Spatiotemporal and Molecular Epidemiology of Cutaneous Leishmaniasis in Libya
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nationwide School Assessment Libya Ministry
Ministry of Education º«∏©àdGh á«HÎdG IQGRh Ministry of Education Nationwide School Assessment Libya Nationwide School Assessment Report - 2012 Assessment Report School Nationwide Libya LIBYA Libya Nationwide School Assessment Report 2012 Libya Nationwide School Assessment Report 2012 º«∏©àdGh á«HÎdG IQGRh Ministry of Education Nationwide School Assessment Libya © UNICEF Libya/2012-161Y4640/Giovanni Diffidenti LIBYA: Doaa Al-Hairish, a 12 year-old student in Sabha (bottom left corner), and her fellow students during a class in their school in Sabha. Doaa is one of the more shy girls in her class, and here all the others are raising their hands to answer the teacher’s question while she sits quiet and observes. The publication of this volume is made possible through a generous contribution from: the Russian Federation, Kingdom of Sweden, the European Union, Commonwealth of Australia, and the Republic of Poland. The contents of this publication are the sole responsibility of the authors and can in no way be taken to reflect the views of the donors. © Libya Ministry of Education Parts of this publication can be reproduced or quoted without permission provided proper attribution and due credit is given to the Libya Ministry of Education. Design and Print: Beyond Art 4 Printing Printed in Jordan Table of Contents Preface 5 Map of schools investigated by the Nationwide School Assessment 6 Acronyms 7 Definitions 7 1. Executive Summary 8 1.1. Context 9 1.2. Nationwide School Assessment 9 1.3. Key findings 9 1.3.1. Overall findings 9 1.3.2. Basic school information 10 1.3.3. -

1. the Big Picture Political Security
Libya Weekly Political Security Update Bell Whispering Bell March 17, 2020 1. The Big Picture Oil crisis to take centre stage amid COVID-19 concerns While ,fighting remains limited to bouts of violence More importantly, the LNA is expected to exploit the and intermittent skirmishes between Libyan situation to strengthen its case for accessing oil & National Army (LNA) and Government of National gas revenues. Of note, the blockade on exports Accord (GNA) forces, reinforcements continue to orchestrated by pro-LNA tribes continues to deepen underline the prospect of an escalation in Libya’s with losses now estimated at 3 billion USD west, especially along the Sirte-Weshka-Abugrein according to the National Oil Corporation (NOC). engagement axes. Reports of large GNA-aligned The oil crisis was the centre of Haftar’s Paris and CONTENTS Misrata military reinforcements were spotted Berlin visits. France’s diplomacy made it clear this arriving in Abugrein to join the GNA’s Sirte-Jufra week that Haftar forms an integral part of Libya’s Ops Room on 09 March. In response, the LNA’s future. Haftar met with French President Emmanuel 1 general command mobilised additional resources Macron and expressed commitment to abide by a THE BIG PICTURE towards Weshka - Abugrein on 10 March. ceasefire if GNA forces comply. Haftar’s Paris visit Oil crisis to take centre stage was low-profile and no official communique was amid COVID-19 concerns The LNA led by Khalifa Haftar continues to claim it released, leading French media to underline the is monitoring GNA preparations for a broader Elysee’s low confidence in a resolution. -

