Origin of the Microangiopathic Changes in Diabetes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Documentationand Coding Tips: Peripheral Vascular Disease
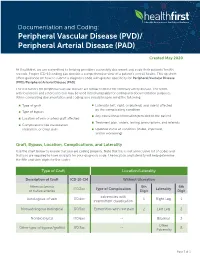
Documentation and Coding: Peripheral Vascular Disease (PVD)/ Peripheral Arterial Disease (PAD) Created May 2020 At Healthfirst, we are committed to helping providers accurately document and code their patients’ health records. Proper ICD-10 coding can provide a comprehensive view of a patient’s overall health. This tip sheet offers guidance on how to submit a diagnosis code with greater specificity for Peripheral Vascular Disease (PVD)/Peripheral Arterial Disease (PAD). The risk factors for peripheral vascular disease are similar to those for coronary artery disease. The terms arteriosclerosis and atherosclerosis may be used interchangeably for coding and documentation purposes. When completing documentation and coding, you should keep in mind the following: Type of graft Laterality (left, right, or bilateral) and side(s) affected by the complicating condition Type of bypass Any educational information provided to the patient Location of vein or artery graft affected Treatment plan, orders, testing, prescriptions, and referrals Complications like claudication, ulceration, or chest pain Updated status of condition (stable, improved, and/or worsening) Graft, Bypass, Location, Complications, and Laterality Use the chart below to ensure that you are coding properly. Note that this is not an inclusive list of codes and that you are required to have six digits for your diagnosis code. The location and laterality will help determine the fifth and sixth digits for the codes. Type of Graft Location/Laterality Description of Graft ICD-10-CM Without -

A Cross Sectional Study of Cutaneous Manifestations in 300 Patients of Diabetes Mellitus
International Journal of Advances in Medicine Khuraiya S et al. Int J Adv Med. 2019 Feb;6(1):150-154 http://www.ijmedicine.com pISSN 2349-3925 | eISSN 2349-3933 DOI: http://dx.doi.org/10.18203/2349-3933.ijam20190122 Original Research Article A cross sectional study of cutaneous manifestations in 300 patients of diabetes mellitus Sandeep Khuraiya1*, Nancy Lal2, Naseerudin3, Vinod Jain3, Dilip Kachhawa3 1Department of Dermatology, 2Department of Radiation Oncology , Gandhi Medical College, Bhopal, Madhya Pradesh, India 3Department of Dermatology, Dr. SNMC, Jodhpur, Rajasthan, India Received: 13 December 2018 Accepted: 05 January 2019 *Correspondence: Dr. Sandeep Khuraiya, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Background: Diabetes Mellitus (DM) is a worldwide problem and one of the most common endocrine disorder. The skin is affected by both the acute metabolic derangements and the chronic degenerative complications of diabetes. Methods: The present study was a one-year cross sectional study from January 2014 to December 2014. All confirmed cases of DM with cutaneous manifestations irrespective of age, sex, duration of illness and associated diseases, willing to participate in the study were included in the study. Routine haematological and urine investigations, FBS, RBS and HbA1c levels were carried out in all patients. Results: A total of 300 patients of diabetes mellitus with cutaneous manifestations were studied. -

Note for Guidance on Clinical Investigation of Medicinal Products for the Treatment of Peripheral Arterial Occlusive Disease
The European Agency for the Evaluation of Medicinal Products Evaluation of Medicines for Human Use London, 25 April 2002 CPMP/EWP/714/98 rev 1 COMMITTEE FOR PROPRIETARY MEDICINAL PRODUCTS (CPMP) NOTE FOR GUIDANCE ON CLINICAL INVESTIGATION OF MEDICINAL PRODUCTS FOR THE TREATMENT OF PERIPHERAL ARTERIAL OCCLUSIVE DISEASE DISCUSSION IN THE EFFICACY WORKING PARTY September 1999 – September 2000 TRANSMISSION TO CPMP November 2000 RELEASE FOR CONSULTATION November 2000 DEADLINE FOR COMMENTS May 2001 DISCUSSION IN THE EFFICACY WORKING PARTY November 2001 – February 2002 TRANSMISSION TO CPMP April 2002 ADOPTION BY CPMP April 2002 DATE FOR COMING INTO OPERATION October 2002 Note: This revised Note for guidance will replace the previous Note for guidance (CPMP/EWP/233/95) , adopted in November 1995. 7 Westferry Circus, Canary Wharf, London, E14 4HB, UK Tel. (44-20) 74 18 84 00 Fax (44-20) 74 18 8613 E-mail: [email protected] http://www.emea.eu.int EMEA 2002 Reproduction and/or distribution of this document is authorised for non commercial purposes only provided the EMEA is acknowledged NOTE FOR GUIDANCE ON CLINICAL INVESTIGATIONS OF MEDICINAL PRODUCTS IN THE TREATMENT OF CHRONIC PERIPHERAL ARTERIAL OCCLUSIVE DISEASE TABLE OF CONTENTS 1. INTRODUCTION .................................................................................................... 4 2. GENERAL CONSIDERATIONS REGARDING PAOD TRIALS..................... 4 2.1 PAOD Classification and Epidemiological Background ...................................... 4 2.2 Clinical Trial Features ............................................................................................ -

