Pathological Conditions Involving Extracellular Hemoglobin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hemoglobin Variants: Biochemical Properties and Clinical Correlates
Downloaded from http://perspectivesinmedicine.cshlp.org/ on September 29, 2021 - Published by Cold Spring Harbor Laboratory Press Hemoglobin Variants: Biochemical Properties and Clinical Correlates Christopher S. Thom1,2, Claire F. Dickson3, David A. Gell3, and Mitchell J. Weiss2 1Cell and Molecular Biology Graduate Group, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania 19104 2Hematology Department, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania 19104 3Menzies Research Institute, University of Tasmania, Hobart, Australia Correspondence: [email protected] Diseases affecting hemoglobin synthesis and function are extremely common worldwide. More than 1000 naturally occurring human hemoglobin variants with single amino acid substitutions throughout the molecule have been discovered, mainly through their clinical and/or laboratory manifestations. These variants alter hemoglobin structure and biochem- ical properties with physiological effects ranging from insignificant to severe. Studies of these mutations in patients and in the laboratory have produced a wealth of information on he- moglobin biochemistry and biology with significant implications for hematology practice. More generally, landmark studies of hemoglobin performed over the past 60 years have established important paradigms for the disciplines of structural biology, genetics, biochem- istry, and medicine. Here we review the major classes of hemoglobin variants, emphasizing general concepts and illustrative examples. lobin gene mutations affecting hemoglobin stitutions, antitermination mutations, and al- G(Hb), the major blood oxygen (O2) carrier, tered posttranslational processing (Table 1). are common, affecting an estimated 7% of the Naturally occurring Hb mutations cause a world’s population (Weatherall and Clegg 2001; range of biochemical abnormalities, some of Kohne 2011). These mutations are broadly sub- which produce clinically significant symptoms. -

Hemoglobinopathies: Clinical & Hematologic Features And
Hemoglobinopathies: Clinical & Hematologic Features and Molecular Basis Abdullah Kutlar, MD Professor of Medicine Director, Sickle Cell Center Georgia Health Sciences University Types of Normal Human Hemoglobins ADULT FETAL Hb A ( 2 2) 96-98% 15-20% Hb A2 ( 2 2) 2.5-3.5% undetectable Hb F ( 2 2) < 1.0% 80-85% Embryonic Hbs: Hb Gower-1 ( 2 2) Hb Gower-2 ( 2 2) Hb Portland-1( 2 2) Hemoglobinopathies . Qualitative – Hb Variants (missense mutations) Hb S, C, E, others . Quantitative – Thalassemias Decrease or absence of production of one or more globin chains Functional Properties of Hemoglobin Variants . Increased O2 affinity . Decreased O2 affinity . Unstable variants . Methemoglobinemia Clinical Outcomes of Substitutions at Particular Sites on the Hb Molecule . On the surface: Sickle Hb . Near the Heme Pocket: Hemolytic anemia (Heinz bodies) Methemoglobinemia (cyanosis) . Interchain contacts: 1 1 contact: unstable Hbs 1 2 contact: High O2 affinity: erythrocytosis Low O2 affinity: anemia Clinically Significant Hb Variants . Altered physical/chemical properties: Hb S (deoxyhemoglobin S polymerization): sickle syndromes Hb C (crystallization): hemolytic anemia; microcytosis . Unstable Hb Variants: Congenital Heinz body hemolytic anemia (N=141) . Variants with altered Oxygen affinity High affinity variants: erythrocytosis (N=93) Low affinity variants: anemia, cyanosis (N=65) . M-Hemoglobins Methemoglobinemia, cyanosis (N=9) . Variants causing a thalassemic phenotype (N=51) -thalassemia Hb Lepore ( ) fusion Aberrant RNA processing (Hb E, Hb Knossos, Hb Malay) Hyperunstable globins (Hb Geneva, Hb Westdale, etc.) -thalassemia Chain termination mutants (Hb Constant Spring) Hyperunstable variants (Hb Quong Sze) Modified and updated from Bunn & Forget: Hemoglobin: Molecular, Genetic, and Clinical Aspects. WB Saunders, 1986. -