1 Department of the Treasury Office of Foreign Assets
This document is scheduled to be published in the Federal Register on 11/23/2011 and available online at http://federalregister.gov/a/2011-30293, and on FDsys.gov DEPARTMENT OF THE TREASURY OFFICE OF FOREIGN ASSETS CONTROL REMOVAL FROM THE LIST OF SPECIALLY DESIGNATED NATIONALS AND BLOCKED PERSONS OF CERTAIN ENTITIES LISTED PURSUANT TO EXECUTIVE ORDER 13566 AGENCY: Office of Foreign Assets Control, Treasury. ACTION: Notice. ---------------------- SUMMARY: The Treasury Department's Office of Foreign Assets Control (“OFAC”) is removing from the list of Specially Designated Nationals and Blocked Persons (“SDN List”) the names of 42 entities that are listed pursuant to Executive Order 13566 of February 25, 2011, “Blocking Property and Prohibiting Certain Transactions Related to Libya.” DATES: The removal from the SDN List of the 42 entities identified in this notice is effective on November 18, 2011. FOR FURTHER INFORMATION CONTACT: Assistant Director for Sanctions Compliance & Evaluation, tel.: 202-622-2490, Assistant Director for Licensing, tel.: 202-622-2480, Assistant Director for Policy, tel.: 202-622-4855, Office of Foreign Assets Control, or Chief Counsel (Foreign Assets Control), tel.: 202-622-2410, Office of the General Counsel, Department of the Treasury (not toll free numbers). SUPPLEMENTARY INFORMATION: Electronic and Facsimile Availability 1 This document and additional information concerning OFAC are available from OFAC’s Web site (www.treasury.gov/ofac) or via facsimile through a 24-hour fax-on-demand service, tel.: 202/622-0077. Background On February 25, 2011, the President issued Executive Order 13566, “Blocking Property and Prohibiting Certain Transactions Related to Libya” (“E.O. 13566”), pursuant to, inter alia, the International Emergency Economic Powers Act (50 U.S.C. -

Factors Affecting Recent Vegetation Change in North-East Libya
FACTORS AFFECTING RECENT VEGETATION CHANGE IN NORTH-EAST LIBYA GHADA. M. A. AHWAIDI Ecosystems and Environment Research Centre School of Environment and Life Sciences University of Salford Salford, M5 4WT, UK Submitted in Partial Fulfilment of the Requirements of the Degree of Doctor of Philosophy, 19 July 2017 i Contents Table of contents…………………………………………………………………… ... i List of tables………………………………………………………………………….. v List of figures………………………………………………………………………….. vi Acknowledgements……………………………………………………………………. ix Declaration…………………………………………………………………………….. x Abstract………………………………………………………………………………… xi CHAPTER 1: INTRODUCTION…………………………………………………..… 1 1.1 Introduction to the research……………………………………………… 1 1.2 Research aims and objectives……………………………………………. 4 1.3 Thesis structure………………………………………………………….. 7 CHAPTER 2: LITERATURE REVIEW……………………………………….…... 10 2.1 Introduction ……………………………………………………………... 10 2.2 Vegetation cover change in the Mediterranean region…………………... 11 2.3 Factors affecting vegetation change……………………………………... 12 2.3.1 General factors affecting vegetation change…………………………...… 12 2.3.2 Effects of human activity on vegetation change in the Mediterranean region 13 2.3.3 Effect of climate change on vegetation in the Mediterranean region….… 14 2.4 Approaches to monitoring vegetation change……………………………. 17 2.4.1 Ground based measurement of vegetation……………………………….. 18 2.4.1.1 Vegetation cover …………………………………………………………. 18 2.4.1.2 Leaf area index…………………………………………………………… 19 2.4.1.3 Density…………………………………………………………………… 19 2.4.2 Remote sensing of vegetation change……………………………………. 19 2.4.2.1 Spectral response of vegetation…………………………………………… 20 2.4.2.2 Vegetation Indices (VI)…………………………………………………... 22 2.4.2.2.1 Normalized Difference Vegetation Index (NDVI)……………………….. 22 2.4.2.2.2 Soil Adjusted Vegetation Index (SAVI)………………………………….. 23 2.4.2.2.3 Enhance Vegetation Index (EVI)…………………………………………. 24 2.4.2.3 Image classification………………………………………………………. 25 2.5 Remote sensing of vegetation change in the Mediterranean…………….. -

