Study on Various Types of Infections Related to Balanitis in Circumcised Or Uncircumcised Male and Its Causes, Symptoms and Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Male Reproductive System
Management of Men’s Reproductive 3 Health Problems Men’s Reproductive Health Curriculum Management of Men’s Reproductive 3 Health Problems © 2003 EngenderHealth. All rights reserved. 440 Ninth Avenue New York, NY 10001 U.S.A. Telephone: 212-561-8000 Fax: 212-561-8067 e-mail: [email protected] www.engenderhealth.org This publication was made possible, in part, through support provided by the Office of Population, U.S. Agency for International Development (USAID), under the terms of cooperative agreement HRN-A-00-98-00042-00. The opinions expressed herein are those of the publisher and do not necessarily reflect the views of USAID. Cover design: Virginia Taddoni ISBN 1-885063-45-8 Printed in the United States of America. Printed on recycled paper. Library of Congress Cataloging-in-Publication Data Men’s reproductive health curriculum : management of men’s reproductive health problems. p. ; cm. Companion v. to: Introduction to men’s reproductive health services, and: Counseling and communicating with men. Includes bibliographical references. ISBN 1-885063-45-8 1. Andrology. 2. Human reproduction. 3. Generative organs, Male--Diseases--Treatment. I. EngenderHealth (Firm) II. Counseling and communicating with men. III. Title: Introduction to men’s reproductive health services. [DNLM: 1. Genital Diseases, Male. 2. Physical Examination--methods. 3. Reproductive Health Services. WJ 700 M5483 2003] QP253.M465 2003 616.6’5--dc22 2003063056 Contents Acknowledgments v Introduction vii 1 Disorders of the Male Reproductive System 1.1 The Male -

Assessment of Lower Urinary Tract Symptoms in Younger Men
MEN’S HEALTH ASSESSMENT OF LOWER URINARY TRACT SYMPTOMS IN YOUNGER MEN Lower urinary tract symptoms (LUTS) are common in the ageing male and represent a significant burden on both the patient and the healthcare system worldwide. 1,2 Accordingly, the majority of clinical trials and guidelines focus on the older patient, despite the fact that men below these ages will also present with many of the same symptoms. In this review, the authors explore the challenges of assessing and managing men below 50 years with LUTS. Dr Odunayo The aetiology of LUTS is multifactorial with causes How common are LUTS Kalejaiye attributed to dysfunction of the bladder and its in younger men? Urology SpR outlet – including the prostate, urethra and sphincter; The EPIC study, 3 a population-based survey which the neurological innervation of the lower urinary recruited men aged over 18 years, found that the Professor tract, and medical co-morbidities.1,2 It is important prevalence of LUTS increased with age, from 51.3% Raj Persad to consider all these aspects when assessing patients. in men aged 18-39 years to 62% in those aged 40-59 While in older men, benign prostatic enlargement years. This is compared with a prevalence of 80.7% Consultant is the commonest cause of male LUTS, in younger in men aged 60 years or older. Storage symptoms Urologist; men this is unusual, and other diagnoses should be were commonest in men 39 years or younger, with a Honorary considered more likely. prevalence of 37.5%, compared with a prevalence of Professor of 19.9% for voiding symptoms in this age group. -
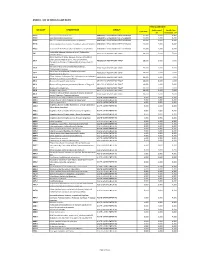
Annex 1: List of Medical Case Rates
ANNEX 1. LIST OF MEDICAL CASE RATES FIRST CASE RATE ICD CODE DESCRIPTION GROUP Professional Health Care Case Rate Fee Institution Fee P91.3 Neonatal cerebral irritability ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.4 Neonatal cerebral depression ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.6 Hypoxic ischemic encephalopathy of newborn ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.8 Other specified disturbances of cerebral status of newborn ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.9 Disturbance of cerebral status of newborn, unspecified ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 Peritonsillar abscess; Abscess of tonsil; Peritonsillar J36 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 cellulitis; Quinsy Other diseases of larynx; Abscess of larynx; Cellulitis of larynx; Disease NOS of larynx; Necrosis of larynx; J38.7 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Pachyderma of larynx; Perichondritis of larynx; Ulcer of larynx Retropharyngeal and parapharyngeal abscess; J39.0 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Peripharyngeal abscess Other abscess of pharynx; Cellulitis of pharynx; J39.1 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Nasopharyngeal abscess Other diseases of pharynx; Cyst of pharynx or nasopharynx; J39.2 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Oedema of pharynx or nasopharynx J85.1 Abscess of lung with pneumonia ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 J85.2 Abscess of lung without pneumonia; Abscess of lung NOS ABSCESS OF RESPIRATORY -

