The Increasing Impact of Cerebral Amyloid Angiopathy: Essential New
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Study of the Formation of Oligomers and Amyloid Plaques from Amylin by Capillary Electrophoresis and Fluorescent Microchip E
University of Arkansas, Fayetteville ScholarWorks@UARK Biological and Agricultural Engineering Biological and Agricultural Engineering Undergraduate Honors Theses 5-2015 The tuds y of the formation of oligomers and amyloid plaques from Amylin by capillary electrophoresis and fluorescent microchip electrophoresis Shane Weindel University of Arkansas, Fayetteville Follow this and additional works at: http://scholarworks.uark.edu/baeguht Part of the Engineering Commons Recommended Citation Weindel, Shane, "The tudys of the formation of oligomers and amyloid plaques from Amylin by capillary electrophoresis and fluorescent microchip electrophoresis" (2015). Biological and Agricultural Engineering Undergraduate Honors Theses. 25. http://scholarworks.uark.edu/baeguht/25 This Thesis is brought to you for free and open access by the Biological and Agricultural Engineering at ScholarWorks@UARK. It has been accepted for inclusion in Biological and Agricultural Engineering Undergraduate Honors Theses by an authorized administrator of ScholarWorks@UARK. For more information, please contact [email protected], [email protected]. The Study of the Formation of Oligomers and Amyloid Plaques from Amylin by Capillary Electrophoresis and Fluorescent Microchip Electrophoresis Shane Weindel, Biological Engineering Undergraduate Christa Hestekin, Chemical Engineering Assistant Professor Department of Biological & Agricultural Engineering 203 Engineering Hall 1 University of Arkansas Abstract Amylin, a pancreatic β-cell hormone, was the focus of this research project. This hormone is co-localized and co-secreted with insulin in response to nutrient stimuli. The hormone inhibits food intake, gastric emptying and glucagon secretion. Insulin and amylin appear to complement each other in the control of plasma glucose levels. Human amylin has a propensity to self-aggregate and to form insoluble bodies. -
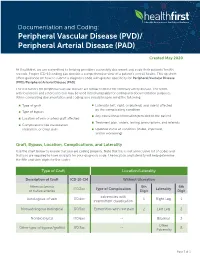
Documentationand Coding Tips: Peripheral Vascular Disease
Documentation and Coding: Peripheral Vascular Disease (PVD)/ Peripheral Arterial Disease (PAD) Created May 2020 At Healthfirst, we are committed to helping providers accurately document and code their patients’ health records. Proper ICD-10 coding can provide a comprehensive view of a patient’s overall health. This tip sheet offers guidance on how to submit a diagnosis code with greater specificity for Peripheral Vascular Disease (PVD)/Peripheral Arterial Disease (PAD). The risk factors for peripheral vascular disease are similar to those for coronary artery disease. The terms arteriosclerosis and atherosclerosis may be used interchangeably for coding and documentation purposes. When completing documentation and coding, you should keep in mind the following: Type of graft Laterality (left, right, or bilateral) and side(s) affected by the complicating condition Type of bypass Any educational information provided to the patient Location of vein or artery graft affected Treatment plan, orders, testing, prescriptions, and referrals Complications like claudication, ulceration, or chest pain Updated status of condition (stable, improved, and/or worsening) Graft, Bypass, Location, Complications, and Laterality Use the chart below to ensure that you are coding properly. Note that this is not an inclusive list of codes and that you are required to have six digits for your diagnosis code. The location and laterality will help determine the fifth and sixth digits for the codes. Type of Graft Location/Laterality Description of Graft ICD-10-CM Without -

