Contents Arteriosclerosis Atherosclerosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Documentationand Coding Tips: Peripheral Vascular Disease
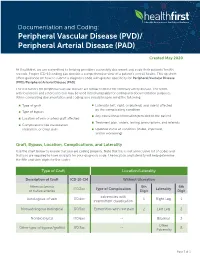
Documentation and Coding: Peripheral Vascular Disease (PVD)/ Peripheral Arterial Disease (PAD) Created May 2020 At Healthfirst, we are committed to helping providers accurately document and code their patients’ health records. Proper ICD-10 coding can provide a comprehensive view of a patient’s overall health. This tip sheet offers guidance on how to submit a diagnosis code with greater specificity for Peripheral Vascular Disease (PVD)/Peripheral Arterial Disease (PAD). The risk factors for peripheral vascular disease are similar to those for coronary artery disease. The terms arteriosclerosis and atherosclerosis may be used interchangeably for coding and documentation purposes. When completing documentation and coding, you should keep in mind the following: Type of graft Laterality (left, right, or bilateral) and side(s) affected by the complicating condition Type of bypass Any educational information provided to the patient Location of vein or artery graft affected Treatment plan, orders, testing, prescriptions, and referrals Complications like claudication, ulceration, or chest pain Updated status of condition (stable, improved, and/or worsening) Graft, Bypass, Location, Complications, and Laterality Use the chart below to ensure that you are coding properly. Note that this is not an inclusive list of codes and that you are required to have six digits for your diagnosis code. The location and laterality will help determine the fifth and sixth digits for the codes. Type of Graft Location/Laterality Description of Graft ICD-10-CM Without -
Known Infectious Causes of Vasculitis in Man
PATHOGENESIS Known infectious causes of vasculitis in man STANLEY J. NAIDES, MD n array of pathogens is known to cause vasculi- and our ability to intervene in disease processes, have ren- tis in man.1,2 For several of these agents, vas- dered some causes of vasculitis far less common. culitis is the major manifestation of disease. The Amajority, however, typically present as infec- ■ VIRAL CAUSES OF VASCULITIS tious processes in which vasculitis is an occasional mani- Our knowledge of viral pathogenesis has exploded in the festation of disease. For many, vasculitis may be a compo- last quarter of the twentieth century, accelerated in large nent of disease pathogenesis but is not a prominent feature part by epidemics of “emerging” viral diseases. Hepatitis C of the clinical presentation. The various agents—viruses, virus, discovered in 1989, has worldwide prevalence.3 The bacteria, and fungi—share a common target, blood vessels. 10- to 20-year latent period before hepatic or rheumatic The involvement of vessels may be direct, with vascular manifestations of disease explains the increasing number structures serving as targets. Many infectious pathogens of cases of hepatitis C virus–mediated vasculitis currently have tissue tropism that includes endothelium. Other being seen in the United States following the epidemic of agents may bind to the vessel wall because the vascular en- new infections in the 1980s.4 Prior to the discovery and dothelium expresses specific receptors for the pathogen or characterization of hepatitis C virus in the late 1980s, the another moiety with which the pathogen travels. Even triad of arthritis, palpable purpura, and type II cryoglobu- when the agent does not enter the endothelial cell, the im- linemia was given the sobriquet “essential mixed cryo- mune response to the agent may be focused at the vessel globulinemia” and considered an idiopathic vasculitis. -

Identification of Microorganisms Using Nucleic Acid Probes