Supplementary Information Changes in the Plasma Proteome At
Supplementary Information Changes in the plasma proteome at asymptomatic and symptomatic stages of autosomal dominant Alzheimer’s disease Julia Muenchhoff1, Anne Poljak1,2,3, Anbupalam Thalamuthu1, Veer B. Gupta4,5, Pratishtha Chatterjee4,5,6, Mark Raftery2, Colin L. Masters7, John C. Morris8,9,10, Randall J. Bateman8,9, Anne M. Fagan8,9, Ralph N. Martins4,5,6, Perminder S. Sachdev1,11,* Supplementary Figure S1. Ratios of proteins differentially abundant in asymptomatic carriers of PSEN1 and APP Dutch mutations. Mean ratios and standard deviations of plasma proteins from asymptomatic PSEN1 mutation carriers (PSEN1) and APP Dutch mutation carriers (APP) relative to reference masterpool as quantified by iTRAQ. Ratios that significantly differed are marked with asterisks (* p < 0.05; ** p < 0.01). C4A, complement C4-A; AZGP1, zinc-α-2-glycoprotein; HPX, hemopexin; PGLYPR2, N-acetylmuramoyl-L-alanine amidase isoform 2; α2AP, α-2-antiplasmin; APOL1, apolipoprotein L1; C1 inhibitor, plasma protease C1 inhibitor; ITIH2, inter-α-trypsin inhibitor heavy chain H2. 2 A) ADAD)CSF) ADAD)plasma) B) ADAD)CSF) ADAD)plasma) (Ringman)et)al)2015)) (current)study)) (Ringman)et)al)2015)) (current)study)) ATRN↓,%%AHSG↑% 32028% 49% %%%%%%%%HC2↑,%%ApoM↓% 24367% 31% 10083%% %%%%TBG↑,%%LUM↑% 24256% ApoC1↓↑% 16565% %%AMBP↑% 11738%%% SERPINA3↓↑% 24373% C6↓↑% ITIH2% 10574%% %%%%%%%CPN2↓%% ↓↑% %%%%%TTR↑% 11977% 10970% %SERPINF2↓↑% CFH↓% C5↑% CP↓↑% 16566% 11412%% 10127%% %%ITIH4↓↑% SerpinG1↓% 11967% %%ORM1↓↑% SerpinC1↓% 10612% %%%A1BG↑%%% %%%%FN1↓% 11461% %%%%ITIH1↑% C3↓↑% 11027% 19325% 10395%% %%%%%%HPR↓↑% HRG↓% %%% 13814%% 10338%% %%% %ApoA1 % %%%%%%%%%GSN↑% ↓↑ %%%%%%%%%%%%ApoD↓% 11385% C4BPA↓↑% 18976%% %%%%%%%%%%%%%%%%%ApoJ↓↑% 23266%%%% %%%%%%%%%%%%%%%%%%%%%%ApoA2↓↑% %%%%%%%%%%%%%%%%%%%%%%%%%%%%A2M↓↑% IGHM↑,%%GC↓↑,%%ApoB↓↑% 13769% % FGA↓↑,%%FGB↓↑,%%FGG↓↑% AFM↓↑,%%CFB↓↑,%% 19143%% ApoH↓↑,%%C4BPA↓↑% ApoA4↓↑%%% LOAD/MCI)plasma) LOAD/MCI)plasma) LOAD/MCI)plasma) LOAD/MCI)plasma) (Song)et)al)2014)) (Muenchhoff)et)al)2015)) (Song)et)al)2014)) (Muenchhoff)et)al)2015)) Supplementary Figure S2. -