Natural Remedies of Common Human Parasites and Pathogens
ACTA SCIENTIFIC MICROBIOLOGY (ISSN: 2581-3226) Volume 2 Issue 11 November 2019 Investigation Paper Natural Remedies of Common Human Parasites and Pathogens Omar M Amin* Parasitology Center, Scottsdale, Arizona *Corresponding Author: Omar M Amin, Parasitology Center, Scottsdale, Arizona. Received: July 12, 2019; Published: October 16, 2019 DOI: 10.31080/ASMI.2019.02.0401 • Bleeding. • Appetite changes. • Malabsorption. • Mucus. • Rectal itching. • Gut leakage. • Poor digestion. • Systemic/other symptoms • Fatigue. • Skin rash. • Dry cough. • Brain fog/memory loss. • Lymph blockage. Figure 1 • Allergies. • Nausea. Diagnosis and management of: • Muscle or joint pain. • Parasitic organisms and agents of medical and public • Dermatitis. health importance in fecal, blood, skin, urine specimens. • Headaches. • Toxicities related to Neurocutaneous Syndrome (NCS). • Insomnia. Development of anti-parasitic herbal products (F/C/R) Edu- How we get infected cational services: workshops, seminars, training and publications Drinking water or juice: Giardia, Cryptosporidium. provided. 1. 2. Skin contact with contaminated water: Schistosomi- Consultations and protocols for herbal and allopathic treat- asis, swimmers itch. ments. Research: over 220 publications on parasites from all con- Food (fecal-oral infections): most protozoans, ex., tinents. 3. Blastocysts, Entamoeba spp. and worms: Ascaris. Why test? 4. Arthropods: Lyme disease, plague, typhus, etc. You need to be tested if you have one or more of these symp- 5. Air: Upper respiratory tract infections (viruses, bac- toms: teria), ex GI symptoms 6. Pets: Hydatid., flu, Valleycyst disease,fever, Hanta heart virus. worm, larva mi- grans (dogs), Toxoplasma (cats), Taenia (beef, swine. • Diarrhea/constipation. People (contagious diseases): AIDS, herpes. • Irritable bowel 7. Soil: hook worms, thread worms. • Cramps 8. -

Cutaneous Balamuthia Mandrillaris Infection As a Precursor To
Volume 23 Number 7 | July 2017 Dermatology Online Journal || Case Report DOJ 23 (7): 4 Cutaneous Balamuthia mandrillaris infection as a precursor to Balamuthia amoebic encephalitis (BAE) in a healthy 84-year-old Californian Larisa M Lehmer, Gabriel E Ulibarri, Bruce D Ragsdale, James Kunkle Affiliations: University of California Irvine Health, Department of Dermatology, Irvine, California, Central Coast Pathology Laboratory, San Luis Obispo, California, Western Diagnostic Services Laboratory, San Luis Obispo, California, Central Coast Dermatology, Arroyo Grande, California Corresponding Author: Larisa M Lehmer, Department of Dermatology, UC Irvine Health, 118 Med Surg 1, Irvine, CA 92697-2400, Email: [email protected] Abstract Keywords: Balamuthia mandrillaris; cutaneous balamuthiasis; granulomatous amoebic encephalitis; Soil and freshwater-dwelling amoebae may GAE; balamuthia amoebic encephalitis; BAE; opportunistically infect the skin and evoke a immunocompromise; granulomatous dermatitis; granulomatous dermatitis that camouflages their immune senescence. underlying morphology. Amoebic infestations are incredibly rare in the U.S., predominantly occurring in the young, elderly, and immunocompromised. Introduction Sadly, because diagnosis is difficult and unsuspected, Balamuthia mandrillaris (B. mandrillaris), along most cases are diagnosed at autopsy. The following with Naegleria, Sappinia and several species of case is of a healthy 84-year-old man with a non- Acanthomeba, are free-living amoebae found in fresh healing nodulo-ulcerative cutaneous lesion on his water and soil worldwide that may opportunistically left forearm that appeared following a gardening infect the skin and/or central nervous system (CNS) injury. Lesional punch biopsies repeatedly showed of humans. The first sign of infection ranges from non-specific granulomatous inflammation with a stubborn indurated plaque or ulceration on the no pathogens evident histologically or by culture. -

