Review Article
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Paraneoplastic Syndromes in Lung Cancer
Chapter 2 Paraneoplastic Syndromes in Lung Cancer Dilaver TasDilaver Tas Additional information is available at the end of the chapter http://dx.doi.org/10.5772/intechopen.79127 Abstract In recent years, the incidence of lung cancer (LC) has been increasing throughout the world and is the most common type of cancer in all regions of the world, occurring more frequently in men than in women. Paraneoplastic syndromes (PNS) refer to clinical conditions that develop in relation to tumors, without physical effects of the primary or metastatic tumors. The development of PNS is not associated with the size of the primary tumor or the extent of metastases. It is usually seen in small-cell lung cancer (SCLC) as well as other types of lung cancer. PNS developed in almost 1 in 10 patients with lung cancer and it may be an indicator for the diagnosis of lung cancer and it can be seen during later stages of cancer or at the time of cancer recurrence. Accordingly, the identification of these syndromes can be helpful in the early diagnosis of occult cancers, allowing timely treatment. PNS decreases the quality of life of the patients with cancer and thus requires specific treatment. Moreover, these conditions can be used as a marker of cancer activity and can predict prognosis. In this section, a detailed description of PNS is provided. Keywords: lung cancer, small-cell lung cancer, non-small-cell lung cancer, paraneoplastic syndromes 1. Introduction 1.1. Definition The term “paraneoplastic syndrome (PNS)” refers to tumor-related symptoms and findings that are independent of the direct, local extent or physical effects of metastases. -

Review Cutaneous Patterns Are Often the Only Clue to a a R T I C L E Complex Underlying Vascular Pathology
pp11 - 46 ABstract Review Cutaneous patterns are often the only clue to a A R T I C L E complex underlying vascular pathology. Reticulate pattern is probably one of the most important DERMATOLOGICAL dermatological signs of venous or arterial pathology involving the cutaneous microvasculature and its MANIFESTATIONS OF VENOUS presence may be the only sign of an important underlying pathology. Vascular malformations such DISEASE. PART II: Reticulate as cutis marmorata congenita telangiectasia, benign forms of livedo reticularis, and sinister conditions eruptions such as Sneddon’s syndrome can all present with a reticulate eruption. The literature dealing with this KUROSH PARSI MBBS, MSc (Med), FACP, FACD subject is confusing and full of inaccuracies. Terms Departments of Dermatology, St. Vincent’s Hospital & such as livedo reticularis, livedo racemosa, cutis Sydney Children’s Hospital, Sydney, Australia marmorata and retiform purpura have all been used to describe the same or entirely different conditions. To our knowledge, there are no published systematic reviews of reticulate eruptions in the medical Introduction literature. he reticulate pattern is probably one of the most This article is the second in a series of papers important dermatological signs that signifies the describing the dermatological manifestations of involvement of the underlying vascular networks venous disease. Given the wide scope of phlebology T and its overlap with many other specialties, this review and the cutaneous vasculature. It is seen in benign forms was divided into multiple instalments. We dedicated of livedo reticularis and in more sinister conditions such this instalment to demystifying the reticulate as Sneddon’s syndrome. There is considerable confusion pattern. -