Human Plasma and Recombinant Hemopexins: Heme Binding Revisited
International Journal of Molecular Sciences Article Human Plasma and Recombinant Hemopexins: Heme Binding Revisited Elena Karnaukhova 1,*, Catherine Owczarek 2, Peter Schmidt 2, Dominik J. Schaer 3 and Paul W. Buehler 4,5,* 1 Center for Biologics Evaluation and Research, Food and Drug Administration, Silver Spring, MD 20993, USA 2 CSL Limited, Bio21 Institute, Parkville, Victoria 3010, Australia; [email protected] (C.O.); [email protected] (P.S.) 3 Division of Internal Medicine, University Hospital of Zurich, 8091 Zurich, Switzerland; [email protected] 4 Department of Pathology, The University of Maryland School of Medicine, Baltimore, MD 21201, USA 5 The Center for Blood Oxygen Transport and Hemostasis, Department of Pediatrics, The University of Maryland School of Medicine, Baltimore, MD 21201, USA * Correspondence: [email protected] (E.K.); [email protected] (P.W.B.) Abstract: Plasma hemopexin (HPX) is the key antioxidant protein of the endogenous clearance pathway that limits the deleterious effects of heme released from hemoglobin and myoglobin (the term “heme” is used in this article to denote both the ferrous and ferric forms). During intra-vascular hemolysis, heme partitioning to protein and lipid increases as the plasma concentration of HPX declines. Therefore, the development of HPX as a replacement therapy during high heme stress could be a relevant intervention for hemolytic disorders. A logical approach to enhance HPX yield involves recombinant production strategies from human cell lines. The present study focuses on a biophysical assessment of heme binding to recombinant human HPX (rhHPX) produced in the Expi293FTM (HEK293) cell system. -
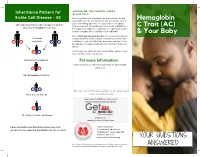
Hemoglobin C Trait (AC) Hemoglobin Eletrophoresis and a Mean Corpuscular Volume
Inheritance Pattern for SHOULD WE, THE PARENTS, TAKE A BLOOD TEST? Sickle Cell Disease - SC Before you have your next baby, we suggest that you and Hemoglobin your partner get special blood test. We all have two sets of genes for hemoglobin. One set is passed on to the baby When one parent has sickle cell trait (AS) and the from each parent. The testing should include, at minimum, a C Trait (AC) other has hemoglobin C trait (AC) hemoglobin eletrophoresis and a mean corpuscular volume. A sickle solubility test (sickledex) is not sufficient! & Your Baby Only if both you and your partner are tested can you know their baby exactly what kind of hemoglobin condition your next child A S may have A C could have. Look carefully at the inheritance pattern for the possibilities of having a baby with the SC form of sickle cell disease. A A A counselor can tell you if any of your future children could have a form of sickle cell disease. AA (normal hemoglobin) For more information or Contact your local SCDAA organization or other health A C agency at: AC (hemoglobin C trait) or A S Or contact the SCDAA National Office at the address and AS (sickle cell trait) or telephone number below. Stay connected with Get Connected the first patient powered registry S C SC (a type of sickle cell disease) Register at www.getconnectedscd.com It does not matter what their other babies have, their Sickle Cell Disease next one has the same four possibilities: AA, AC, AS, or SC. -

Phd Thesis Tjaard Pijning
University of Groningen Divergent or just different Rozeboom, Henriette IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2014 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Rozeboom, H. (2014). Divergent or just different: Structural studies on six different enzymes. [S.n.]. Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). The publication may also be distributed here under the terms of Article 25fa of the Dutch Copyright Act, indicated by the “Taverne” license. More information can be found on the University of Groningen website: https://www.rug.nl/library/open-access/self-archiving-pure/taverne- amendment. Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons the number of authors shown on this cover page is limited to 10 maximum. Download date: 29-09-2021 Divergent or just different Structural studies on six different enzymes Henriëtte Rozeboom Printed by Ipskamp Drukkers, Enschede The research presented in this thesis was carried out in the Protein Crystallography group at the Groningen Biomolecular Sciences and Biotechnology Institute. -

Impact of Heterozygous Hemoglobin E on Six Commercial Methods for Hemoglobin A1c Measurement
Impact of heterozygous hemoglobin E on six commercial methods for hemoglobin A1c measurement Sharon Yong1, Hong Liu1, Cindy Lye Teng Lum2, Qian Liu2, Sin Ye Sim3, Felicia Fu Mun Chay3, Wan Ling Cheng4, Siew Fong Neo4, Suru Chew4, Lizhen Ong4, Tze Ping Loh4, Qinde Liu1, Tang Lin Teo1 and Sunil Kumar Sethi4 1 Chemical Metrology Division, Health Sciences Authority, Singapore, Singapore 2 Department of Pathology, Sengkang General Hospital, Singapore, Singapore 3 Department of Laboratory Medicine, Alexandra Hospital, Singapore, Singapore 4 Department of Laboratory Medicine, National University Hospital, Singapore, Singapore ABSTRACT Background: This study examined the impact of heterozygous HbE on HbA1c measurements by six commonly used commercial methods. The results were compared with those from a modified isotope-dilution mass spectrometry (IDMS) reference laboratory method on a liquid chromatograph coupled with tandem mass spectrometer (LC-MS/MS). Methods: Twenty-three leftover samples of patients with heterozygous HbE (HbA1c range: 5.4–11.6%), and nineteen samples with normal hemoglobin (HbA1c range: 5.0–13.7%) were included. The selected commercial methods included the Tina-quant HbA1c Gen. 3 (Roche Diagnostics, Basel, Switzerland), Cobas B 101 (Roche Diagnostics, Basel, Switzerland), D100 (Bio-Rad Laboratories, Hercules, CA, USA), Variant II Turbo HbA1c 2.0 (Bio-Rad Laboratories, Hercules, CA, USA), DCA Vantage (Siemens Healthcare, Erlangen, Germany) and HbA1c Advanced (Beckman Coulter Inc., Brea, CA, USA). Results: With the exception of Cobas B 101 and the Variant II Turbo 2.0, the 95% confidence intervals of the Passing–Bablok regression lines between the results Submitted 25 September 2020 from the six commercial methods and the IDMS method overlapped. -

