Peripheral Vascular Disease Becomes Increasingly Prevalent with by the Symptom Or Complication (E.G
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Documentationand Coding Tips: Peripheral Vascular Disease
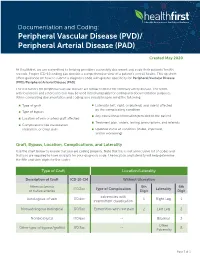
Documentation and Coding: Peripheral Vascular Disease (PVD)/ Peripheral Arterial Disease (PAD) Created May 2020 At Healthfirst, we are committed to helping providers accurately document and code their patients’ health records. Proper ICD-10 coding can provide a comprehensive view of a patient’s overall health. This tip sheet offers guidance on how to submit a diagnosis code with greater specificity for Peripheral Vascular Disease (PVD)/Peripheral Arterial Disease (PAD). The risk factors for peripheral vascular disease are similar to those for coronary artery disease. The terms arteriosclerosis and atherosclerosis may be used interchangeably for coding and documentation purposes. When completing documentation and coding, you should keep in mind the following: Type of graft Laterality (left, right, or bilateral) and side(s) affected by the complicating condition Type of bypass Any educational information provided to the patient Location of vein or artery graft affected Treatment plan, orders, testing, prescriptions, and referrals Complications like claudication, ulceration, or chest pain Updated status of condition (stable, improved, and/or worsening) Graft, Bypass, Location, Complications, and Laterality Use the chart below to ensure that you are coding properly. Note that this is not an inclusive list of codes and that you are required to have six digits for your diagnosis code. The location and laterality will help determine the fifth and sixth digits for the codes. Type of Graft Location/Laterality Description of Graft ICD-10-CM Without -

Peripheral Artery Disease (Pad)
PERIPHERAL ARTERY DISEASE (PAD) Provider’s guide to diagnose and code PAD Peripheral Artery Disease (ICD-10 code I73.9) is estimated The American Cardiology and American Heart Association to affect 12 to 20% of Americans age 65 and older with as 2013 revised guidelines recommend the following many as 75% of that group being asymptomatic (Rogers et al, interpretation for noncompression values for ABI 2011). Of note, for the purposes of this clinical flyer the term (Anderson, 2013). peripheral vascular disease (PVD) is used synonymously with PAD. Table 2: Interpretation of ABI Values Who and how to screen for PAD Value Interpretation The updated 2013 American College of Cardiology and > 1.30 Non-compressible American Heart Association guidelines for the management of 1.00 – 1.29 Normal patients with PAD, recommends screening patients at risk for lower extremity PAD (Anderson et al, 2013). 0.91 – 0.99 Borderline The guidelines recommend reviewing vascular signs and 0.41 - 0.90 Mild to moderate PAD symptoms (e.g., walking impairment, claudication, ischemic 0.00 – 0.40 Severe PAD rest pain and/or presence of non-healing wounds) and physical examination (e.g., evaluation of pulses and inspection The diagnostic accuracy of the ABI can be hindered under the of lower extremities). The Trans-Atlantic Inter-Society following conditions: (Ruff, 2003) Consensus Document on Management of PAD and U.S. Preventative Task Force on screening for PAD identify similar › Patient anxiety and/or discomfort screening criteria that address patient’s age, smoking history, › Poor positioning of patient or restless patient co-morbid conditions and physical exam findings (Moyer, 2013 & Norgren et al, 2007). -