Lesions Resembling Malignant Atrophic Papulosis in a Patient with Progressive Systemic Sclerosis
Lesions Resembling Malignant Atrophic Papulosis in a Patient With Progressive Systemic Sclerosis Clive M. Liu, MD; Ronald M. Harris, MD, MBA; C. David Hansen, MD Malignant atrophic papulosis (MAP), or Degos bleeding, and neurologic deficits. The prognosis is syndrome, is a rare disorder of unknown etiology. usually poor. Histologic characteristics include a It is characterized by a deep subcutaneous vas- vasculopathy below the necrobiotic zone with culopathy resulting in atrophic, porcelain-white endothelial swelling, proliferation, and thrombosis. papules. We report the case of a 42-year-old To our knowledge, only a few cases of MAP associ- woman with a history of progressive systemic ated with connective tissue disease have been sclerosis who presented with painful subcuta- reported: 4 cases with systemic lupus erythematosus, neous nodules on her abdomen along with 1 with dermatomyositis, and 1 with progressive sys- chronic atrophic papules on her upper and lower temic sclerosis.2-5 We present the case report of a limbs. Biopsy results of both types of lesions woman with progressive systemic sclerosis and revealed vascular thrombi without surrounding MAP-like lesions. inflammation. We briefly review the literature on MAP and its association with various connective Case Report tissue diseases. To our knowledge, there have Round erosions with dry central crusts developed on been no previous reports of a patient with the a 42-year-old woman with a long history of progres- clinical and histologic presentations described sive systemic sclerosis, significant pulmonary hyper- here. Although the histologic appearance of the tension, and right heart failure. Although the subcutaneous nodules was very similar to that of lesions were scattered on all limbs, the most promi- the atrophic papules, the clinical characteristics nent lesions extended from the right labium majus of the 2 types of lesions were strikingly different. -
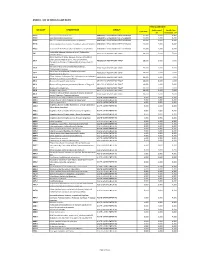
Annex 1: List of Medical Case Rates
ANNEX 1. LIST OF MEDICAL CASE RATES FIRST CASE RATE ICD CODE DESCRIPTION GROUP Professional Health Care Case Rate Fee Institution Fee P91.3 Neonatal cerebral irritability ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.4 Neonatal cerebral depression ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.6 Hypoxic ischemic encephalopathy of newborn ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.8 Other specified disturbances of cerebral status of newborn ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.9 Disturbance of cerebral status of newborn, unspecified ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 Peritonsillar abscess; Abscess of tonsil; Peritonsillar J36 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 cellulitis; Quinsy Other diseases of larynx; Abscess of larynx; Cellulitis of larynx; Disease NOS of larynx; Necrosis of larynx; J38.7 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Pachyderma of larynx; Perichondritis of larynx; Ulcer of larynx Retropharyngeal and parapharyngeal abscess; J39.0 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Peripharyngeal abscess Other abscess of pharynx; Cellulitis of pharynx; J39.1 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Nasopharyngeal abscess Other diseases of pharynx; Cyst of pharynx or nasopharynx; J39.2 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Oedema of pharynx or nasopharynx J85.1 Abscess of lung with pneumonia ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 J85.2 Abscess of lung without pneumonia; Abscess of lung NOS ABSCESS OF RESPIRATORY -

Degos-Like Lesions Associated with Systemic Lupus Erythematosus
Degos-Like Lesions Associated with SLE pISSN 1013-9087ㆍeISSN 2005-3894 Ann Dermatol Vol. 29, No. 2, 2017 https://doi.org/10.5021/ad.2017.29.2.215 CASE REPORT Degos-Like Lesions Associated with Systemic Lupus Erythematosus Min Soo Jang, Jong Bin Park, Myeong Hyeon Yang, Ji Yun Jang, Joon Hee Kim, Kang Hoon Lee, Geun Tae Kim1, Hyun Hwangbo, Kee Suck Suh Departments of Dermatology and 1Internal Medicine, Kosin University College of Medicine, Busan, Korea Degos disease, also referred to as malignant atrophic pap- 29(2) 215∼218, 2017) ulosis, was first described in 1941 by Köhlmeier and was in- dependently described by Degos in 1942. Degos disease is -Keywords- characterized by diffuse, papular skin eruptions with porce- Degos disease, Degos-like lesions, Systemic lupus eryth- lain-white centers and slightly raised erythematous te- ematosus langiectatic rims associated with bowel infarction. Although the etiology of Degos disease is unknown, autoimmune dis- eases, coagulation disorders, and vasculitis have all been INTRODUCTION considered as underlying pathogenic mechanisms. Approx- imately 15% of Degos disease have a benign course limited Degos disease is a rare systemic vaso-occlusive disorder. to the skin and no history of gastrointestinal or central nerv- Degos-like lesions associated with systemic lupus eryth- ous system (CNS) involvement. A 29-year-old female with ematosus (SLE) are a type of vasculopathy. Almost all history of systemic lupus erythematosus (SLE) presented with Degos-like lesions have the clinical pathognomonic ap- a 2-year history of asymptomatic lesions on the dorsum of all pearance of porcelain-white, atrophic papules with pe- fingers and both knees. -