Identification of Microorganisms Using Page 1 of 45 Nucleic Acid Probes Medical Policy An Independent Licensee of the Blue Cross and Blue Shield Association Title: Identification of Microorganisms Using Nucleic Acid Probes See Also: Influenza Virus Diagnostic Testing and Treatment in the Outpatient Setting Professional Institutional Original Effective Date: July 8, 2008 Original Effective Date: July 16, 2009 Revision Date(s): June 16, 2009; Revision Date(s): March 1, 2012; March 1, 2012; June 5, 2012; June 5, 2012; November 19, 2012; November 19, 2012; January 15, 2013; January 15, 2013; November 12, 2013 November 12, 2013 Current Effective Date: November 12, 2013 Current Effective Date: November 12, 2013 State and Federal mandates and health plan member contract language, including specific provisions/exclusions, take precedence over Medical Policy and must be considered first in determining eligibility for coverage. To verify a member's benefits, contact Blue Cross and Blue Shield of Kansas Customer Service. The BCBSKS Medical Policies contained herein are for informational purposes and apply only to members who have health insurance through BCBSKS or who are covered by a self-insured group plan administered by BCBSKS. Medical Policy for FEP members is subject to FEP medical policy which may differ from BCBSKS Medical Policy. The medical policies do not constitute medical advice or medical care. Treating health care providers are independent contractors and are neither employees nor agents of Blue Cross and Blue Shield of Kansas and are solely responsible for diagnosis, treatment and medical advice. If your patient is covered under a different Blue Cross and Blue Shield plan, please refer to the Medical Policies of that plan. -

Syphilis As Seen by a Hospital Physician
284 Prof. Monro?Syphilis as seen by a Hospital Physician. SYPHILIS AS SEEN BY A HOSPITAL PHYSICIAN* By T. K. MONRO, M.A., M.D., Professor of Medicine, University of Glasgow. \ " / Mr. President and Gentlemen,?I thank you heartily for the honour you have done me in inviting me to be Honorary President of this Faculty for the session which is now opening. I was duly informed by Dr. Wardlaw that my principal duty as incumbent of this honourable office was to deliver an address to the Faculty, and as his invitation reached me while I was on holiday, with other objects in view, I had time to contemplate the responsibility I had undertaken, and to consider how I was to face it. In getting over the usual initial difficulty as to the choice of a subject, some assistance was afforded me by the President's instruction that the address ought to be one for the general practitioner. Quite a number of subjects would be appropriate from this point of view. I should have been glad to say some- thing on oral sepsis, a condition often spoken of, and no doubt often wrongly blamed, but also apt to be overlooked. Dentists do not always realise how completely one may be misled by the absence of subjective and objective evidence; so that even an experienced man may pass as innocuous a tooth which subse- quent extraction shows to have disease at its root. Medical men sometimes make a mistake in the opposite direction, by insisting, without sufficient justification, on the removal of teeth, e.g., in epileptiform neuralgia. -

Review Cutaneous Patterns Are Often the Only Clue to a a R T I C L E Complex Underlying Vascular Pathology
pp11 - 46 ABstract Review Cutaneous patterns are often the only clue to a A R T I C L E complex underlying vascular pathology. Reticulate pattern is probably one of the most important DERMATOLOGICAL dermatological signs of venous or arterial pathology involving the cutaneous microvasculature and its MANIFESTATIONS OF VENOUS presence may be the only sign of an important underlying pathology. Vascular malformations such DISEASE. PART II: Reticulate as cutis marmorata congenita telangiectasia, benign forms of livedo reticularis, and sinister conditions eruptions such as Sneddon’s syndrome can all present with a reticulate eruption. The literature dealing with this KUROSH PARSI MBBS, MSc (Med), FACP, FACD subject is confusing and full of inaccuracies. Terms Departments of Dermatology, St. Vincent’s Hospital & such as livedo reticularis, livedo racemosa, cutis Sydney Children’s Hospital, Sydney, Australia marmorata and retiform purpura have all been used to describe the same or entirely different conditions. To our knowledge, there are no published systematic reviews of reticulate eruptions in the medical Introduction literature. he reticulate pattern is probably one of the most This article is the second in a series of papers important dermatological signs that signifies the describing the dermatological manifestations of involvement of the underlying vascular networks venous disease. Given the wide scope of phlebology T and its overlap with many other specialties, this review and the cutaneous vasculature. It is seen in benign forms was divided into multiple instalments. We dedicated of livedo reticularis and in more sinister conditions such this instalment to demystifying the reticulate as Sneddon’s syndrome. There is considerable confusion pattern. -