Sexual Function Considerations in Penile Reconstructive Surgery
ARTICOLO ORIGINALE / ORIGINAL ARTICLE GIMSeR 2008;15:1-13 Sexual function considerations in penile reconstructive surgery Funzione sessuale: considerazioni in chirurgia ricostruttiva del pene G. GARAFFA, N. CHRISTOPHER, D.J. RALPH St. Peter’s Department of Andrology, The Institute of Urology, University College London Hospitals, Ground floor, Rosenheim Wing, London, England Key words: Peyronie’s disease, Penile cancer, Balanitis xerotica obliterans, Penile trauma, Penile amputation, Penile fracture Parole chiave: Malattia di La Peyronie, Cancro peniena, Balanite obliterante erotica, Trauma penieno, Amputazione peniena, Frattura peniena Summary The aim of this paper is to give a concise overview of surgical techniques used to manage Peyronie’s disease, penile squamous cell carcinoma, penile trauma, fracture and amputation of the penis, and balanitis xerotica obliterans. Our methodology involved a PubMed-based review of the last 20 years literature regarding the management of the above conditions. From the literature analysis we extrapolated the surgical strategies providing the best outcomes in terms if sexual function. Riassunto Scopo di questa minireview è fornire una panoramica delle tecniche chirurgiche utilizzate nel trattamento di: malattia di La Peyro- nie, carcinoma squamoso del pene, trauma e frattura peniene, amputazione del pene e balanitis xerotica obliterans. A questo scopo abbiamo valutato la letteratura degli ultimi 20 anni presente in PubMed relativa alla chirurgia delle patologie so- pramenzionate. Nell’ambito della nostra -

Die Prinzipien Der Chirurgischen Therapie Beim Fortgeschrittenen
Aus der Chirurgischen Klinik und Poliklinik - Innenstadt, der Ludwig-Maximilian- Universität-München Direktor: Prof. Dr. med. Wolf Mutschler Die Prinzipien der chirurgischen Therapie beim fortgeschrittenen Pyoderma gangränosum Dissertation zum Erwerb des Doktorgrades der Medizin an der Medizinischen Fakultät der Ludwig-Maximilians-Universität zu München vorgelegt von Christoph Hendrik Volkering aus Groß-Gerau 2008 Mit Genehmigung der Medizinischen Fakultät der Universität München Berichterstatter: Prof. Dr. Sigurd Keßler Mitberichterstatter: Prof. Dr. Hans C. Korting Priv. Doz. Dr. Martin K. Angele Dekan: Prof. Dr. med. Dr. h.c. Maximilian Reiser, FACR Tag der mündlichen Prüfung: 20.11.2008 - 2 - INHALT 1. Einleitung: ........................................................................................................... - 6 - 1.1. Das Pyoderma gangränosum: ..................................................................... - 6 - 1.1.1. Geschichte: ......................................................................................... - 6 - 1.1.2. Inzidenz: ............................................................................................. - 6 - 1.1.3. Assoziierte Erkrankungen: .................................................................. - 7 - 1.1.4. Typen des Pyoderma gangränosum: .................................................. - 9 - 1.1.5. Histopathologie: ................................................................................ - 12 - 1.1.6. Pathogenese: ................................................................................... -

Sexual Health Information for Gay & Bisexual
Sexual Health Information for Gay & Bisexual Men When we talk about sexual health, we often focus on HIV and other STIs, but there are a number of other illness and issues that can affect men’s sexual health. These can include erectile dysfunction (finding it difficult to get or keep an erection), testicular problems, anal pain and discomfort and other infections affecting the genital or anal area. Balanitis Balanitis is a condition where the end of the penis (or the glans) becomes inflamed, leading to redness, irritation and soreness. Men who experience this can sometimes mistake this for symptoms of an STI. Possible causes of balanitis are: a build up of yeast infection, urine, sweat or other debris under the foreskin an allergic reaction to some soaps, washing powders or cleansing products an allergic reaction to condoms phimosis – a condition where the foreskin is tight and does not pull back over the glans another sexually transmitted infection Treatments depend on the cause of balanitis, but could include: an anti-yeast cream or tablets (e.g.canesten) a steroid cream to reduce inflammation advising the use of non-latex condoms circumcision (if the man has phimosis) regular washing of the glans with water and a bland soap treatments for any STIs present Testicular Cancer This is the most common form of cancer affecting young men between the ages of 15 and 40. Men with an un- descended or partially descended testicle (one or both testicles don’t come down into the scrotum) are more likely to develop testicular cancer as do men with a family history of this cancer. -