Familial Mediterranean Fever: Effects of Genotype and Ethnicity on Inflammatory Attacks and Amyloidosis
Familial Mediterranean Fever: Effects of Genotype and Ethnicity on Inflammatory Attacks and Amyloidosis Aviva Mimouni, MD*; Nurit Magal, PhD*; Nava Stoffman, MD*; Tamy Shohat, MD*; Ara Minasian, MD‡; Michael Krasnov, MD*; Gabrielle J. Halpern, MRCPsych*; Jerome I. Rotter, MD§; Nathan Fischel-Ghodsian, MD§; Yehuda L. Danon, MDʈ; and Mordechai Shohat, MD* ABSTRACT. Objective. The gene causing familial factors other than genotype, such as environment or genes Mediterranean fever (FMF)—an autosomal recessive dis- other than MEFV, play a role in the determination of the ease characterized by recurrent short episodes of fever severity of the inflammatory attacks in FMF. Pediatrics associated most commonly with peritonitis, pleuritis, 2000;105(5). URL: http://www.pediatrics.org/cgi/content/ and arthritis—has recently been found and several mu- full/105/5/e70; amyloidosis, specific mutation, phenotype-ge- tations identified. The most severe complication of the notype correlation, ethnicity. disease is amyloidosis, which can lead to renal failure. The aim of this study was to investigate the role of genetic versus nongenetic factors on the phenotype as ABBREVIATIONS. FMF, familial Mediterranean fever; MEFV, well as on the development of amyloidosis in FMF in a Mediterranean fever (the FMF gene); PCR, polymerase chain re- large and heterogeneous group of patients. action; CI, confidence interval. Methodology. We studied 382 patients from 4 ethnic origins living in different environments: North African amilial Mediterranean fever (FMF) is an auto- Jews, other Jews, Turks, Armenians living in the United somal recessive disease affecting primarily non- States, and Armenians from Yerevan, Armenia. Informa- tion regarding amyloidosis was available for 371 pa- Ashkenazi Jews, Armenians, Turks, and Ar- F1 tients. -

Peripheral Artery Disease (Pad)
PERIPHERAL ARTERY DISEASE (PAD) Provider’s guide to diagnose and code PAD Peripheral Artery Disease (ICD-10 code I73.9) is estimated The American Cardiology and American Heart Association to affect 12 to 20% of Americans age 65 and older with as 2013 revised guidelines recommend the following many as 75% of that group being asymptomatic (Rogers et al, interpretation for noncompression values for ABI 2011). Of note, for the purposes of this clinical flyer the term (Anderson, 2013). peripheral vascular disease (PVD) is used synonymously with PAD. Table 2: Interpretation of ABI Values Who and how to screen for PAD Value Interpretation The updated 2013 American College of Cardiology and > 1.30 Non-compressible American Heart Association guidelines for the management of 1.00 – 1.29 Normal patients with PAD, recommends screening patients at risk for lower extremity PAD (Anderson et al, 2013). 0.91 – 0.99 Borderline The guidelines recommend reviewing vascular signs and 0.41 - 0.90 Mild to moderate PAD symptoms (e.g., walking impairment, claudication, ischemic 0.00 – 0.40 Severe PAD rest pain and/or presence of non-healing wounds) and physical examination (e.g., evaluation of pulses and inspection The diagnostic accuracy of the ABI can be hindered under the of lower extremities). The Trans-Atlantic Inter-Society following conditions: (Ruff, 2003) Consensus Document on Management of PAD and U.S. Preventative Task Force on screening for PAD identify similar › Patient anxiety and/or discomfort screening criteria that address patient’s age, smoking history, › Poor positioning of patient or restless patient co-morbid conditions and physical exam findings (Moyer, 2013 & Norgren et al, 2007). -

Beta Amyloid Imaging with Positron Emission Tomography For
Corporate Medical Policy Beta Amyloid Imaging With Positron Emission Tomography for Alzheimer’s Disease File Name: beta_amyloid_imaging_with_positron_emission_tomography_for_alzheimers_disease Origination: 10/2014 Last CAP Review: 5/2021 Next CAP Review: 5/2022 Last Review: 5/2021 Description of Procedure or Service Three radioactive tracers (florbetapir F18, flutemetamol F18, florbetaben F18) that bind to beta amyloid and can be detected in vivo with positron emission tomography (PET) have been developed. This technology is being evaluated to detect beta amyloid neuritic plaque density in adult patients with cognitive impairment who are being evaluated for Alzheimer disease (AD) and/or other causes of cognitive decline. Background The diagnosis of AD is divided into 3 categories: possible, probable, and definite AD. A diagnosis of definite AD requires postmortem confirmation of AD pathology, including the presence of extracellular beta amyloid plaques and intraneuronal neurofibrillary tangles in the cerebral cortex. There can be a range of beta amyloid plaques and neurofibrillary tanges on histopathology that support a low, intermediate or high probability of AD. Probable AD dementia is diagnosed clinically when the patient meets core clinical criteria for dementia and has a typical clinical course for AD. A typical clinical course is defined as an insidious onset, with the initial and most prominent cognitive deficits being either amnestic or nonamnestic, e.g., language, visuospatial, or executive function deficits, and a history of progressively worsening cognition over time. A diagnosis of possible AD dementia is made when the patient meets the core clinical criteria for AD dementia but has an atypical course or an etiologically mixed presentation. Mild cognitive impairment (MCI) may be diagnosed when there is a change in cognition, but impairment is insufficient for the diagnosis of dementia. -

