil. dDepartment of Veterinary Clinic Pathology, Faculty of Veterinary, Universidade Federal Rio Grande do Sul, Porto Alegre, RS, Brasil. eLaboratory of Genetic Diseases, University of Pennsilvania, Philadelphia, United States. RESUMEN La deficiencia de piruvato quinasa (PK) es un desorden hemolítico autosómico recesivo descrito en perros y gatos. La piruvato quinasa es una de las enzimas regulatorias esenciales de la glicólisis anaeróbica, la deficiencia de esta enzima causa una destrucción prematura de los eritrocitos. El presente es un estudio de caso y relata los hallazgos clínicos y paraclínicos en un perro brasileño de la raza West Highland White Terrier (WHWT) con historia de debilidad e intolerancia al ejercicio. El paciente presentaba mucosas pálidas, anemia hemolítica bastante regenerativa y osteoclerosis. La deficiencia de PK fue confirmada a través de una prueba de ADN raza específica para la inserción 6bp en el extremo 3’ del exón 10 de la secuencia del gen de la piruvato quinasa eritrocitaria (R-PK) como fue descrito. Al perro se le practicó eutanasia a los 20 meses de edad debido al deterioro de su estado clínico, el cual incluyó anemia e incompatibilidad sanguínea. -

Adult, Embryonic and Fetal Hemoglobin Are Expressed in Human Glioblastoma Cells
514 INTERNATIONAL JOURNAL OF ONCOLOGY 44: 514-520, 2014 Adult, embryonic and fetal hemoglobin are expressed in human glioblastoma cells MARWAN EMARA1,2, A. ROBERT TURNER1 and JOAN ALLALUNIS-TURNER1 1Department of Oncology, University of Alberta and Alberta Health Services, Cross Cancer Institute, Edmonton, AB T6G 1Z2, Canada; 2Center for Aging and Associated Diseases, Zewail City of Science and Technology, Cairo, Egypt Received September 7, 2013; Accepted October 7, 2013 DOI: 10.3892/ijo.2013.2186 Abstract. Hemoglobin is a hemoprotein, produced mainly in Introduction erythrocytes circulating in the blood. However, non-erythroid hemoglobins have been previously reported in other cell Globins are hemo-containing proteins, have the ability to types including human and rodent neurons of embryonic bind gaseous ligands [oxygen (O2), nitric oxide (NO) and and adult brain, but not astrocytes and oligodendrocytes. carbon monoxide (CO)] reversibly. They have been described Human glioblastoma multiforme (GBM) is the most aggres- in prokaryotes, fungi, plants and animals with an enormous sive tumor among gliomas. However, despite extensive basic diversity of structure and function (1). To date, hemoglobin, and clinical research studies on GBM cells, little is known myoglobin, neuroglobin (Ngb) and cytoglobin (Cygb) repre- about glial defence mechanisms that allow these cells to sent the vertebrate globin family with distinct function and survive and resist various types of treatment. We have tissue distributions (2). During ontogeny, developing erythro- shown previously that the newest members of vertebrate blasts sequentially express embryonic {[Gower 1 (ζ2ε2), globin family, neuroglobin (Ngb) and cytoglobin (Cygb), are Gower 2 (α2ε2), and Portland 1 (ζ2γ2)] to fetal [Hb F(α2γ2)] expressed in human GBM cells. -

The Hematological Complications of Alcoholism
The Hematological Complications of Alcoholism HAROLD S. BALLARD, M.D. Alcohol has numerous adverse effects on the various types of blood cells and their functions. For example, heavy alcohol consumption can cause generalized suppression of blood cell production and the production of structurally abnormal blood cell precursors that cannot mature into functional cells. Alcoholics frequently have defective red blood cells that are destroyed prematurely, possibly resulting in anemia. Alcohol also interferes with the production and function of white blood cells, especially those that defend the body against invading bacteria. Consequently, alcoholics frequently suffer from bacterial infections. Finally, alcohol adversely affects the platelets and other components of the blood-clotting system. Heavy alcohol consumption thus may increase the drinker’s risk of suffering a stroke. KEY WORDS: adverse drug effect; AODE (alcohol and other drug effects); blood function; cell growth and differentiation; erythrocytes; leukocytes; platelets; plasma proteins; bone marrow; anemia; blood coagulation; thrombocytopenia; fibrinolysis; macrophage; monocyte; stroke; bacterial disease; literature review eople who abuse alcohol1 are at both direct and indirect. The direct in the number and function of WBC’s risk for numerous alcohol-related consequences of excessive alcohol increases the drinker’s risk of serious Pmedical complications, includ- consumption include toxic effects on infection, and impaired platelet produc- ing those affecting the blood (i.e., the the bone marrow; the blood cell pre- tion and function interfere with blood cursors; and the mature red blood blood cells as well as proteins present clotting, leading to symptoms ranging in the blood plasma) and the bone cells (RBC’s), white blood cells from a simple nosebleed to bleeding in marrow, where the blood cells are (WBC’s), and platelets.