Physiology & Biophysics
DEPARTMENTAL RESOURCES The Department of Physiology & Biophysics plays a unique role in biological research. It is in effect a conduit through which the powerful techniques and tools of the physical sciences are brought to bear on significant problems of biological importance. The range of problems being addressed in the Department runs the gamut from understanding functionally important atomic scale motions of proteins to characterizing complex behavior on the cellular through organelle level. The tools being used to pursue these cutting edge problems include state of the art instrumentation for magnetic resonance, laser and synchrotron radiation spectroscopies as well as extensive computer modeling. The strength of the Department stems not only from the significant problems that are being aggressively addressed by the departmental faculty, but also from the resources and the collaborative spirit with the department. The Department houses several world class spectroscopy facilities: Biomolecular Laser Research Center (BLRC) The BLRC is composed of three interrelated laser oriented facilities. The laser spectroscopy facility (LSF) contains an extensive array of state-of-the-art laser spectroscopic tools devoted to studying structure, function and dynamics in isolated biomolecules. The laser imaging and microscopy facility (L1MF) focuses on interfacing laser spectroscopy with microscopy to study complex systems at the molecular level. The third facility, devoted to laser based diagnostic tools for clinical applications, is still in the development stage. Pulsed EPR Facility The EPR facility consists of a number of state-of-the-art spectrometers that have been constructed at Einstein. Both theoretical work and experiments are being carried out to define the structure of metal binding sites in metalloproteins and to determine the orientation and distance of substrates to metal centers at active sites of metalloenzymes. -

Your Baby Has Hemoglobin E Or Hemoglobin O Trait for Parents
NEW HAMPSHIRE NEWBORN SCREENING PROGRAM Your Baby Has Hemoglobin E or Hemoglobin O Trait For Parents All infants born in New Hampshire are screened for a panel of conditions at birth. A small amount of blood was collected from your baby’s heel and sent to the laboratory for testing. One of the tests looked at the hemoglobin in your baby’s blood. Your baby’s test found that your baby has either hemoglobin E trait or hemoglobin O trait. The newborn screen- ing test cannot tell the difference between hemoglobin E and hemoglobin O so we do not know which one your baby has. Both hemoglobin E trait and hemoglobin O trait are common and do not cause health problems. Hemoglobin E trait and hemoglobin O trait will never develop to disease. What is hemoglobin? Hemoglobin is the part of the blood that carries oxygen to all parts of the body. There are different types of hemoglobin. The type of hemoglobin we have is determined from genes that we inherit from our parents. Genes are the instructions for how our body develops and functions. We have two copies of each gene; one copy is inherited from our mother in the egg and one copy is inherited from our father in the sperm. What are hemoglobin E trait and hemoglobin O trait? The normal, and most common, type of hemoglobin is called hemoglobin A. Hemoglobin E trait is when a baby inherited one gene for hemoglobin A from one parent and one gene for hemoglobin E from the other parent. -