A Guide to Transthyretin Amyloidosis
A Guide to Transthyretin Amyloidosis Authored by Teresa Coelho, Bo-Goran Ericzon, Rodney Falk, Donna Grogan, Shu-ichi Ikeda, Mathew Maurer, Violaine Plante-Bordeneuve, Ole Suhr, Pedro Trigo 2016 Edition Edited by Merrill Benson, Mathew Maurer What is amyloidosis? Amyloidosis is a systemic disorder characterized by extra cellular deposition of a protein-derived material, known as amyloid, in multiple organs. Amyloidosis occurs when native or mutant poly- peptides misfold and aggregate as fibrils. The amyloid deposits cause local damage to the cells around which they are deposited leading to a variety of clinical symptoms. There are at least 23 different proteins associated with the amyloidoses. The most well-known type of amyloidosis is associated with a hematological disorder, in which amyloid fibrils are derived from monoclonal immunoglobulin light-chains (AL amyloidosis). This is associated with a clonal plasma cell disorder, closely related to and not uncommonly co-existing with multiple myeloma. Chronic inflammatory conditions such as rheumatoid arthritis or chronic infections such as bronchiectasis are associated with chronically elevated levels of the inflammatory protein, serum amyloid A, which may misfold and cause AA amyloidosis. The hereditary forms of amyloidosis are autosomal dominant diseases characterized by deposition of variant proteins, in dis- tinctive tissues. The most common hereditary form is transthyretin amyloidosis (ATTR) caused by the misfolding of protein monomers derived from the tetrameric protein transthyretin (TTR). Mutations in the gene for TTR frequently re- sult in instability of TTR and subsequent fibril formation. Closely related is wild-type TTR in which the native TTR protein, particu- larly in the elderly, can destabilize and re-aggregate causing non- familial cases of TTR amyloidosis. -

Once AL Amyloidosis: Not Always AL Amyloidosis
Amyloid The Journal of Protein Folding Disorders ISSN: 1350-6129 (Print) 1744-2818 (Online) Journal homepage: http://www.tandfonline.com/loi/iamy20 Once AL amyloidosis: not always AL amyloidosis Tulip Jhaveri, Shayna Sarosiek, Frederick L. Ruberg, Omar Siddiqi, John L. Berk & Vaishali Sanchorawala To cite this article: Tulip Jhaveri, Shayna Sarosiek, Frederick L. Ruberg, Omar Siddiqi, John L. Berk & Vaishali Sanchorawala (2018): Once AL amyloidosis: not always AL amyloidosis, Amyloid, DOI: 10.1080/13506129.2018.1449104 To link to this article: https://doi.org/10.1080/13506129.2018.1449104 Published online: 08 Mar 2018. Submit your article to this journal View related articles View Crossmark data Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=iamy20 AMYLOID, 2018 https://doi.org/10.1080/13506129.2018.1449104 LETTER TO THE EDITOR Once AL amyloidosis: not always AL amyloidosis Amyloid cardiomyopathy could be related to AL amyloidosis, He continued with haematologic complete response at this wild-type transthyretin amyloidosis (ATTRwt) or hereditary time without recurrence of lymphoma. In view of continued amyloidosis (ATTRm). It is crucial to distinguish and accur- hematologic CR and new cardiomyopathy, an endomyocardial ately type the precursor amyloidogenic protein in order to biopsy (age 76 years) revealed amyloid deposition by Congo offer appropriate treatment, prognosis and genetic counsel- red staining. Microdissection and liquid chromatography ing. Treatment for AL amyloidosis is directed towards the with laser capture tandem mass spectrometry identified plasma cell dyscrasia, whereas treatment for transthyretin transthyretin protein as the precursor amyloid protein. Serum amyloidosis is directed towards stabilization of misfolded isoelectric focusing and genetic testing demonstrated normal TTR [1] or reduction in production of mutant TTR [2,3]. -