Intracerebral Hemorrhage
Circulation Journal ORIGINAL ARTICLE Circ J 2019; 83: 441 – 446 doi: 10.1253/circj.CJ-18-0938 Stroke Safety of Anticoagulant Therapy Including Direct Oral Anticoagulants in Patients With Acute Spontaneous Intracerebral Hemorrhage Yuki Sakamoto, MD; Chikako Nito, MD, PhD; Yasuhiro Nishiyama, MD, PhD; Satoshi Suda, MD, PhD; Noriko Matsumoto, MD, PhD; Junya Aoki, MD, PhD; Takashi Shimoyama, MD, PhD; Takuya Kanamaru, MD, PhD; Kentaro Suzuki, MD; Takuya Nishimura, MD; Masahiro Mishina, MD, PhD; Kazumi Kimura, MD, PhD Background: Because the efficacy and safety of anticoagulant therapy in patients with acute intracerebral hemorrhage (ICH) are not fully known, present study aimed to elucidate the current status and the safety of anticoagulant therapy, mainly direct oral anticoagulants (DOACs), for acute ICH and anticoagulant-indicated patients. Methods and Results: From September 2014 through March 2017, consecutive patients with acute (<7 days from onset), sponta- neous ICH were retrospectively enrolled from a prospective registry. Whether to start anticoagulation was at the attending physicians’ discretion, and thromboembolic or hemorrhagic events during hospitalization were analyzed. A total of 236 patients (80 women [34%]; median age 69 [interquartile range 61–79] years; National Institutes of Health stroke scale score 7 [3–16]) were enrolled. Of them, 47 patients (20%) had an indication for anticoagulant therapy (33 had atrial fibrillation, 14 developed deep vein thrombosis), and 41 of 47 patients (87%) were actually treated with anticoagulant therapy (DOACs were used in 34 patients) after a median of 7 days from ICH onset. There was neither hematoma expansion nor excessive hemorrhagic complications during hospitalization after starting anticoagulant therapy. -

Association Between Multi-Site Atherosclerotic Plaques and Systemic Arteriosclerosis
Association between multi-site atherosclerotic plaques and systemic arteriosclerosis: results from the BEST study (Beijing Vascular Disease Patients Evaluation Study) huan liu Peking University Shougang Hospital https://orcid.org/0000-0001-6223-7677 Jinbo Liu Peking University Shougang Hospital Wei Huang Peking University Shougang Hospital Hongwei Zhao Peking University Shougang Hospital Na zhao Peking University Shougang Hospital Hongyu wang ( [email protected] ) Research Keywords: arteriosclerosis, atherosclerosis, atherosclerotic plaque, carotid femoral artery pulse wave velocity CF-PWV Posted Date: June 8th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-31641/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published on August 1st, 2020. See the published version at https://doi.org/10.1186/s12947-020-00212-3. Page 1/18 Abstract Background Arteriosclerosis can be reected in various aspect of the artery, including atherosclerotic plaque formation or stiffening on the arterial wall. Both arteriosclerosis and atherosclerosis are important and closely associated with cardiovascular disease (CVD). The aim of the study was to evaluate the association between systemic arteriosclerosis and multi-site atherosclerotic plaques. Methods The study was designed as an observational cross-sectional study. A total of 1178 participants (mean age 67.4 years; 52.2% male) enrolled into the observational study from 2010 to 2017. Systemic arteriosclerosis was assessed by carotid femoral artery pulse wave velocity (CF-PWV) and multi-site atherosclerotic plaques (MAP, >=2 of the below sites) were reected in the carotid or subclavian artery, abdominal aorta and lower extremities arteries using ultrasound equipment. -

Origin of the Microangiopathic Changes in Diabetes
ORIGIN OF THE MICROANGIOPATHIC CHANGES IN DIABETES A. H. BARNETT Birmingham SUMMARY its glycosidally linked disaccharide units. Such alterations The mechanism of development of microangiopathy is lead to abnormal packing of the peptide chains producing incompletely understood, but relates to a number of excessive leakiness of the membrane. The exact mech ultrastructural, biochemical and haemostatic processes. anisms of thickening and leakiness of basement mem These include capillary basement membrane thickening, brane and their relevance to diabetic complications are not non-enzymatic glycosylation, possibly increased free rad entirely clear, but appear to involve several biochemical ical activity, increased flux through the polyol pathway mechanisms. and haemostatic abnormalities. The central feature Non-enzymatic Glycosylation appears to be hyperglycaemia, which is causally related to the above processes and culminates in tissue ischaemia. In the presence of persistent hyperglycaemia glucose This article will briefly describe these processes and will chemically attaches to proteins non-enzymatically to form discuss possible pathogenic interactions which may lead a stable product (keto amine or Amadori product) of which to the development of the pathological lesion. glycosylated haemoglobin is the best-known example. In long-lived tissue proteins such as collagen the ketoamine Microangiopathy is a specific disorder of the small blood then undergoes a series of reactions resulting in the vessels which causes much morbidity and mortality in dia development of advanced glycosylation end products betic patients. Diabetic retinopathy is the commonest (AGE) (Fig. 1).5 AGE are resistant to degradation and con cause of blindness in the working population of the United tinue to accumulate indefinitely on long-lived proteins. -
Anti-Thrombotics in Stroke When to Start and When to Stop
Anti-Thrombotics In Stroke when to start and when to stop Ania Busza MD PhD Assistant Professor of Neurology University of Rochester School of Medicine and Dentistry No Relevent Disclosures • Research funding from NIH/NICHD (K12 award) • Materials provided for research from MC10, Inc This person was He has afib but was Outlinedischarged 1 week discharged only on ago with a subdural. aspirin – when Should they be back My patient is should I restart his on aspirin? currently on warfarin anticoagulation ? but wants to get pregnant. Is that Common questions that arise post-Stroke safe? Why is everyone The report says talking about putting “likely amyloid TIA patients on angiopathy” – what BOTH aspirin and do I do about their plavix for a few antithrombotics? weeks? Outline ? • Physiology – types of clots and the logic behind the different choices for antithrombotic therapy • Timing: When should antithrombotics be started… – after an ischemic stroke? ? ? – after a hemorrhagic stroke? • Safety: What to consider in selecting antithrombotic therapy – in pregnancy – in patients with cerebral amyloid angiopathy ? • DAPT: When is duo-antiplatelet treatment indicated? Physiology of Clots thrombosis - an obstruction of blood flow due to a localized occlusive process within one more more blood vessels. Physiology of Clots RED THROMBI WHITE THROMBI RED THROMBI • Erythrocytes + Fibrin • tend to develop in low flow situations: – dilated cardiac atria / afib – regions of ventricular hypokinesia (ventricular aneurysms, low EF, or MI) – leg/pelvic veins -

