Pamelor Label
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Table 2. 2012 AGS Beers Criteria for Potentially
Table 2. 2012 AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults Strength of Organ System/ Recommendat Quality of Recomm Therapeutic Category/Drug(s) Rationale ion Evidence endation References Anticholinergics (excludes TCAs) First-generation antihistamines Highly anticholinergic; Avoid Hydroxyzin Strong Agostini 2001 (as single agent or as part of clearance reduced with e and Boustani 2007 combination products) advanced age, and promethazi Guaiana 2010 Brompheniramine tolerance develops ne: high; Han 2001 Carbinoxamine when used as hypnotic; All others: Rudolph 2008 Chlorpheniramine increased risk of moderate Clemastine confusion, dry mouth, Cyproheptadine constipation, and other Dexbrompheniramine anticholinergic Dexchlorpheniramine effects/toxicity. Diphenhydramine (oral) Doxylamine Use of diphenhydramine in Hydroxyzine special situations such Promethazine as acute treatment of Triprolidine severe allergic reaction may be appropriate. Antiparkinson agents Not recommended for Avoid Moderate Strong Rudolph 2008 Benztropine (oral) prevention of Trihexyphenidyl extrapyramidal symptoms with antipsychotics; more effective agents available for treatment of Parkinson disease. Antispasmodics Highly anticholinergic, Avoid Moderate Strong Lechevallier- Belladonna alkaloids uncertain except in Michel 2005 Clidinium-chlordiazepoxide effectiveness. short-term Rudolph 2008 Dicyclomine palliative Hyoscyamine care to Propantheline decrease Scopolamine oral secretions. Antithrombotics Dipyridamole, oral short-acting* May -
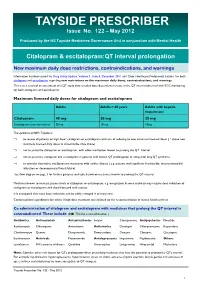
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -

PRODUCT MONOGRAPH ELAVIL® Amitriptyline Hydrochloride Tablets
PRODUCT MONOGRAPH ELAVIL® amitriptyline hydrochloride tablets USP 10, 25, 50 and 75 mg Antidepressant AA PHARMA INC. DATE OF PREPARATION: 1165 Creditstone Road Unit #1 August 29, 2018 Vaughan, ON L4K 4N7 Control No.: 217626 1 PRODUCT MONOGRAPH ELAVIL® amitriptyline hydrochloride tablets USP 10, 25, 50, 75 mg THERAPEUTIC CLASSIFICATION Antidepressant ACTIONS AND CLINICAL PHARMACOLOGY Amitriptyline hydrochloride is a tricyclic antidepressant with sedative properties. Its mechanism of action in man is not known. Amitriptyline inhibits the membrane pump mechanism responsible for the re-uptake of transmitter amines, such as norepinephrine and serotonin, thereby increasing their concentration at the synaptic clefts of the brain. Amitriptyline has pronounced anticholinergic properties and produces EKG changes and quinidine-like effects on the heart (See ADVERSE REACTIONS). It also lowers the convulsive threshold and causes alterations in EEG and sleep patterns. Orally administered amitriptyline is readily absorbed and rapidly metabolized. Steady-state plasma concentrations vary widely and this variation may be genetically determined. Amitriptyline is primarily excreted in the urine, mostly in the form of metabolites, with some excretion also occurring in the feces. INDICATIONS AND CLINICAL USE ELAVIL® (amitriptyline hydrochloride) is indicated in the drug management of depressive illness. ELAVIL® may be used in depressive illness of psychotic or endogenous nature and in selected patients with neurotic depression. Endogenous depression is more likely to be alleviated than are other depressive states. ELAVIL® ®, because of its sedative action, is also of value in alleviating the anxiety component of depression. As with other tricyclic antidepressants, ELAVIL® may precipitate hypomanic episodes in patients with bipolar depression. These drugs are not indicated in mild depressive states and depressive reactions. -

COPD Agents Review – October 2020 Page 2 | Proprietary Information
COPD Agents Therapeutic Class Review (TCR) October 1, 2020 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. October 2020 -