A Review of Primary Vasculitis Mimickers Based on the Chapel Hill Consensus Classification
Hindawi International Journal of Rheumatology Volume 2020, Article ID 8392542, 11 pages https://doi.org/10.1155/2020/8392542 Review Article A Review of Primary Vasculitis Mimickers Based on the Chapel Hill Consensus Classification Farah Zarka ,1 Charles Veillette ,1 and Jean-Paul Makhzoum 2 1Hôpital du Sacré-Cœur de Montreal, University of Montreal, Canada 2Vasculitis Clinic, Department of Internal Medicine, Hôpital du Sacré-Coeur de Montreal, University of Montreal, Canada Correspondence should be addressed to Jean-Paul Makhzoum; [email protected] Received 10 July 2019; Accepted 7 January 2020; Published 18 February 2020 Academic Editor: Charles J. Malemud Copyright © 2020 Farah Zarka et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Primary systemic vasculitides are rare diseases that may manifest similarly to more commonly encountered conditions. Depending on the size of the vessel affected (large vessel, medium vessel, or small vessel), different vasculitis mimics must be considered. Establishing the right diagnosis of a vasculitis mimic will prevent unnecessary immunosuppressive therapy. 1. Introduction 2. Large-Vessel Vasculitis Mimics Vasculitides are rare heterogenous diseases that affect vessel Large-vessel vasculitis (LVV) is an inflammatory vascu- walls as the main site of inflammation. Organs affected vary lopathy affecting large arteries; giant cell arteritis (GCA) depending on the type and size of blood vessels involved and Takayasu’s arteritis (TAK) are the two main docu- [1]. Autoimmune vasculitis can be primary (idiopathic) or mented variants, each with their own characteristic fea- secondary to an underlying disease. -
List of Codes Used to Identify Measures Reported in the QDFC
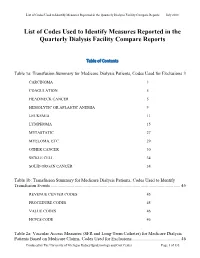
List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports Table of Contents Table 1a: Transfusion Summary for Medicare Dialysis Patients, Codes Used for Exclusions 3 CARCINOMA 3 COAGULATION 5 HEAD/NECK CANCER 5 HEMOLYTIC OR APLASTIC ANEMIA 9 LEUKEMIA 11 LYMPHOMA 15 METASTATIC 27 MYELOMA, ETC. 29 OTHER CANCER 30 SICKLE CELL 34 SOLID ORGAN CANCER 34 Table 1b: Transfusion Summary for Medicare Dialysis Patients, Codes Used to Identify Transfusion Events .................................................................................................................. 45 REVENUE CENTER CODES 45 PROCEDURE CODES 45 VALUE CODES 46 HCPCS CODE 46 Table 2a: Vascular Access Measures (SFR and Long-Term Catheter) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Exclusions ........................................... 46 Produced by The University of Michigan Kidney Epidemiology and Cost Center Page 1 of 135 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 COMA 46 END STAGE LIVER DISEASE 48 METASTATIC CANCER 48 Table 2b: Standardized Fistulae Rate (SFR) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Prevalent Comorbidities Adjusted in Model .................................... 50 ANEMIA 50 CORONARY ARTERY DISEASE 52 CONGESTIVE HEART FAILURE 55 CEREBROVASCULAR DISEASE 56 CHRONIC OBSTRUCTIVE PULMONARY DISEASE 68 DIABETES 69 DRUG DEPENDENCE 79 INFECTIONS (NON-VASCULAR ACCESS-RELATED): 93 PERIPHERAL VASCULAR DISEASE (INCLUDES ARTERIAL, VENOUS AND NONSPECIFIC DISEASES) 124 Table 3: Dialysis Adequacy ................................................................................................... -
Lecture 1 ― INTRODUCTION INTO MICROBIOLOGY