Urinary Retention in Adults: Diagnosis and Initial Management Brian A
Urinary Retention in Adults: Diagnosis and Initial Management BRIAN a. SELIUS, DO, and rAJESH SUBEDI, MD, Northeastern Ohio Universities College of Medicine, St. Elizabeth Health Center, Youngstown, Ohio Urinary retention is the inability to voluntarily void urine. This condition can be acute or chronic. Causes of urinary retention are numerous and can be classified as obstructive, infectious and inflammatory, pharmacologic, neuro- logic, or other. The most common cause of urinary retention is benign prostatic hyperplasia. Other common causes include prostatitis, cystitis, urethritis, and vulvovaginitis; receiving medications in the anticholinergic and alpha- adrenergic agonist classes; and cortical, spinal, or peripheral nerve lesions. Obstructive causes in women often involve the pelvic organs. A thorough history, physical examination, and selected diagnostic testing should determine the cause of urinary retention in most cases. Initial management includes bladder catheterization with prompt and com- plete decompression. Men with acute urinary retention from benign prostatic hyperplasia have an increased chance of returning to normal voiding if alpha blockers are started at the time of catheter insertion. Suprapubic catheteriza- tion may be superior to urethral catheterization for short-term management and silver alloy-impregnated urethral catheters have been shown to reduce urinary tract infection. Patients with chronic urinary retention from neurogenic bladder should be able to manage their condition with clean, intermittent self-catheterization; low-friction catheters have shown benefit in these patients. Definitive management of urinary retention will depend on the etiology and may include surgical and medical treatments. (Am Fam Physician. 2008;77(5):643-650. Copyright © 2008 American Academy of Family Physicians.) rinary retention is the inabil- physician to make an accurate diagnosis ity to voluntarily urinate. -

Microhematuria and Urinary Tract Infections
1/30/2018 MICROHEMATURIA AND URINARY TRACT INFECTIONS ANEESA HUSAIN, PA-C USMD CANCER CENTER ARLINGTON - UROLOGY I HAVE NO FINANCIAL DISCLOSURES THAT WOULD BE A POTENTIAL CONFLICT OF INTEREST WITH THIS PRESENTATION. MICROHEMATURIA TOPICS OF DISCUSSION • DEFINITION • HISTORY • PHYSICAL EXAM • DIFFERENTIAL DIAGNOSES • WORK UP • TREATMENT • WHEN TO REFER? 1 1/30/2018 MICROHEMATURIA DEFINED AS.. • ≥3 RBCs per HPF (HIGH POWER FIELD) ON URINE MICROSCOPY • SHOULD NOT BASE SOLELY ON ONE DIPSTICK READING • CAN CORRELATE TO DIPSTICK URINE ANALYSIS • TRACE, SMALL, MODERATE, LARGE https://www.auanet.org/guidelines/asymptomatic-microhematuria-(2012-reviewed-and-validity-confirmed-2016) MICROHEMATURIA TOP DIFFERENTIAL DIAGNOSES • UTI/PROSTATITIS • KIDNEY STONES • URINARY TRACT OBSTRUCTION • URINARY TRACT MALIGNANCY • NEPHROLOGIC SOURCES MICROHEMATURIA HISTORY • NEW DIAGNOSIS OF MICROHEMATURIA? • PRIOR HISTORY OF GROSS OR MICROHEMATURIA? • PRIOR WORK UP • COMORBIDITIES • PELVIC RADIATION • SURGICAL HISTORY • FOR WOMEN, ASK ABOUT MENSES AND/OR MENOPAUSE • ANTICOAGULATION OR BLOOD THINNERS • SYMPTOMS 2 1/30/2018 MICROHEMATURIA HISTORY - SYMPTOMS • DYSURIA • FREQUENCY • URGENCY • DIFFICULTY VOIDING • INCONTINENCE – PAD USAGE • ABDOMINAL OR BACK PAIN • PERINEAL PAIN MICROHEMATURIA PHYSICAL EXAM • ABDOMINAL EXAM • CVA/FLANK TENDERNESS • GU EXAM • MALE – CONSIDER MEATAL STENOSIS, BALANITIS, TESTICULAR PAIN, PROSTATITIS, PROSTATE ENLARGEMENT • FEMALE – CONSIDER VAGINAL BLEEDING, YEAST INFECTION, ATROPHIC VAGINITIS MICROHEMATURIA DIFFERENTIAL DIAGNOSES • UTI/PROSTATITIS -