Peripheral Artery Disease (Pad)
PERIPHERAL ARTERY DISEASE (PAD) Provider’s guide to diagnose and code PAD Peripheral Artery Disease (ICD-10 code I73.9) is estimated The American Cardiology and American Heart Association to affect 12 to 20% of Americans age 65 and older with as 2013 revised guidelines recommend the following many as 75% of that group being asymptomatic (Rogers et al, interpretation for noncompression values for ABI 2011). Of note, for the purposes of this clinical flyer the term (Anderson, 2013). peripheral vascular disease (PVD) is used synonymously with PAD. Table 2: Interpretation of ABI Values Who and how to screen for PAD Value Interpretation The updated 2013 American College of Cardiology and > 1.30 Non-compressible American Heart Association guidelines for the management of 1.00 – 1.29 Normal patients with PAD, recommends screening patients at risk for lower extremity PAD (Anderson et al, 2013). 0.91 – 0.99 Borderline The guidelines recommend reviewing vascular signs and 0.41 - 0.90 Mild to moderate PAD symptoms (e.g., walking impairment, claudication, ischemic 0.00 – 0.40 Severe PAD rest pain and/or presence of non-healing wounds) and physical examination (e.g., evaluation of pulses and inspection The diagnostic accuracy of the ABI can be hindered under the of lower extremities). The Trans-Atlantic Inter-Society following conditions: (Ruff, 2003) Consensus Document on Management of PAD and U.S. Preventative Task Force on screening for PAD identify similar › Patient anxiety and/or discomfort screening criteria that address patient’s age, smoking history, › Poor positioning of patient or restless patient co-morbid conditions and physical exam findings (Moyer, 2013 & Norgren et al, 2007). -

Protein Profile Screening: Reduced Expression of Sord in the Mouse
REPRODUCTIONRESEARCH Protein profile screening: reduced expression of Sord in the mouse epididymis induced by nicotine inhibits tyrosine phosphorylation level in capacitated spermatozoa Jingbo Dai*, Wangjie Xu*, Xianglong Zhao, Meixing Zhang, Dong Zhang, Dongsheng Nie, Min Bao, Zhaoxia Wang, Lianyun Wang and Zhongdong Qiao School of Life Sciences and Biotechnology, Shanghai Jiao Tong University, Shanghai 200240, People’s Republic of China Correspondence should be addressed to Z Qiao; Email: [email protected] *(J Dai and W Xu contributed equally to this work) Abstract Many studies have revealed the hazardous effects of cigarette smoking and nicotine exposure on male fertility, but the actual, underlying molecular mechanism remains relatively unclear. To evaluate the detrimental effects of nicotine exposure on the sperm maturation process, two-dimensional gel electrophoresis and mass spectrometry analyses were performed to screen and identify differentially expressed proteins from the epididymal tissue of mice exposed to nicotine. Data mining analysis indicated that 15 identified proteins were mainly involved in the molecular transportation process and the polyol pathway, indicating impaired epididymal secretory functions. Experiments in vitro confirmed that nicotine inhibited tyrosine phosphorylation levels in capacitated spermatozoa via the downregulated seminal fructose concentration. Sord, a key gene encoding sorbitol dehydrogenase, was further investigated to reveal that nicotine induced hyper-methylation of the promoter region of this gene. Nicotine-induced reduced expression of Sord could be involved in impaired secretory functions of the epididymis and thus prevent the sperm from undergoing proper maturation and capacitation, although further experiments are needed to confirm this hypothesis. Reproduction (2016) 151 227–237 Introduction be detected in smokers’ serum and semen (Pacifici et al. -