Management of Major Depressive Disorder Clinical Practice Guidelines May 2014
Federal Bureau of Prisons Management of Major Depressive Disorder Clinical Practice Guidelines May 2014 Table of Contents 1. Purpose ............................................................................................................................................. 1 2. Introduction ...................................................................................................................................... 1 Natural History ................................................................................................................................. 2 Special Considerations ...................................................................................................................... 2 3. Screening ........................................................................................................................................... 3 Screening Questions .......................................................................................................................... 3 Further Screening Methods................................................................................................................ 4 4. Diagnosis ........................................................................................................................................... 4 Depression: Three Levels of Severity ............................................................................................... 4 Clinical Interview and Documentation of Risk Assessment............................................................... -

PERPHENAZINE and AMITRIPTYLINE HYDROCHLORIDE- Perphenazine and Amitriptyline Hydrochloride Tablet, Film Coated Mylan Pharmaceuticals Inc
PERPHENAZINE AND AMITRIPTYLINE HYDROCHLORIDE- perphenazine and amitriptyline hydrochloride tablet, film coated Mylan Pharmaceuticals Inc. ---------- WARNING Increased Mortality in Elderly Patients with Dementia-Related Psychosis Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug- treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. Perphenazine and amitriptyline hydrochloride is not approved for the treatment of patients with dementia- related psychosis (see WARNINGS). Suicidality and Antidepressant Drugs Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of perphenazine and amitriptyline or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. -

Tactile Stimulation on Adulthood Modifies the HPA Axis, Neurotrophic Factors, and GFAP Signaling Reverting Depression-Like Behavior in Female Rats
Molecular Neurobiology (2019) 56:6239–6250 https://doi.org/10.1007/s12035-019-1522-5 Tactile Stimulation on Adulthood Modifies the HPA Axis, Neurotrophic Factors, and GFAP Signaling Reverting Depression-Like Behavior in Female Rats Kr. Roversi1 & Caren Tatiane de David Antoniazzi1 & L. H. Milanesi1 & H. Z. Rosa1 & M. Kronbauer1 & D. R. Rossato2 & T. Duarte1 & M. M. Duarte3 & Marilise E. Burger1 Received: 9 October 2018 /Accepted: 30 January 2019 /Published online: 11 February 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Depression is a common psychiatric disease which pharmacological treatment relieves symptoms, but still far from ideal. Tactile stimulation (TS) has shown beneficial influences in neuropsychiatric disorders, but the mechanism of action is not clear. Here, we evaluated the TS influence when applied on adult female rats previously exposed to a reserpine-induced depression-like animal model. Immediately after reserpine model (1 mg/kg/mL, 1×/day, for 3 days), female Wistar rats were submitted to TS (15 min, 3×/day, for 8 days) or not (unhandled). Imipramine (10 mg/kg/mL) was used as positive control. After behavioral assessments, animals were euthanized to collect plasma and prefrontal cortex (PFC). Behavioral observations in the forced swimming test, splash test, and sucrose preference confirmed the reserpine-induced depression-like behavior, which was reversed by TS. Our findings showed that reserpine increased plasma levels of adrenocorticotropic hormone and corticosterone, decreased brain- derived neurotrophic factor (BDNF) and tropomyosin receptor kinase B, and increased proBDNF immunoreactivity in the PFC, which were also reversed by TS. Moreover, TS reestablished glial fibrillary acidic protein and glucocorticoid receptor levels, decreased by reserpine in PFC, while glial cell line–derived neurotrophic factor was increased by TS per se. -