Expert Consensus Recommendations to Improve Diagnosis of ATTR Amyloidosis with Polyneuropathy
Journal of Neurology https://doi.org/10.1007/s00415-019-09688-0 REVIEW Expert consensus recommendations to improve diagnosis of ATTR amyloidosis with polyneuropathy David Adams1 · Yukio Ando2 · João Melo Beirão3 · Teresa Coelho4 · Morie A. Gertz5 · Julian D. Gillmore6 · Philip N. Hawkins6 · Isabelle Lousada7 · Ole B. Suhr8 · Giampaolo Merlini9,10 Received: 10 December 2019 / Revised: 20 December 2019 / Accepted: 23 December 2019 © The Author(s) 2020 Abstract Amyloid transthyretin (ATTR) amyloidosis with polyneuropathy (PN) is a progressive, debilitating, systemic disease wherein transthyretin protein misfolds to form amyloid, which is deposited in the endoneurium. ATTR amyloidosis with PN is the most serious hereditary polyneuropathy of adult onset. It arises from a hereditary mutation in the TTR gene and may involve the heart as well as other organs. It is critical to identify and diagnose the disease earlier because treatments are available to help slow the progression of neuropathy. Early diagnosis is complicated, however, because presentation may vary and family history is not always known. Symptoms may be mistakenly attributed to other diseases such as chronic infammatory demyelinating polyradiculoneuropathy (CIDP), idiopathic axonal polyneuropathy, lumbar spinal stenosis, and, more rarely, diabetic neuropathy and AL amyloidosis. In endemic countries (e.g., Portugal, Japan, Sweden, Brazil), ATTR amyloidosis with PN should be suspected in any patient who has length-dependent small-fber PN with autonomic dysfunction and a family history of ATTR amyloidosis, unexplained weight loss, heart rhythm disorders, vitreous opacities, or renal abnormali- ties. In nonendemic countries, the disease may present as idiopathic rapidly progressive sensory motor axonal neuropathy or atypical CIDP with any of the above symptoms or with bilateral carpal tunnel syndrome, gait disorders, or cardiac hypertro- phy. -

Cerebral Amyloidosis, Amyloid Angiopathy, and Their Relationship to Stroke and Dementia
65 Cerebral amyloidosis, amyloid angiopathy, and their relationship to stroke and dementia ∗ Jorge Ghiso and Blas Frangione β-pleated sheet structure, the conformation responsi- Department of Pathology, New York University School ble for their physicochemical properties and tinctoreal of Medicine, New York, NY, USA characteristics. So far, 20 different proteins have been identified as subunits of amyloid fibrils [56,57,60 (for review and nomenclature)]. Although collectively they Cerebral amyloid angiopathy (CAA) is the common term are products of normal genes, several amyloid precur- used to define the deposition of amyloid in the walls of sors contain abnormal amino acid substitutions that can medium- and small-size leptomeningeal and cortical arteries, arterioles and, less frequently, capillaries and veins. CAA impose an unusual potential for self-aggregation. In- is an important cause of cerebral hemorrhages although it creased levels of amyloid precursors, either in the cir- may also lead to ischemic infarction and dementia. It is a culation or locally at sites of deposition, are usually the feature commonly associated with normal aging, Alzheimer result of overexpression, defective clearance, or both. disease (AD), Down syndrome (DS), and Sporadic Cerebral Of all the amyloid proteins identified, less than half are Amyloid Angiopathy. Familial conditions in which amyloid known to cause amyloid deposition in the central ner- is chiefly deposited as CAA include hereditary cerebral hem- vous system (CNS), which in turn results in cognitive orrhage with amyloidosis of Icelandic type (HCHWA-I), fa- decline, dementia, stroke, cerebellar and extrapyrami- milial CAA related to Aβ variants, including hereditary cere- dal signs, or a combination of them. -