IWGDF Guideline on Diagnosis, Prognosis and Management of Peripheral Artery Disease in Patients with a Foot Ulcer and Diabetes
IWGDF Guideline on diagnosis, prognosis and management of peripheral artery disease in patients with a foot ulcer and diabetes Part of the 2019 IWGDF Guidelines on the Prevention and Management of Diabetic Foot Disease IWGDF Guidelines AUTHORS Robert J. Hinchlife1, Rachael O. Forsythe2, Jan Apelqvist3, Ed J. Boyko4, Robert Fitridge5, Joon Pio Hong6, Konstantinos Katsanos7, Joseph L. Mills8, Sigrid Nikol9, Jim Reekers10, Maarit Venermo11, R. Eugene Zierler12, Nicolaas C. Schaper13 on behalf of the International Working Group on the Diabetic Foot (IWGDF) INSTITUTIONS 1 Bristol Centre for Surgical Research, University of Bristol, Bristol, UK 2 British Heart Foundation / University of Edinburgh Centre for Cardiovascular Science, University of Edinburgh, Edinburgh, Scotland, UK 3 Department of Endocrinology, University Hospital of Malmö, Sweden 4 Seattle Epidemiologic Research and Information Centre-Department of Veterans Afairs Puget Sound Health Care System and the University of Washington, Seattle, Washington, USA 5 Vascular Surgery, The University of Adelaide, Adelaide, South Australia, Australia 6 Asan Medical Center University of Ulsan, Seoul, Korea 7 Patras University Hospital School of Medicine, Rion, Patras, Greece 8 SALSA (Southern Arizona Limb Salvage Alliance), University of Arizona Health Sciences Center, Tucson, Arizona, USA 9 Asklepios Klinik St. Georg, Hamburg, Germany 10 Department of Vascular Radiology, Amsterdam Medical Centre, The Netherlands 11 Helsinki University Hospital, University of Helsinki, Finland 12 Department of Surgery, University of Washington, Seattle, Washington, USA 13 Div. Endocrinology, MUMC+, CARIM and CAPHRI Institute, Maastricht, The Netherlands KEYWORDS diabetic foot; foot ulcer; guidelines; peripheral artery disease; surgery; diagnosis; prognosis; vascular disease www.iwgdfguidelines.org IWGDF PAD Guideline ABSTRACT The International Working Group on the Diabetic Foot (IWGDF) has published evidence-based guidelines on the prevention and management of diabetic foot disease since 1999. -

Coronary Microvascular Dysfunction
Journal of Clinical Medicine Review Coronary Microvascular Dysfunction Federico Vancheri 1,*, Giovanni Longo 2, Sergio Vancheri 3 and Michael Henein 4,5,6 1 Department of Internal Medicine, S.Elia Hospital, 93100 Caltanissetta, Italy 2 Cardiovascular and Interventional Department, S.Elia Hospital, 93100 Caltanissetta, Italy; [email protected] 3 Radiology Department, I.R.C.C.S. Policlinico San Matteo, 27100 Pavia, Italy; [email protected] 4 Institute of Public Health and Clinical Medicine, Umea University, SE-90187 Umea, Sweden; [email protected] 5 Department of Fluid Mechanics, Brunel University, Middlesex, London UB8 3PH, UK 6 Molecular and Nuclear Research Institute, St George’s University, London SW17 0RE, UK * Correspondence: [email protected] Received: 10 August 2020; Accepted: 2 September 2020; Published: 6 September 2020 Abstract: Many patients with chest pain undergoing coronary angiography do not show significant obstructive coronary lesions. A substantial proportion of these patients have abnormalities in the function and structure of coronary microcirculation due to endothelial and smooth muscle cell dysfunction. The coronary microcirculation has a fundamental role in the regulation of coronary blood flow in response to cardiac oxygen requirements. Impairment of this mechanism, defined as coronary microvascular dysfunction (CMD), carries an increased risk of adverse cardiovascular clinical outcomes. Coronary endothelial dysfunction accounts for approximately two-thirds of clinical conditions presenting with symptoms and signs of myocardial ischemia without obstructive coronary disease, termed “ischemia with non-obstructive coronary artery disease” (INOCA) and for a small proportion of “myocardial infarction with non-obstructive coronary artery disease” (MINOCA). More frequently, the clinical presentation of INOCA is microvascular angina due to CMD, while some patients present vasospastic angina due to epicardial spasm, and mixed epicardial and microvascular forms. -