The Increasing Impact of Cerebral Amyloid Angiopathy: Essential New
JNNP Online First, published on August 26, 2017 as 10.1136/jnnp-2016-314697 Cerebrovascular disease J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp-2016-314697 on 26 August 2017. Downloaded from REVIEW The increasing impact of cerebral amyloid angiopathy: essential new insights for clinical practice Gargi Banerjee,1 Roxana Carare,2 Charlotte Cordonnier,3 Steven M Greenberg,4 Julie A Schneider,5 Eric E Smith,6 Mark van Buchem,7 Jeroen van der Grond,7 Marcel M Verbeek,8,9 David J Werring1 For numbered affiliations see ABSTRact Furthermore, CAA gained new relevance with the end of article. Cerebral amyloid angiopathy (CAA) has never been advent of anti-Aβ immunotherapies for the treat- more relevant. The last 5 years have seen a rapid ment of Alzheimer’s disease (AD), as a sizeable Correspondence to increase in publications and research in the field, with proportion of those treated went on to develop Dr David J Werring, The National Hospital for Neurology and the development of new biomarkers for the disease, imaging features of CAA-related inflammation as 5 Neurosurgery, UCL Institute thanks to advances in MRI, amyloid positron emission an unintended consequence. This, together with of Neurology, Queen Square, tomography and cerebrospinal fluid biomarker analysis. advances in our understanding of the impact of London WC1N 3BG, UK; d. The inadvertent development of CAA-like pathology CAA on cognition, in the context of ICH, ageing werring@ ucl. ac. uk in patients treated with amyloid-beta immunotherapy and AD, has broadened the clinical spectrum Received 1 March 2017 for Alzheimer’s disease has highlighted the importance of disease to which the contribution of CAA is Revised 26 April 2017 of establishing how and why CAA develops; without recognised. -