Natural Remedies of Common Human Parasites and Pathogens
ACTA SCIENTIFIC MICROBIOLOGY (ISSN: 2581-3226) Volume 2 Issue 11 November 2019 Investigation Paper Natural Remedies of Common Human Parasites and Pathogens Omar M Amin* Parasitology Center, Scottsdale, Arizona *Corresponding Author: Omar M Amin, Parasitology Center, Scottsdale, Arizona. Received: July 12, 2019; Published: October 16, 2019 DOI: 10.31080/ASMI.2019.02.0401 • Bleeding. • Appetite changes. • Malabsorption. • Mucus. • Rectal itching. • Gut leakage. • Poor digestion. • Systemic/other symptoms • Fatigue. • Skin rash. • Dry cough. • Brain fog/memory loss. • Lymph blockage. Figure 1 • Allergies. • Nausea. Diagnosis and management of: • Muscle or joint pain. • Parasitic organisms and agents of medical and public • Dermatitis. health importance in fecal, blood, skin, urine specimens. • Headaches. • Toxicities related to Neurocutaneous Syndrome (NCS). • Insomnia. Development of anti-parasitic herbal products (F/C/R) Edu- How we get infected cational services: workshops, seminars, training and publications Drinking water or juice: Giardia, Cryptosporidium. provided. 1. 2. Skin contact with contaminated water: Schistosomi- Consultations and protocols for herbal and allopathic treat- asis, swimmers itch. ments. Research: over 220 publications on parasites from all con- Food (fecal-oral infections): most protozoans, ex., tinents. 3. Blastocysts, Entamoeba spp. and worms: Ascaris. Why test? 4. Arthropods: Lyme disease, plague, typhus, etc. You need to be tested if you have one or more of these symp- 5. Air: Upper respiratory tract infections (viruses, bac- toms: teria), ex GI symptoms 6. Pets: Hydatid., flu, Valleycyst disease,fever, Hanta heart virus. worm, larva mi- grans (dogs), Toxoplasma (cats), Taenia (beef, swine. • Diarrhea/constipation. People (contagious diseases): AIDS, herpes. • Irritable bowel 7. Soil: hook worms, thread worms. • Cramps 8. -

Degos Disease Associated with Behçet's Disease
Letter to the Editor http://dx.doi.org/10.5021/ad.2015.27.2.235 Degos Disease Associated with Behçet’s Disease Young Jee Kim, Sook Jung Yun, Seung-Chul Lee, Jee-Bum Lee Department of Dermatology, Chonnam National University Medical School, Gwangju, Korea Dear Editor: found as an apparent idiopathic disease or as a surrogate Degos disease (DD) is a rare, thrombo-occlusive vasculop- clinical finding in some connective tissue diseases. Here, athy that primarily affect the skin, gastrointestinal tract, we report a patient with cutaneous manifestation of DD, and central nervous system1. The cutaneous lesions pres- associated with mucocutaneous and systemic BD lesions. ent as characteristic papules with porcelain-white central A 45-year-old woman had asymptomatic erythematous atrophy and an erythematous raised border. Behçet’s dis- papules with central, porcelain-white colored umbilication ease (BD) is a systemic vasculitis characterized clinically on the trunk and both extremities for 20 years, and some by recurrent oral aphthous and genital ulcers, cutaneous of the lesions had healed to leave atrophic scars (Fig. 1A, lesions, and iridocyclitis/posterior uveitis2. DD can be B). She also had recurrent oral and genital ulcers for 20 Fig. 1. (A, B) Erythematous to brownish papules with porcelain- white central atrophy. (C) Recurrent oral aphthous ulcer. Received March 13, 2014, Revised May 14, 2014, Accepted for publication June 23, 2014 Corresponding author: Jee-Bum Lee, Department of Dermatology, Chonnam National University Hospital, 42 Jebong-ro, Dong-gu, Gwangju 501-757, Korea. Tel: 82-62-220-6684, Fax: 82-62-222-4058, E-mail: [email protected] This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http:// creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, pro- vided the original work is properly cited. -

Paraneoplastic Syndromes in Lung Cancer and Their Management
359 Review Article Page 1 of 9 Paraneoplastic syndromes in lung cancer and their management Asad Anwar1, Firas Jafri1, Sara Ashraf2, Mohammad Ali S. Jafri3, Michael Fanucchi3 1Department of Internal Medicine, Westchester Medical Center, Valhalla, NY, USA; 2Department of Hematology/Oncology, Marshall University, Huntington, WV, USA; 3Department of Hematology/Oncology, Westchester Medical Center, Valhalla, NY, USA Contributions: (I) Conception and design: All authors; (II) Administrative support: None; (III) Provision of study materials or patients: None; (IV) Collection and assembly of data: None; (V) Data analysis and interpretation: None; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Mohammad Ali S. Jafri, MD. Department of Hematology/Oncology, Westchester Medical Center, Valhalla, NY, USA. Email: [email protected]. Abstract: Paraneoplastic syndromes are most frequently associated with lung cancer. This review considers a variety paraneoplastic syndromes associated with lung cancer and discusses their pathophysiology, clinical features and management options. Keywords: Paraneoplastic syndromes; lung cancer; thoracic oncology Submitted Feb 12, 2019. Accepted for publication Apr 25, 2019. doi: 10.21037/atm.2019.04.86 View this article at: http://dx.doi.org/10.21037/atm.2019.04.86 Introduction PTHrP production (parathyroid hormone related-protein), it is referred to as HHM. Paraneoplastic syndromes refer to the remote effects HHM is observed in a variety of malignancies such as associated with malignancy which are unrelated to direct breast, renal, multiple myeloma and lung; squamous cell tumor invasion or metastases (1). These may occur before is the most frequently observed subtype (3-5). Osteolytic the cancer is diagnosed and can be independent in their metastases are another significant cause of hypercalcemia in severity to the stage of the primary tumor. -