Collateral Glucose-Utlizing Pathwaya in Diabetic Polyneuropathy
International Journal of Molecular Sciences Review Collateral Glucose-Utlizing Pathwaya in Diabetic Polyneuropathy Hiroki Mizukami 1,* and Sho Osonoi 1,2 1 Department Pathology and Molecular Medicine, Hirosaki University Graduate School of Medicine, 5 Zaifu-cho, Hirosaki, Aomori 036-8562, Japan; [email protected] 2 Department of Endocrinology and Metabolism, Hirosaki University Graduate School of Medicine, 5 Zaifu-cho, Hirosaki, Aomori 036-8562, Japan * Correspondence: [email protected]; Tel.: +81-172-39-5025 Abstract: Diabetic polyneuropathy (DPN) is the most common neuropathy manifested in diabetes. Symptoms include allodynia, pain, paralysis, and ulcer formation. There is currently no established radical treatment, although new mechanisms of DPN are being vigorously explored. A pathophysio- logical feature of DPN is abnormal glucose metabolism induced by chronic hyperglycemia in the peripheral nerves. Particularly, activation of collateral glucose-utilizing pathways such as the polyol pathway, protein kinase C, advanced glycation end-product formation, hexosamine biosynthetic pathway, pentose phosphate pathway, and anaerobic glycolytic pathway are reported to contribute to the onset and progression of DPN. Inhibitors of aldose reductase, a rate-limiting enzyme involved in the polyol pathway, are the only compounds clinically permitted for DPN treatment in Japan, although their efficacies are limited. This may indicate that multiple pathways can contribute to the pathophysiology of DPN. Comprehensive metabolic analysis may help to elucidate global changes in the collateral glucose-utilizing pathways during the development of DPN, and highlight therapeutic targets in these pathways. Keywords: diabetic polyneuropathy; glycolysis; oxidative stress; polyol pathway; hexosamine biosynthetic pathway; advanced glycation end-products; PKC; glucosamine; pentose phosphate pathway; anaerobic glycolytic pathway Citation: Mizukami, H.; Osonoi, S. -

Intracerebral Hemorrhage
Circulation Journal ORIGINAL ARTICLE Circ J 2019; 83: 441 – 446 doi: 10.1253/circj.CJ-18-0938 Stroke Safety of Anticoagulant Therapy Including Direct Oral Anticoagulants in Patients With Acute Spontaneous Intracerebral Hemorrhage Yuki Sakamoto, MD; Chikako Nito, MD, PhD; Yasuhiro Nishiyama, MD, PhD; Satoshi Suda, MD, PhD; Noriko Matsumoto, MD, PhD; Junya Aoki, MD, PhD; Takashi Shimoyama, MD, PhD; Takuya Kanamaru, MD, PhD; Kentaro Suzuki, MD; Takuya Nishimura, MD; Masahiro Mishina, MD, PhD; Kazumi Kimura, MD, PhD Background: Because the efficacy and safety of anticoagulant therapy in patients with acute intracerebral hemorrhage (ICH) are not fully known, present study aimed to elucidate the current status and the safety of anticoagulant therapy, mainly direct oral anticoagulants (DOACs), for acute ICH and anticoagulant-indicated patients. Methods and Results: From September 2014 through March 2017, consecutive patients with acute (<7 days from onset), sponta- neous ICH were retrospectively enrolled from a prospective registry. Whether to start anticoagulation was at the attending physicians’ discretion, and thromboembolic or hemorrhagic events during hospitalization were analyzed. A total of 236 patients (80 women [34%]; median age 69 [interquartile range 61–79] years; National Institutes of Health stroke scale score 7 [3–16]) were enrolled. Of them, 47 patients (20%) had an indication for anticoagulant therapy (33 had atrial fibrillation, 14 developed deep vein thrombosis), and 41 of 47 patients (87%) were actually treated with anticoagulant therapy (DOACs were used in 34 patients) after a median of 7 days from ICH onset. There was neither hematoma expansion nor excessive hemorrhagic complications during hospitalization after starting anticoagulant therapy. -