МИНИСТЕРСТВО ЗДРАВООХРАНЕНИЯ РЕСПУБЛИКИ БЕЛАРУСЬ УЧРЕЖДЕНИЕ ОБРАЗОВАНИЯ «ГОМЕЛЬСКИЙ ГОСУДАРСТВЕННЫЙ МЕДИЦИНСКИЙ УНИВЕРСИТЕТ» Кафедра микробиологии, вирусологии и иммунологии А. И. КОЗЛОВА, Д. В. ТАПАЛЬСКИЙ МИКРОБИОЛОГИЯ, ВИРУСОЛОГИЯ И ИММУНОЛОГИЯ Учебно-методическое пособие для студентов 2 и 3 курсов факультета по подготовке специалистов для зарубежных стран медицинских вузов MICROBIOLOGY, VIROLOGY AND IMMUNOLOGY Teaching workbook for 2 and 3 year students of the Faculty on preparation of experts for foreign countries of medical higher educational institutions Гомель ГомГМУ 2015 УДК 579+578+612.017.1(072)=111 ББК 28.4+28.3+28.073(2Англ)я73 К 59 Рецензенты: доктор медицинских наук, профессор, заведующий кафедрой клинической микробиологии Витебского государственного ордена Дружбы народов медицинского университета И. И. Генералов; кандидат медицинских наук, доцент, доцент кафедры эпидемиологии и микробиологии Белорусской медицинской академии последипломного образования О. В. Тонко Козлова, А. И. К 59 Микробиология, вирусология и иммунология: учеб.-метод. пособие для студентов 2 и 3 курсов факультета по подготовке специалистов для зарубежных стран медицинских вузов = Microbiology, virology and immunology: teaching workbook for 2 and 3 year students of the Faculty on preparation of experts for foreign countries of medical higher educa- tional institutions / А. И. Козлова, Д. В. Тапальский. — Гомель: Гом- ГМУ, 2015. — 240 с. ISBN 978-985-506-698-0 В учебно-методическом пособии представлены тезисы лекций по микробиоло- гии, вирусологии и иммунологии, рассмотрены вопросы морфологии, физиологии и генетики микроорганизмов, приведены сведения об общих механизмах функциони- рования системы иммунитета и современных иммунологических методах диагности- ки инфекционных и неинфекционных заболеваний. Приведены сведения об этиоло- гии, патогенезе, микробиологической диагностике и профилактике основных бакте- риальных и вирусных инфекционных заболеваний человека. Может быть использовано для закрепления материала, изученного в курсе микро- биологии, вирусологии, иммунологии. -

Etiology and Clinical Outcome of Budd-Chiari Syndrome and Portal Vein Thrombosis
Etiology and Clinical Outcome of Budd-Chiari Syndrome and Portal Vein Thrombosis Jildou Hoekstra ISBN: 978-90-8559-172-6 Financial support for printing of this thesis was kindly provided by the Department of Gastroenterology and Hepatology of the Erasmus University Medical Center, J.E. Jurriaanse Stichting and the Dutch Society of Hepatology (NVH). Printed by: Optima Grafische Communicatie, Rotterdam, the Netherlands Cover: photograph & design by Niels Agatz © 2010. Jildou Hoekstra, Rotterdam, the Netherlands. All rights reserved. No parts of this work may be reproduced or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior permission of the author. Etiology and Clinical Outcome of Budd-Chiari Syndrome and Portal Vein Thrombosis Etiologie en klinisch beloop van Budd-Chiari syndroom en vena portae trombose Proefschrift ter verkrijging van de graad van doctor aan de Erasmus Universiteit Rotterdam op gezag van de rector magnificus Prof.dr. H.G. Schmidt en volgens besluit van het College voor Promoties. De openbare verdediging zal plaatsvinden op vrijdag 17 december 2010 om 11:30 uur door Jildou Hoekstra geboren te Amstelveen PROMOTIECOMMISSIE Promotoren: Prof.dr. H.L.A. Janssen Prof.dr. F.W.G. Leebeek Overige leden: Prof.dr. H.J. Metselaar Prof.dr. P. Sonneveld Prof.dr. J.P.H. Drenth sin en wille kin folle tille CONTENTS Chapter 1 Introduction 9 Chapter 2 Etiologic factors underlying Budd-Chiari syndrome and portal vein 35 thrombosis: clues for site-specific thrombosis -

Association Between Multi-Site Atherosclerotic Plaques and Systemic Arteriosclerosis
Association between multi-site atherosclerotic plaques and systemic arteriosclerosis: results from the BEST study (Beijing Vascular Disease Patients Evaluation Study) huan liu Peking University Shougang Hospital https://orcid.org/0000-0001-6223-7677 Jinbo Liu Peking University Shougang Hospital Wei Huang Peking University Shougang Hospital Hongwei Zhao Peking University Shougang Hospital Na zhao Peking University Shougang Hospital Hongyu wang ( [email protected] ) Research Keywords: arteriosclerosis, atherosclerosis, atherosclerotic plaque, carotid femoral artery pulse wave velocity CF-PWV Posted Date: June 8th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-31641/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published on August 1st, 2020. See the published version at https://doi.org/10.1186/s12947-020-00212-3. Page 1/18 Abstract Background Arteriosclerosis can be reected in various aspect of the artery, including atherosclerotic plaque formation or stiffening on the arterial wall. Both arteriosclerosis and