Nuedexta) National Drug Monograph May 2013 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives
Dextromethorphan/ Quinidine Monograph Dextromethorphan Hydrobromide and Quinidine Sulfate (Nuedexta) National Drug Monograph May 2013 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a comprehensive drug review for making formulary decisions. These documents will be updated when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. Executive Summary: Current therapy for pseudobulbar affect (PBA) typically utilizes non-pharmacologic coping strategies such as relaxation and distraction techniques. The off-label use of selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs) and dopaminergic agents has found limited success in treating PBA exacerbations. Dextromethorphan/quinidine (Nuedexta) is a combination of two existing generic formulary options; however quinidine is not available in an appropriate strength or in a liquid formulation (200mg, 300mg capsules only). Low dose quinidine inhibits the rapid metabolism of dextromethorphan, therefore increasing the bioavailability of dextromethorphan, resulting in effective plasma levels. In a double-blind, placebo-controlled study, the combination of dextromethorphan (20 or 30 mg) and low dose quinidine (10 mg) [STAR trial] significantly reduced the frequency of pseudobulbar affect episodes vs. placebo over the course of 12 weeks of treatment (p < 0.0001). Patients in the dextromethorphan/quinidine 20 mg/10 mg group reported a mean weekly episode reduction of 82% from baseline vs. a reduction of 47% in the placebo group (p = 0.001). Mean Center for Neurological Study-Lability Scale (CNS-LS) scores decreased by 8.2 points for both dextromethorphan/quinidine dosage groups vs. -

Determination of Salivary Efavirenz by Liquid Chromatography Coupled with Tandem Mass Spectrometry
G Model CHROMB-17040; No. of Pages 5 ARTICLE IN PRESS Journal of Chromatography B, xxx (2010) xxx–xxx Contents lists available at ScienceDirect Journal of Chromatography B journal homepage: www.elsevier.com/locate/chromb Determination of salivary efavirenz by liquid chromatography coupled with tandem mass spectrometry Anri Theron a, Duncan Cromarty b, Malie Rheeders a, Michelle Viljoen a,∗ a Pharmacology, School of Pharmacy & Unit for Drug Research and Development North-West University, Private Bag X6001, Building G16, Room 113, Potchefstroom 2520, South Africa b Department of Pharmacology, Medical School, University of Pretoria, PO Box 2034, Pretoria 0001, South Africa article info abstract Article history: A novel and robust screening method for the determination of the non-nucleoside reverse transcriptase Received 12 May 2010 inhibitor, efavirenz (EFV), in human saliva has been developed and validated based on high perfor- Accepted 31 August 2010 mance liquid chromatography tandem mass spectrometry (LC–MS/MS). Sample preparation of the saliva Available online xxx involved solid-phase extraction (SPE) on C18 cartridges. The analytes were separated by high perfor- mance liquid chromatography (Phenomenex Kinetex C18, 150 mm × 3 mm internal diameter, 2.6 m Keywords: particle size) and detected with tandem mass spectrometry in electrospray positive ionization mode Efavirenz with multiple reaction monitoring. Gradient elution with increasing methanol (MeOH) concentration Saliva LC–MS/MS was used to elute the analytes, at a flow-rate of 0.4 mL/min. The total run time was 8.4 min and the retention times for the internal standard (reserpine) was 5.4 min and for EFV was 6.5 min. -

Trimbow, INN-Beclometasone Dipropionate, Formoterol Fumarate
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Trimbow 87 micrograms/5 micrograms/9 micrograms pressurised inhalation, solution 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each delivered dose (the dose leaving the mouthpiece) contains 87 micrograms of beclometasone dipropionate, 5 micrograms of formoterol fumarate dihydrate and 9 micrograms of glycopyrronium (as 11 micrograms glycopyrronium bromide). Each metered dose (the dose leaving the valve) contains 100 micrograms of beclometasone dipropionate, 6 micrograms of formoterol fumarate dihydrate and 10 micrograms of glycopyrronium (as 12.5 micrograms glycopyrronium bromide). Excipient with known effect Trimbow contains 8.856 mg ethanol per actuation. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Pressurised inhalation, solution (pressurised inhalation). Colourless to yellowish liquid solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications COPD Maintenance treatment in adult patients with moderate to severe chronic obstructive pulmonary disease (COPD) who are not adequately treated by a combination of an inhaled corticosteroid and a long-acting beta2-agonist or a combination of a long-acting beta2-agonist and a long-acting muscarinic antagonist (for effects on symptoms control and prevention of exacerbations see section 5.1). Asthma Maintenance treatment of asthma, in adults not adequately controlled with a maintenance combination of a long-acting beta2-agonist and medium dose of inhaled corticosteroid, and who experienced one or more asthma exacerbations in the previous year. 4.2 Posology and method of administration Posology Adults The recommended dose is two inhalations twice daily. The maximum dose is two inhalations twice daily. Patients should be advised to take Trimbow every day even when asymptomatic. -