Aldose Reductase Inhibitors: AT-001: a Next Generation Aldose Reductase Inhibitor in Development for Diabetic Cardiomyopathy (Dbcm) Francesca Lawson, MD, FAHA
Aldose Reductase Inhibitors: AT-001: a Next Generation Aldose Reductase Inhibitor in Development for Diabetic Cardiomyopathy (DbCM) Francesca Lawson, MD, FAHA Confidential Disclosures • Employee at Applied Therapeutics • Shareholder of Applied Therapeutics 2 Diabetic Cardiomyopathy: Abnormal Cardiac Structure and Functional Capacity Resulting from Diabetes-Associated Metabolic Alterations Approximately, 17-24% of patients with • ~24% of DbCM patients diabetes have DbCM in the absence of other forms of heart disease. 1,2 progress to overt heart failure or death within 1.5 years4 ~77 M patients worldwide have DbCM3 • 37% within 5 years5 • ~ 8.0M in North America • ~ 10.0M in Europe • Patients with diabetes are counseled on HF risk reduction: No Treatment for DbCM Lifestyle modification • No therapies target the metabolic derangement responsible for o o Hyperglycemia o Hypertension DbCM and subsequent worsening to overt HF o Albuminuria • Heart Failure treatment is only initiated upon onset of clinical o Dyslipidemia symptomatology (stage C heart failure) 3 1. Dandamudi et al. J Card Fail. 2014;20(5):304-309. 2. Pham et al. Intl J Endocrinology 3. International Diabetes Foundation, 2017,4. Wang et al. JACC: Cardiovasc Imaging 2018; 5. From et al. JACC 2010 Pathogenesis of DbCM & Hyperactivation of Polyol Pathway1,2 Hexokinase Glucose-6- Glycolitic Glucose Phosphate Pathway Kreb Cycle Hyperglycemia / Ischemia (Polyol Pathway Activated) Aldose Reductase Osmotic stress Sorbitol CELL DEATH Sorbitol Dehydrogenase Redox Imbalance ROS Formation Fructose Advanced Glycation PKC, NF-kB* Activation CELL DEATH *Nf-kB is a protein complex that controls transcription of DNA, cytokine production and cell survival 4 1. Brownlee M. Diabetes Care. 2005;54(6):1615-1625. -
Anti-Thrombotics in Stroke When to Start and When to Stop
Anti-Thrombotics In Stroke when to start and when to stop Ania Busza MD PhD Assistant Professor of Neurology University of Rochester School of Medicine and Dentistry No Relevent Disclosures • Research funding from NIH/NICHD (K12 award) • Materials provided for research from MC10, Inc This person was He has afib but was Outlinedischarged 1 week discharged only on ago with a subdural. aspirin – when Should they be back My patient is should I restart his on aspirin? currently on warfarin anticoagulation ? but wants to get pregnant. Is that Common questions that arise post-Stroke safe? Why is everyone The report says talking about putting “likely amyloid TIA patients on angiopathy” – what BOTH aspirin and do I do about their plavix for a few antithrombotics? weeks? Outline ? • Physiology – types of clots and the logic behind the different choices for antithrombotic therapy • Timing: When should antithrombotics be started… – after an ischemic stroke? ? ? – after a hemorrhagic stroke? • Safety: What to consider in selecting antithrombotic therapy – in pregnancy – in patients with cerebral amyloid angiopathy ? • DAPT: When is duo-antiplatelet treatment indicated? Physiology of Clots thrombosis - an obstruction of blood flow due to a localized occlusive process within one more more blood vessels. Physiology of Clots RED THROMBI WHITE THROMBI RED THROMBI • Erythrocytes + Fibrin • tend to develop in low flow situations: – dilated cardiac atria / afib – regions of ventricular hypokinesia (ventricular aneurysms, low EF, or MI) – leg/pelvic veins -

The Increasing Impact of Cerebral Amyloid Angiopathy: Essential New
JNNP Online First, published on August 26, 2017 as 10.1136/jnnp-2016-314697 Cerebrovascular disease J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp-2016-314697 on 26 August 2017. Downloaded from REVIEW The increasing impact of cerebral amyloid angiopathy: essential new insights for clinical practice Gargi Banerjee,1 Roxana Carare,2 Charlotte Cordonnier,3 Steven M Greenberg,4 Julie A Schneider,5 Eric E Smith,6 Mark van Buchem,7 Jeroen van der Grond,7 Marcel M Verbeek,8,9 David J Werring1 For numbered affiliations see ABSTRact Furthermore, CAA gained new relevance with the end of article. Cerebral amyloid angiopathy (CAA) has never been advent of anti-Aβ immunotherapies for the treat- more relevant. The last 5 years have seen a rapid ment of Alzheimer’s disease (AD), as a sizeable Correspondence to increase in publications and research in the field, with proportion of those treated went on to develop Dr David J Werring, The National Hospital for Neurology and the development of new biomarkers for the disease, imaging features of CAA-related inflammation as 5 Neurosurgery, UCL Institute thanks to advances in MRI, amyloid positron emission an unintended consequence. This, together with of Neurology, Queen Square, tomography and cerebrospinal fluid biomarker analysis. advances in our understanding of the impact of London WC1N 3BG, UK; d. The inadvertent development of CAA-like pathology CAA on cognition, in the context of ICH, ageing werring@ ucl. ac. uk in patients treated with amyloid-beta immunotherapy and AD, has broadened the clinical spectrum Received 1 March 2017 for Alzheimer’s disease has highlighted the importance of disease to which the contribution of CAA is Revised 26 April 2017 of establishing how and why CAA develops; without recognised.