atherosclerosis are important and closely associated with cardiovascular disease (CVD). The aim of the study was to evaluate the association between systemic arteriosclerosis and multi-site atherosclerotic plaques. Methods The study was designed as an observational cross-sectional study. A total of 1178 participants (mean age 67.4 years; 52.2% male) enrolled into the observational study from 2010 to 2017. Systemic arteriosclerosis was assessed by carotid femoral artery pulse wave velocity (CF-PWV) and multi-site atherosclerotic plaques (MAP, >=2 of the below sites) were reected in the carotid or subclavian artery, abdominal aorta and lower extremities arteries using ultrasound equipment. -

10Th Anniversary of the Human Genome Project
Grand Celebration: 10th Anniversary of the Human Genome Project Volume 3 Edited by John Burn, James R. Lupski, Karen E. Nelson and Pabulo H. Rampelotto Printed Edition of the Special Issue Published in Genes www.mdpi.com/journal/genes John Burn, James R. Lupski, Karen E. Nelson and Pabulo H. Rampelotto (Eds.) Grand Celebration: 10th Anniversary of the Human Genome Project Volume 3 This book is a reprint of the special issue that appeared in the online open access journal Genes (ISSN 2073-4425) in 2014 (available at: http://www.mdpi.com/journal/genes/special_issues/Human_Genome). Guest Editors John Burn University of Newcastle UK James R. Lupski Baylor College of Medicine USA Karen E. Nelson J. Craig Venter Institute (JCVI) USA Pabulo H. Rampelotto Federal University of Rio Grande do Sul Brazil Editorial Office Publisher Assistant Editor MDPI AG Shu-Kun Lin Rongrong Leng Klybeckstrasse 64 Basel, Switzerland 1. Edition 2016 MDPI • Basel • Beijing • Wuhan ISBN 978-3-03842-123-8 complete edition (Hbk) ISBN 978-3-03842-169-6 complete edition (PDF) ISBN 978-3-03842-124-5 Volume 1 (Hbk) ISBN 978-3-03842-170-2 Volume 1 (PDF) ISBN 978-3-03842-125-2 Volume 2 (Hbk) ISBN 978-3-03842-171-9 Volume 2 (PDF) ISBN 978-3-03842-126-9 Volume 3 (Hbk) ISBN 978-3-03842-172-6 Volume 3 (PDF) © 2016 by the authors; licensee MDPI, Basel, Switzerland. All articles in this volume are Open Access distributed under the Creative Commons License (CC-BY), which allows users to download, copy and build upon published articles even for commercial purposes, as long as the author and publisher are properly credited, which ensures maximum dissemination and a wider impact of our publications. -

Prehypertension Increases the Risk for Renal Arteriosclerosis in Autopsies: the Hisayama Study
JASN Express. Published on June 20, 2007 as doi: 10.1681/ASN.2007010067 CLINICAL EPIDEMIOLOGY www.jasn.org Prehypertension Increases the Risk for Renal Arteriosclerosis in Autopsies: The Hisayama Study Toshiharu Ninomiya,* Michiaki Kubo,* Yasufumi Doi,† Koji Yonemoto,* Yumihiro Tanizaki,* Kazuhiko Tsuruya,† Katsuo Sueishi,‡ Masazumi Tsuneyoshi,§ Mitsuo Iida,† and Yutaka Kiyohara* Departments of *Environmental Medicine, †Medicine and Clinical Science, ‡Pathophysiological and Experimental Pathology, and §Anatomic Pathology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan ABSTRACT Information regarding the association between prehypertension BP level and renal arteriosclerosis is limited. In 652 consecutive population-based autopsy samples without hypertension treatment before death, the relationship between the severity of renal arteriosclerosis and BP levels classified according to the criteria of the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure was examined. The age- and gender-adjusted frequencies of renal arteriosclerosis linearly increased with elevating BP levels; both hypertensive and prehypertensive subjects had significantly higher frequencies of renal arteriosclerosis than subjects with normal BP (normal 11.9%; prehypertension 28.5%; stage 1 hypertension 32.9%; stage 2 hypertension 58.2%; all P Ͻ 0.01 versus normal). In a logistic regression model, prehypertension was significantly associated with renal arteriosclerosis after adjustment for other cardiovascular risk factors (prehyper- tension multivariate-adjusted odds ratio [mOR] 5.99 [95% confidence interval (CI) 2.20 to 15.97]; stage 1 hypertension mOR 6.99 [95% CI 2.61 to 18.72]; stage 2 hypertension mOR 22.21 [95% CI 8.35 to 59.08]). This significant association was observed for all renal arterial sizes.