Guidelines on Urinary and Male Genital Tract Infections
European Association of Urology GUIDELINES ON URINARY AND MALE GENITAL TRACT INFECTIONS K.G. Naber, B. Bergman, M.C. Bishop, T.E. Bjerklund Johansen, H. Botto, B. Lobel, F. Jimenez Cruz, F.P. Selvaggi UPDATE MARCH 2004 TABLE OF CONTENTS PAGE 1 INTRODUCTION 7 1.1 Classification 7 1.2 References 8 2 UNCOMPLICATED UTIS IN ADULTS 8 2.1 Summary 8 2.2 Background 10 2.3 Definition 10 2.4 Aetiological spectrum 10 2.5 Acute uncomplicated cystitis in pre-menopausal, non-pregnant women 11 2.5.1 Diagnosis 11 2.5.2 Treatment 11 2.5.3 Post-treatment follow-up 13 2.6 Acute uncomplicated pyelonephritis in pre-menopausal, non-pregnant women 13 2.6.1 Diagnosis 13 2.6.2 Treatment 13 2.6.3 Post-treatment follow-up 14 2.7 Recurrent (uncomplicated) UTIs in women 14 2.7.1 Background 14 2.7.2 Prophylactic antimicrobial regimens 15 2.7.3 Alternative prophylactic methods 15 2.8 UTIs in pregnancy 15 2.8.1 Epidemiology 15 2.8.2 Asymptomatic bacteriuria 16 2.8.3 Acute cystitis during pregnancy 16 2.8.4 Acute pyelonephritis during pregnancy 16 2.9 UTIs in post-menopausal women 16 2.10 Acute uncomplicated UTIs in young men 17 2.10.1 Pathogenesis and risk factors 17 2.10.2 Diagnosis 17 2.10.3 Treatment 17 2.11 References 17 3 UTIs IN CHILDREN 21 3.1 Summary 21 3.2 Background 21 3.3 Aetiology 21 3.4 Pathogenesis 21 2 UPDATE MARCH 2004 3.5 Signs and symptoms 22 3.5.1 New-borns 22 3.5.2 Children < 6 months of age 22 3.5.3 Pre-school children (2-6 years of age) 22 3.5.4 School-children and adolescents 22 3.5.5 Severity of a UTI 22 3.5.6 Severe UTIs 22 3.5.7 Simple UTIs -

Reiter's Disease* by A
- REITER'S DISEASE* BY A. H. HARKNESS Joint-Director Endell Street Clinic, St. Peter's and St. Paul's Hospital (Institute of Urology); Consultant in. Venereal Diseases to- St. -Charles' Hospital; the Civil Consultant in Venereal Diseases to the Royal Navy Reiter's disease is characterized by a clinical joint. This appears to me to have been a clear syndrome consisting of a primary abacterial ure- case of the dysenteric syndrome. -Description of thritis of venereal origin, bilateral conjunctivitis, the syndrome, until the oetiology is established, polyarthritis, frequently balanitis, and sometimes would be facilitated if a distinct differentiation keratodermia blennorrhagica; cardiac and other were made between cases of venereal and those of manifestations have also been described.- The dysenteric origin. I advocated in 1947 that the, itiology is unknown. term " Reiter's disease," or better still " dysenteric There is an almost identical syndrome associated arthritis," be applied only to the latter, and that with the various types of dysentery (the primary the former-those of venereal origin-be described focus of infection in these cases is the bowel and as " non-gonococcal polyarthritis " or " the non- not the urethra) which is probably the same disease. gonococcal syndrome." Much confusion would, There are also certain other diseases and reactions I am convinced, be avoided by such a distinction. due -to treatment which may simulate the syndrome The venereal syndrome, as we know it today, very closely. was recognized many years before Reiter published In my experience true Reiter's disease is one in his case, indeed a case in which the syndrome was which the primary focus of infection is an abacterial complete was described by Launois in 1899.