Genetic Modifiers at the Crossroads of Personalised Medicine for Haemoglobinopathies
Journal of Clinical Medicine Article Genetic Modifiers at the Crossroads of Personalised Medicine for Haemoglobinopathies Coralea Stephanou, Stella Tamana , Anna Minaidou, Panayiota Papasavva, , , Marina Kleanthous * y and Petros Kountouris * y Molecular Genetics Thalassaemia Department, The Cyprus Institute of Neurology and Genetics, Nicosia 2371, Cyprus; [email protected] (C.S.); [email protected] (S.T.); [email protected] (A.M.); [email protected] (P.P.) * Correspondence: [email protected] (M.K.); [email protected] (P.K.); Tel.:+357-2239-2652 (M.K.); +357-2239-2623 (P.K.) Equal contribution; Joint last authorship. y Received: 20 September 2019; Accepted: 5 November 2019; Published: 9 November 2019 Abstract: Haemoglobinopathies are common monogenic disorders with diverse clinical manifestations, partly attributed to the influence of modifier genes. Recent years have seen enormous growth in the amount of genetic data, instigating the need for ranking methods to identify candidate genes with strong modifying effects. Here, we present the first evidence-based gene ranking metric (IthaScore) for haemoglobinopathy-specific phenotypes by utilising curated data in the IthaGenes database. IthaScore successfully reflects current knowledge for well-established disease modifiers, while it can be dynamically updated with emerging evidence. Protein–protein interaction (PPI) network analysis and functional enrichment analysis were employed to identify new potential disease modifiers and to evaluate the biological profiles of selected phenotypes. The most relevant gene ontology (GO) and pathway gene annotations for (a) haemoglobin (Hb) F levels/Hb F response to hydroxyurea included urea cycle, arginine metabolism and vascular endothelial growth factor receptor (VEGFR) signalling, (b) response to iron chelators included xenobiotic metabolism and glucuronidation, and (c) stroke included cytokine signalling and inflammatory reactions. -

MASSHEALTH TRANSMITTAL LETTER LAB-22 July 2002 TO
Commonwealth of Massachusetts Executive Office of Health and Human Services Division of Medical Assistance 600 Washington Street Boston, MA 02111 www.mass.gov/dma MASSHEALTH TRANSMITTAL LETTER LAB-22 July 2002 TO: Independent Clinical Laboratories Participating in MassHealth FROM: Wendy E. Warring, Commissioner RE: Independent Clinical Laboratory Manual (Laboratory HCPCS) The federal government has revised the HCFA Common Procedure Coding System (HCPCS) for MassHealth billing. This letter transmits changes for your provider manual that contain the new and revised codes. The revised Subchapter 6 is effective for dates of service on or after April 30, 2002. The codes introduced under the 2002 HCPCS code book are effective for dates of service on or after April 30, 2002. We will accept either the new or the old codes for dates of service through July 28, 2002. For dates of service on or after July 29, 2002, you must use the new codes to receive payment. If you wish to obtain a fee schedule, you may purchase Division of Health Care Finance and Policy regulations from either the Massachusetts State Bookstore or from the Division of Health Care Finance and Policy (see addresses and telephone numbers below). You must contact them first to find out the price of the publication. The Division of Health Care Finance and Policy also has the regulations available on disk. The regulation title for laboratory is 114.3 CMR 20.00: Laboratory. Massachusetts State Bookstore Division of Health Care Finance and Policy State House, Room 116 Two Boylston Street -

Implication of Globin Gene Expression, Hemoglobin F and Hemoglobin E Levels on Β-Thalassemia/Hb E Disease Severity
Available online at www.aNNclinlabsci.org Annals of Clinical & Laboratory Science, vol. 44, no. 4, 2014 437 Implication of Globin Gene Expression, Hemoglobin F and Hemoglobin E Levels on β-Thalassemia/Hb E Disease Severity Suwimol Siriworadechkul1, Sumalee Jindadamrongwech1, SuporN Chuncharunee2, and Saranya Aupparakkitanon1 1Department of Pathology and 2Department of Medicine, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand Abstract. One of the factors affecting the degree of severity in β-thalassemia disease is the presence of un- matched α-hemoglobin chains. Thus, the expression levels of globin genes in reticulocytes of β-thalassemia subjects were measured using quantitative RT-PCR, demonstrating that α/β globin mRNA ratio, as well as levels of γ-globin mRNA and Hb F, increased with progressing degree of β globin synthesis defect. The levels of γ-globin mRNA and Hb F could not be directly correlated with severity of β-thalassemia/Hb E disease due to a low statistical power of this analysis. Higher levels of Hb E were present, however, in clini- cally mild patients, as compared to moderately severe β-thalassemia/Hb E subjects. This suggests that in β-thalassemia/Hb E disease, elevation of Hb E level through enhancing correctly spliced βE-globin mRNA offers another approach in ameliorating disease severity. In addition, co-inheritance of α-thalassemia 2 trait in β-thalassemia/Hb E subjects was associated with milder outcome compared with those with the same β-thalassemia genotypes, confirming the notion of the beneficial effect of a more balanced α:β-globin chain ratio. Key words: Globin gene expression, Hemoglobin E, Hemoglobin F, β-thalassemia, modifying factor.