ANTIDEPRESSANTS in USE in CLINICAL PRACTICE Mark Agius1 & Hannah Bonnici2 1Clare College, University of Cambridge, Cambridge, UK 2Hospital Pharmacy St
Psychiatria Danubina, 2017; Vol. 29, Suppl. 3, pp 667-671 Conference paper © Medicinska naklada - Zagreb, Croatia ANTIDEPRESSANTS IN USE IN CLINICAL PRACTICE Mark Agius1 & Hannah Bonnici2 1Clare College, University of Cambridge, Cambridge, UK 2Hospital Pharmacy St. James Hospital Malta, Malta SUMMARY The object of this paper, rather than producing new information, is to produce a useful vademecum for doctors prescribing antidepressants, with the information useful for their being prescribed. Antidepressants need to be seen as part of a package of treatment for the patient with depression which also includes psychological treatments and social interventions. Here the main Antidepressant groups, including the Selective Serotonin uptake inhibiters, the tricyclics and other classes are described, together with their mode of action, side effects, dosages. Usually antidepressants should be prescribed for six months to treat a patient with depression. The efficacy of anti-depressants is similar between classes, despite their different mechanisms of action. The choice is therefore based on the side-effects to be avoided. There is no one ideal drug capable of exerting its therapeutic effects without any adverse effects. Increasing knowledge of what exactly causes depression will enable researchers not only to create more effective antidepressants rationally but also to understand the limitations of existing drugs. Key words: antidepressants – depression - psychological therapies - social therapies * * * * * Introduction Monoamine oxidase (MAO) inhibitors í Non-selective Monoamine Oxidase Inhibitors Depression may be defined as a mood disorder that í Selective Monoamine Oxidase Type A inhibitors negatively and persistently affects the way a person feels, thinks and acts. Common signs include low mood, Atypical Anti-Depressants and other classes changes in appetite and sleep patterns and loss of inte- rest in activities that were once enjoyable. -

DBL™ Promethazine Hydrochloride Injection BP
DBL™ Promethazine Hydrochloride Injection BP 1. NAME OF THE MEDICINE Promethazine hydrochloride 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each mL of the solution contains 25.0 mg promethazine hydrochloride, 0.10 mg disodium edetate, 1.30 microlitre glacial acetic acid, 27.2 mg sodium acetate and 1.32 mg sodium metabisulfite in water for injections. Excipient(s) with known effect Sodium metabisulfite For the full list of excipients, see section 6.1 List of Excipients. 3. PHARMACEUTICAL FORM Solution for injection. DBL™ Promethazine Hydrochloride Injection BP is a clear, colourless solution of pH 5.0 to 6.0. 4. CLINICAL PARTICULARS 4.1 Therapeutic Indications DBL™ Promethazine Hydrochloride Injection BP is indicated for the following conditions: Treatment of allergic reactions such as: uncomplicated allergic conditions of the immediate type, e.g., pruritus, urticaria and angioedema, when oral therapy is impossible or contraindicated. Treatment and prevention of vomiting including: motion sickness; drug induced nausea; prevention and control of nausea and vomiting associated with certain types of anaesthesia and surgery, such as procedures with a high incidence of post-operative vomiting (e.g., gynaecological surgery, strabismus or middle ear surgery, and electroconvulsive therapy); in patients with a past history of motion sickness or post- operative vomiting; and in patients in whom avoidance of vomiting is crucial (e.g., neurosurgery and eye surgery). Page 1 of 10 Promethazine has sedative effects and it is also used in: pre-operative, post-operative and obstetric (during labour) sedation. 4.2 Dose and Method of Administration Dosage Allergic conditions Adults: 25 mg to 50 mg by deep intramuscular injection or slow intravenous injection; may be repeated within two hours if necessary.