Proposed Alternate Electoral Law for Selection of Libya's
Proposed Alternate Electoral Law for Selection of Libya’s Constitutional Assembly Issued by the Libyan Women’s Platform for Peace, in partnership with a coalition of Libyan civil society organizations (Based on and combines Azza Maghur’s , Abdel Qader Qadura’s and Younis Fanoush’s proposals) The Electoral districts shall be divided according to the following: 1.The Eastern District: The Benghazi district, Al-Bayda’ district, Ajdabia district, Darna district, Tobruq district. Each district shall be allocated five seats (four seats for the list and one for the individual). 2. The Western District: 7 seats (6 lists + 1 individual) for Tripoli district, 5 seats (4 lists+ 1 individuals) for Misrata district, 3 seats ( 2 lists + 1 individual) for Sert district, 5 seats ( 4 lists+ 1 individuals) for Zawiyah district. 3.The Southern district: Sabha district. Ubari district. Each district shall be allocated ten seats. (8 seats for the lists and two for the individuals). The election shall be held according to the closed list system. Lists, each of which include five candidates, shall compete according to the mentioned criteria and terms. Any list that does meet such terms shall not be illegible for competition. Those wishing to participate in the election blocs and political entities, individually or collectively within a coalition, may apply through independent lists. The elections shall be carried out according to the absolute majority criterion, hence one integrated list shall win the elections. Should no list win the absolute majority of the votes of the electoral roll (50% + 1) in the first round, a second round shall be held a week after the first round of elections is held. -

The Tide Turns
November 2011 Anthony Bell, Spencer Butts, and David Witter THE LIBYAN REVOLUTION THE TIDE TURNS PART 4 Photo Credit: Fighters for Libya’s interim government rejoice after winning control of the Qaddafi stronghold of Bani Walid, via Wikimedia Commons. All rights reserved. Printed in the United States of America. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording, or any information storage or retrieval system, without permission in writing from the publisher. ©2011 by the Institute for the Study of War. Published in 2011 in the United States of America by the Institute for the Study of War. 1400 16th Street NW, Suite 515 Washington, DC 20036. http://www.understandingwar.org Anthony Bell, Spencer Butts, and David Witter THE LIBYAN REVOLUTION THE TIDE TURNS PART 4 ABOUT THE AUTHORS Anthony Bell is a Research Assistant at ISW, where he conducts research on political and security dynamics on Libya. He has previously studied the conflicts in Afghanistan and Iraq, and published the ISW report Reversing the Northeastern Insurgency. Anthony holds a bachelor’s degree from the George Washington University in International Affairs with a concentration in Conflict and Security. He graduated magna cum laude and received special honors for his senior thesis on the history of U.S. policy towards Afghanistan. He is currently a graduate student in the Security Studies Program at Georgetown University. Spencer Butts is a Research Assistant for the Libya Project at ISW. Prior to joining ISW, Mr. Butts interned at the Peacekeeping and Stability Operations Institute at the Army War College where he wrote a literature review of the Commander’s Emergency Response Program in Iraq. -

Agriculture and Rural Livelihoods Needs Assessment – Libya 1 1
Agriculture and Rural Livelihoods Needs Assessment – Libya 1 1 Agriculture and Rural Livelihoods Needs Assessment – Libya 2 Agriculture and Rural Livelihoods Needs Assessment – Libya Agriculture and Rural Livelihoods Needs Assessment – Libya 3 EXECUTIVE SUMMARY In the aftermath of the 2011 fall of Muammar Gaddafi’s rule in Libya, a power struggle for control of the country developed into an ongoing civil war, resulting in population displacements and disrupting household livelihoods. In addition to the conflict, Libya’s location and internal political instability caused the country to become a key transitory point for African and Middle Eastern migrants traveling to Europe. Previous studies indicate that foreign migrants have historically played a key role in agricultural labor work within the country. In order to develop and implement future interventions to support Libya’s agricultural sector, information is needed relating to the impacts of the ongoing political crisis on the sector (for local, displaced, and migrant populations), current needs, and entry points for agriculture support programs. To fill this information gap, FAO conducted a rapid agricultural needs assessment in August 2017. Key findings The findings of this study show that agriculture still represents an important source of income in rural areas, with notable regional variations. In the east and south, the population heavily depends on salaries and pensions provided by the government or private sector, while agricultural activities are generally considered secondary income sources. In the west, meanwhile, there is a higher dependency on agriculture as an income source as these areas have some larger scale farms. Eastern, southern and western districts alike hold a strong potential to enhance their agricultural production. -