A ABCD, 19, 142, 152 ABCDE, 19, 142 Abramowitz Sign, 3, 5
Index A Atopic dermatitis, 2, 18, 19, 20, 30, ABCD, 19, 142, 152 61, 81, 82, 84, 86, 99 ABCDE, 19, 142 Atrophie blanche, 173, 177 Abramowitz sign, 3, 5 Atrophy, crinkling, 143, 160 Acanthosis nigricans, 105, 106, 132 Atypical nevus, 144, 145, 163, 164 Addison disease (primary adrenal eclipse, 144, 164 insufficiency), 137 ugly duckling, 144, 163 Albright (McCune–Albright Auspitz sign, 3, 5, 6, 18, 104 syndrome), 83, 93 All in different stages, 33, 34, 40 All in same stage, 33, 34, 38 B Alopecia, 57, 77, 94, 105, 106, 111, Bamboo hair, 84, 99, 171, 172 117, 119, 127, 133, 171, 172, Basal cell carcinoma, 17, 104, 140, 182, 184 151, 162, 170 Alopecia areata, 105, 106, 127, 171 Bioterrorism, 33, 38 Amyloid, 107, 119 Black dot (tinea capitis), 37, 57 Angiofibroma, 89 Blue angel (see Tumors, painful) Angiokeratoma, 3, 79, 81, 85 Blue rubber bleb nevus, 144, Angiolipoma, 142, 155 154, 168 Angioma, spider, 107, 109, 134 angiolipioma, 142, 155 Angiomatosis, leptomeningeal, 90 neurilemmoma, 142, 156 Anticoagulant, lupus, 108, 121 glomus tumor, 142, 157 Antiphospholipid syndrome eccrine spiradenoma, 142, 158 (APLS), 19, 107, 108, 121 leiomyoma, 142, 159 Apocrine hidrocystoma, 144, Blue cyst (apocrine hidrocystoma), 166, 168 144, 166, 168 Apple jelly, 36, 37, 47 Blue nose (purpura fulminans), 19, Ash leaf macule (confetti macule), 108, 122 82, 89 Blue papule (blue nevus), 1, 144, Asymmetry, 19, 118, 136, 152 166, 167, 168 187 188 Index Blue rubber bleb nevus, 144, 154, 168 Coast of California, 82, 83, 91 Border Coast of Maine, 83, 93 irregular, 83, -

Cutaneous Balamuthia Mandrillaris Infection As a Precursor To
Volume 23 Number 7 | July 2017 Dermatology Online Journal || Case Report DOJ 23 (7): 4 Cutaneous Balamuthia mandrillaris infection as a precursor to Balamuthia amoebic encephalitis (BAE) in a healthy 84-year-old Californian Larisa M Lehmer, Gabriel E Ulibarri, Bruce D Ragsdale, James Kunkle Affiliations: University of California Irvine Health, Department of Dermatology, Irvine, California, Central Coast Pathology Laboratory, San Luis Obispo, California, Western Diagnostic Services Laboratory, San Luis Obispo, California, Central Coast Dermatology, Arroyo Grande, California Corresponding Author: Larisa M Lehmer, Department of Dermatology, UC Irvine Health, 118 Med Surg 1, Irvine, CA 92697-2400, Email: [email protected] Abstract Keywords: Balamuthia mandrillaris; cutaneous balamuthiasis; granulomatous amoebic encephalitis; Soil and freshwater-dwelling amoebae may GAE; balamuthia amoebic encephalitis; BAE; opportunistically infect the skin and evoke a immunocompromise; granulomatous dermatitis; granulomatous dermatitis that camouflages their immune senescence. underlying morphology. Amoebic infestations are incredibly rare in the U.S., predominantly occurring in the young, elderly, and immunocompromised. Introduction Sadly, because diagnosis is difficult and unsuspected, Balamuthia mandrillaris (B. mandrillaris), along most cases are diagnosed at autopsy. The following with Naegleria, Sappinia and several species of case is of a healthy 84-year-old man with a non- Acanthomeba, are free-living amoebae found in fresh healing nodulo-ulcerative cutaneous lesion on his water and soil worldwide that may opportunistically left forearm that appeared following a gardening infect the skin and/or central nervous system (CNS) injury. Lesional punch biopsies repeatedly showed of humans. The first sign of infection ranges from non-specific granulomatous inflammation with a stubborn indurated plaque or ulceration on the no pathogens evident histologically or by culture. -