Expression of Atrial and Brain Natriuretic Peptides and Their Genes in Hearts of Patients with Cardiac Amyloidosis
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector 754 JACC Vol. 31, No. 4 March 15, 1998:254–65 Expression of Atrial and Brain Natriuretic Peptides and Their Genes in Hearts of Patients With Cardiac Amyloidosis GENZOU TAKEMURA, MD,*† YOSHIKI TAKATSU, MD,* KIYOSHI DOYAMA, MD,‡ HIROSHI ITOH, MD,‡ YOSHIHIKO SAITO, MD,‡ MASATOSHI KOSHIJI, MD,† FUMITAKA ANDO, MD,* TAKAKO FUJIWARA, MD,§ KAZUWA NAKAO, MD,‡ HISAYOSHI FUJIWARA, MD† Hyogo, Gifu and Kyoto, Japan Objectives. We investigated the expression of atrial natriuretic secretory granules in ventricular myoctyes of the patients with peptide (ANP) and brain natriuretic peptide (BNP) and their cardiac amyloidosis, but not in ventricular myocytes from the genes in the hearts of patients with cardiac amyloidosis and those normal control subjects. Double immunocytochemical analysis with isolated atrial amyloidosis. revealed the co-localization of ANP and BNP in the same granules Background. The expression of ANP and BNP is augmented in and that isolated atrial amyloid fibrils were immunoreactive for the ventricles of failing or hypertrophied hearts, or both. The ANP and BNP, whereas ventricular amyloid fibrils were negative expression of ANP and BNP in the ventricles of hearts with for both peptides. Both ANP mRNA and BNP mRNA were cardiac amyloidosis, which is hemodynamically similar to restric- expressed in the ventricles of the patients with cardiac amyloid- tive cardiomyopathy, is not yet known. ANP is the precursor osis but not in the normal ventricles. The autopsy study of four protein of isolated atrial amyloid. patients with cardiac amyloidosis revealed an almost transmural Methods. -
Recognizing TTR-FAP Transthyretin Familial Amyloid Polyneuropathy
This version is Global RC approved and local adaptation and approval is mandatory before distribution. Countries are responsible for language accuracy. Content to be updated with local information and labeling as required. Recognizing TTR-FAP Transthyretin Familial Amyloid Polyneuropathy About TTR-FAP TTR-FAP is a rare, genetic, TTR-FAP is caused by a mutation in the transthyretin gene, which can result in abnormal and unstable progressive and fatal transthyretin proteins. 2,3 neurodegenerative disease affecting an estimated 10,000 people worldwide.1 TTR-FAP – A Disease of Protein Misfolding Free Tetramer Folded Misfolded Toxic Intermediates Monamer Monamer & Amyloid Fibrils TTR-FAP affects men and women equally. Monamer Aggregation Misfolding Functional TTR Structures TTR Structures Symptoms usually begin to affect Associated with Pathology people in their 30s. These abnormal proteins build up and form toxic This varies with genetics and structures called amyloid fibrils, which may deposit in the peripheral nervous system, leading to a decline in ethnic background.2,3 The life neurologic function, or in other parts of the body, such expectancy for someone who as the heart, digestive system, and kidneys.2,3,4,5,6,7 is diagnosed with TTR-FAP is said to be about 10 years.13 Where is TTR-FAP Most Prevalent? There are clusters of TTR-FAP patients in Portugal, Japan, and Sweden.8 TTR-FAP is also found in countries such as the United States, various countries in Europe (e.g., France, Italy, Spain, Germany, and UK), Brazil, and Taiwan.9 Prevalence of TTR-FAP may vary by country of origin and by the type of TTR gene mutation.10 Symptoms of TTR-FAP Symptoms vary, but often, the feet Later, weakness gets worse in the and legs are affected first—with legs.11 The arms may be affected pain, tingling, numbness, or loss of too, starting at the figertips.11 the ability to feel hot and cold.11 Why Early Diagnosis is Key Although the disease affects people differently, it typically gets worse over time and can progress rapidly. -

Cardiac Amyloidosis
Cardiac Amyloidosis Ronald Witteles, MD Stanford University & Brendan M. Weiss, MD University of Pennsylvania Amyloidosis: What is it? • Amylum – Starch (Latin) • Generic term for many diseases: • Protein misfolds into β-sheets • Forms into 8-10 nm fibrils • Extracellular deposition into amyloid deposits Types of Amyloid – Incomplete List • Systemic: • Light chains (AL) – “Primary ” • Transthyretin (ATTR) – “Senile ” or “Familial ” or “FAC” or “FAP” • Serum amyloid A (AA) – “Secondary ” • Localized – Not to be memorized! • Beta-2 microglobulin (A-β2) – Dialysis (osteoarticular structures) • Apolipoprotein A-1 (AApoA-I) – Age-related (aortic intima, cardiac, neuropathic) • Apolipoprotein A-2 (AApoA-2) – Hereditary (kidney) • Calcitonin (ACal) – Complication of thyroid medullary CA • Islet amyloid polypeptide (AIAPP) – Age-related (seen in DM) • Atrial natriuretic peptide (AANF) – Age-related (atrial amyloidosis) • Prolactin (APro) – Age-related, pituitary tumors • Insulin (AIns) – Insulin-pump use (local effects) • Amyloid precursor protein (ABeta) – Age-related/hereditary (Alzheimers) • Prion protein (APrPsc) – Hereditary/sporadic (spongiform encephalopathies) • Cystatin-C (ACys) – Hereditary (cerebral hemorrhage) • Fibrinogen alpha chain (AFib) – Hereditary (kidney) • Lysozome (ALys) – Hereditary (Diffuse, especially kidney, spares heart) • Medin/Lactadherin – Age-related (medial aortic amyloidosis) • Gelsolin (AGel) – Hereditary (neuropathic, corneal) • Keratin – Cutaneous AL: A Brief Dive into Hematology… Plasma cells: Make antibodies