Prehypertension Increases the Risk for Renal Arteriosclerosis in Autopsies: the Hisayama Study
JASN Express. Published on June 20, 2007 as doi: 10.1681/ASN.2007010067 CLINICAL EPIDEMIOLOGY www.jasn.org Prehypertension Increases the Risk for Renal Arteriosclerosis in Autopsies: The Hisayama Study Toshiharu Ninomiya,* Michiaki Kubo,* Yasufumi Doi,† Koji Yonemoto,* Yumihiro Tanizaki,* Kazuhiko Tsuruya,† Katsuo Sueishi,‡ Masazumi Tsuneyoshi,§ Mitsuo Iida,† and Yutaka Kiyohara* Departments of *Environmental Medicine, †Medicine and Clinical Science, ‡Pathophysiological and Experimental Pathology, and §Anatomic Pathology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan ABSTRACT Information regarding the association between prehypertension BP level and renal arteriosclerosis is limited. In 652 consecutive population-based autopsy samples without hypertension treatment before death, the relationship between the severity of renal arteriosclerosis and BP levels classified according to the criteria of the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure was examined. The age- and gender-adjusted frequencies of renal arteriosclerosis linearly increased with elevating BP levels; both hypertensive and prehypertensive subjects had significantly higher frequencies of renal arteriosclerosis than subjects with normal BP (normal 11.9%; prehypertension 28.5%; stage 1 hypertension 32.9%; stage 2 hypertension 58.2%; all P Ͻ 0.01 versus normal). In a logistic regression model, prehypertension was significantly associated with renal arteriosclerosis after adjustment for other cardiovascular risk factors (prehyper- tension multivariate-adjusted odds ratio [mOR] 5.99 [95% confidence interval (CI) 2.20 to 15.97]; stage 1 hypertension mOR 6.99 [95% CI 2.61 to 18.72]; stage 2 hypertension mOR 22.21 [95% CI 8.35 to 59.08]). This significant association was observed for all renal arterial sizes. -

From Brain to Heart: Possible Role of Amyloid-Β in Ischemic Heart Disease and Ischemia-Reperfusion Injury
International Journal of Molecular Sciences Review From Brain to Heart: Possible Role of Amyloid-β in Ischemic Heart Disease and Ischemia-Reperfusion Injury Giulia Gagno 1, Federico Ferro 1, Alessandra Lucia Fluca 1, Milijana Janjusevic 1, Maddalena Rossi 1, Gianfranco Sinagra 1, Antonio Paolo Beltrami 2 , Rita Moretti 3 and Aneta Aleksova 1,* 1 Cardiothoracovascular Department, Azienda Sanitaria Universitaria Giuliano Isontina (ASUGI) and University of Trieste, 34100 Trieste, Italy; [email protected] (G.G.); ff[email protected] (F.F.); alessandrafl[email protected] (A.L.F.); [email protected] (M.J.); [email protected] (M.R.); [email protected] (G.S.) 2 Department of Medicine (DAME), University of Udine, 33100 Udine, Italy; [email protected] 3 Department of Internal Medicine and Neurology, Neurological Clinic, 34100 Trieste, Italy; [email protected] * Correspondence: [email protected] or [email protected]; Tel.: +39-340-550-7762 Received: 3 December 2020; Accepted: 14 December 2020; Published: 17 December 2020 Abstract: Ischemic heart disease (IHD) is among the leading causes of death in developed countries. Its pathological origin is traced back to coronary atherosclerosis, a lipid-driven immuno-inflammatory disease of the arteries that leads to multifocal plaque development. The primary clinical manifestation of IHD is acute myocardial infarction (AMI),) whose prognosis is ameliorated with optimal timing of revascularization. Paradoxically, myocardium re-perfusion can be detrimental because of ischemia-reperfusion injury (IRI), an oxidative-driven process that damages other organs. Amyloid-β (Aβ) plays a physiological role in the central nervous system (CNS). Alterations in its synthesis, concentration and clearance have been connected to several pathologies, such as Alzheimer’s disease (AD) and cerebral amyloid angiopathy (CAA). -

Diabetic Complications Diabetic Complications
Diabetic Complications Diabetic Complications This is a 15 minute webinar session for CNC physicians and staff CNC holds webinars monthly to address topics related to risk adjustment documentation and coding Next scheduled webinar: • December • Topic: Managing Risk & Quality CNC does not accept responsibility or liability for any adverse outcome from this training for any reason including undetected inaccuracy, opinion, and analysis that might prove erroneous or amended, or the coder/physician’s misunderstanding or misapplication of topics. Application of the information in this training does not imply or guarantee claims payment. American Diabetes Association (ADA) American Diabetes Association (ADA) • Hypoglycemia – in 2011, 282 ED visits for adults who had a first listed diagnosis of hypoglycemia and diabetes as another • Hypertension – in 2009 -2012, of adults with diabetes, 71% had uncontrolled blood pressure • Dyslipidemia – in 2009-2012, of adults with diabetes, 65% had blood LDL cholesterol ≥ 100mg • CVD Death Rates – in 2003-2006, cardiovascular disease was 1.7 times higher in patient with diabetes • Heart Attack Rates – in 2010, heart attach rates were 1.8 times higher in patients with diabetes • Stroke – in 2010, stroke rates were 1.5 times higher in patients with diabetes Diabetes Mellitus E08 E09 E10 E11 E13 • Due to • Drug or • Type 1 • Type 2 • Other underlying chemical specified disease induced Documentation must specify • Type of Diabetes • Type of Complication • Kidney • Ophthalmic • Neurologic postprocedural • Circulatory underlying underlying condition • Skin/Dermatitis/Ulcer poisoning poisoning drug due to st st • Periodontal • Hypo/Hyperglycemia Code 1 • Other Code 1 Genetic defects, defects, Genetic Diabetic Complications Glaucoma People with diabetes are 40% more likely to suffer from glaucoma than people without diabetes. -