Expanding Medical Advisory Board Dr. Lee Shapiro, Chief Medical
Awareness. Diagnosis. Education. Research. Our mission is to support and promote research toward treatment and cure of Scleroderma, Degos Disease, and other related disorders, to promote awareness and understanding of these disorders, especially among health-care professionals, and to encourage collaborative efforts, nationally and internationally, aimed at realizing these goals. Expanding Medical Advisory Board Dr. Lee Shapiro, Chief Medical Thank you to all who attended our Officer of the Steffens Foundation, has forged strong Cruise for a Real Cure! collaborative relationships with Scleroderma and Degos More than 100 people took a ride along Disease experts nationally and internationally. He the Hudson River on the Dutch Apple to recently invited 3 physicians and a medical ethicist, who raise awareness and funding for are prestigious experts in their fields, to join Steffens as Scleroderma and Degos Disease members of the medical advisory board for the research and education. foundation. They all graciously agreed to join Steffens in our mission. It is with great pleasure, we introduce Dr. Lesley Saketkoo, Dr. Leslie Frech, Dr. Patrick Whelan, and Stephen Veit, medical ethicist. Dr. Lesley A Saketkoo, MD, MPH, is a researcher, educator and clinician in scleroderma/systemic sclerosis, sarcoidosis, myositis, pulmonary hypertension and interstitial lung disease. In 2011, she established the Scleroderma and Sarcoidosis Patient Care and Research Center between Tulane and Louisiana State University, “center of excellence” by the European Scleroderma Trials and Research Group (EUSTAR), the Thank you to all who donated to make Scleroderma Foundation, and the Scleroderma Clinical Trials Consortium (SCTC).; the event a success! and also established the Pulmonary Hypertension clinic program at LSU, which is Dutch Apple Cruises & Tours now the LSU-Tulane collaborative Comprehensive Pulmonary Hypertension Center DeMarco’s Italian-American Restaurant (CPHC) at University Medical Center, a Pulmonary Hypertension Association Ellms Family Farms certified center of excellence. -

Die Prinzipien Der Chirurgischen Therapie Beim Fortgeschrittenen
Aus der Chirurgischen Klinik und Poliklinik - Innenstadt, der Ludwig-Maximilian- Universität-München Direktor: Prof. Dr. med. Wolf Mutschler Die Prinzipien der chirurgischen Therapie beim fortgeschrittenen Pyoderma gangränosum Dissertation zum Erwerb des Doktorgrades der Medizin an der Medizinischen Fakultät der Ludwig-Maximilians-Universität zu München vorgelegt von Christoph Hendrik Volkering aus Groß-Gerau 2008 Mit Genehmigung der Medizinischen Fakultät der Universität München Berichterstatter: Prof. Dr. Sigurd Keßler Mitberichterstatter: Prof. Dr. Hans C. Korting Priv. Doz. Dr. Martin K. Angele Dekan: Prof. Dr. med. Dr. h.c. Maximilian Reiser, FACR Tag der mündlichen Prüfung: 20.11.2008 - 2 - INHALT 1. Einleitung: ........................................................................................................... - 6 - 1.1. Das Pyoderma gangränosum: ..................................................................... - 6 - 1.1.1. Geschichte: ......................................................................................... - 6 - 1.1.2. Inzidenz: ............................................................................................. - 6 - 1.1.3. Assoziierte Erkrankungen: .................................................................. - 7 - 1.1.4. Typen des Pyoderma gangränosum: .................................................. - 9 - 1.1.5. Histopathologie: ................................................................................ - 12 - 1.1.6. Pathogenese: ...................................................................................