Molina Healthcare Coding Education Peripheral Arterial Disease &
Molina Healthcare Coding Education Peripheral Arterial Disease & ABI Documentation Example: Initial Diagnosis Assessment: A 73 year old asymptomatic male with a history of smoking. ABI results 0.90, currently asymptomatic PAD. ICD-10 Code: I73.9 PAD unspecified Plan: Discussed the importance of risk factor control. Will monitor. Measurement of the ankle-brachial index (ABI) is reasonable if peripheral arterial Established Diagnosis disease (PAD), also known as peripheral Assessment: A 54 year old diabetic female vascular disease (PVD), is suspected. Although the majority of patients with PAD with stable claudication due to PVD. will not have symptoms, clinical reasons to A1C and BP are currently at goal. suspect PAD include claudication, a non- healing ulcer, skin changes including hair ICD-10 Code: E1151 Type 2 diabetes loss over the lower legs, and age >701. mellitus with diabetic peripheral ABI Interpretation: angiopathy without gangrene ≤0.90 – Abnormal and diagnostic for PAD2 Plan: Discussed the importance of risk factor control, continue anti-platelet agent. Coding Tip: Will monitor. Atherosclerotic vascular disease is a chronic, _______________________________________ progressive disease that should be referred to as current or known PAD/PVD, not history 1J Vasc Surg. 2015 Mar;61(3 Suppl):2S-41S. 2 of PAD/PVD3. Ankle Brachial Index Collaboration. Atherosclerosis. 2006 Nov;189(1):61-9. 3AAPC ICD-10-CM: The Complete Code Set, 2016. Have Questions? Contact: [email protected] The information presented herein is for informational and illustrative purposes only. It is not intended, nor is it to be used, to define a standard of care or otherwise substitute for informed medical evaluation, diagnosis and treatment which can be performed by a qualified medical professional. -

Intracranial Vertebral Artery Dissection in Wallenberg Syndrome
Intracranial Vertebral Artery Dissection in Wallenberg Syndrome T. Hosoya, N. Watanabe, K. Yamaguchi, H. Kubota, andY. Onodera PURPOSE: To assess the prevalence of vertebral artery dissection in Wallenberg syndrome. METHODS: Sixteen patients (12 men, 4 women; mean age at ictus, 51 .6 years) with symptoms of Wallenberg syndrome and an infarction demonstrated in the lateral medulla on MR were reviewed retrospectively. The study items were as follows: (a) headache as clinical signs, in particular, occipitalgia and/ or posterior neck pain at ictus; (b) MR findings, such as intramural hematoma on T1-weighted images, intimal flap on T2-weighted images, and double lumen on three-dimensional spoiled gradient-recalled acquisition in a steady state with gadopentetate dimeglumine; (c) direct angiographic findings of dissection, such as double lumen, intimal flap, and resolution of stenosis on follow-up angiography; and (d) indirect angiographic findings of dissection (such as string sign, pearl and string sign, tapered narrowing, etc). Patients were classified as definite dissection if they had reliable MR findings (ie, intramural hematoma, intimal flap, and enhancement of wall and septum) and/ or direct angiographic findings; as probable dissection if they showed both headache and suspected findings (ie, double lumen on 3-D spoiled gradient-recalled acquisition in a steady state or indirect angiographic findings) ; and as suspected dissection in those with only headache or suspected findings. RESULTS: Seven of 16 patients were classified as definite dissection, 3 as probable dissection, and 3 as suspected dissection. Four patients were considered to have bilateral vertebral artery dissection on the basis of MR findings. CONCLUSIONS: Vertebral artery dissection is an important cause of Wallenberg syndrome.