Overview of the International Health Sector Support to Public Health Facilities | Libya January to July 2021
Overview of the International Health Sector Support to public health facilities | Libya January to July 2021 Health Sector Libya, September 2021 Contents 1) Introduction .............................................................................................................................. 2 2) Nation-wide analysis ................................................................................................................. 2 2.1) Kinds of support .................................................................................................................... 4 3) District based analysis: .............................................................................................................. 5 3.1) Support by Organization ....................................................................................................... 6 3.2) Kinds of support .................................................................................................................... 7 Annex-I | List of Organizations per their supported public health facilities: ..................................... 9 Annex-II | List of provided support by type, at a district level ......................................................... 10 Health Sector | Libya Page 1 of 10 1) Introduction This report provides analysis of the delivered assistance by international health sector partners to the MoH public health facilities in Libya, from January to July 2021. A standardized template was designed and shared with sector partners to assess different types of -

Incidence of Cystic Echinococcosis in Libya: I. Seroprevalence of Hydatid Disease in Sheep and Goats Naturally Exposed to the Infection in the North Midland Region
American Journal of Animal and Veterinary Sciences s Original Research Paper Incidence of Cystic Echinococcosis in Libya: I. Seroprevalence of Hydatid Disease in Sheep and Goats Naturally Exposed to the Infection in the North Midland Region 1Mohamed M. Ibrahem, 2Badereddin B. Annajar and 3Wafa M. Ibrahem 1Department of Zoology, Faculty of Science, University of Zawia, P.O. Box 16418, Zawia, Libya 2National Centre for Disease Control, Ain Zara, P.O. Box 71171, Tripoli, Libya 3Department of Parasitology, Faculty of Medicine, University of Zawia, P.O. Box 16418, Zawia, Libya Article history Abstract: Hydatid disease is one of the most and serious public health and Received: 28-05-2016 veterinary problems in Libya and other North African countries. Thirteen Revised: 28-09-2016 rural villages of two main districts bordered to each other at the north Accepted: 27-10-2016 midland of the country namely, Misrata which is almost agricultural area and about 200 km east of Tripoli and Sirt which is almost pasture area and Corresponding Author: Mohamed M. Ibrahem about 500 km east of Tripoli, were included in the current study. Incidence Department of Zoology, of cystic echinococcosis was investigated serologically using serum Faculty of Science, University samples collected from 2651 animals of three groups; young sheep under of Zawia, P.O. Box 16418, two years old (240), adult sheep over two years old (2082) and adult goats Zawia, Libya over two years old (329). Antigen B prepared from camel crude hydatid Email: [email protected] cyst fluid together with ELISA were used for detection of total IgG antibodies against hydatid cysts in the collected serum samples. -

Proposed Alternate Electoral Law for Selection of Libya’S Constitutional Assembly
Proposed Alternate Electoral Law for Selection of Libya’s Constitutional Assembly Issued by the Libyan Women’s Platform for Peace, in partnership with a coalition of Libyan civil society organizations (Based on Azza Maghur’s , Abdel Qader Qadura’s and Younis Fanoush’s proposals) The electoral districts shall be divided into the following: 1. The Eastern Region: The Benghazi district, Al-Bayda’ district, Ajdabia district, Darna district, Tobruq district Each district shall be allocated five seats (four seats for the list and one for the individual). 2. The Western Region: Tripoli district, Misrata district, Sert district, Zawiyah district Each district shall be allocated five seats. 3.The Southern Region: Sabha district. Ubari district. Each district shall be allocated ten seats (eight seats for the lists and two for the individuals). The election shall be held according to the closed list system. Lists, each of which will include five candidates, shall compete according to the mentioned criteria and terms. Any list that does meet such terms shall not be illegible for competition. For the purpose of participating in the elections blocs and political entities, individually or collectively within a coalition, may apply through independent lists. The elections shall be carried out according to the absolute majority criterion, hence one integrated list shall win the elections. Should no list win the absolute majority of the votes of the electoral roll (50% + 1) in the first round, a second round shall be held after a week as of the date of the first round. In the second round, the elections shall be held between the two lists that came in first and second in the first round. -
Libya Complex Emergency Fact Sheet #1
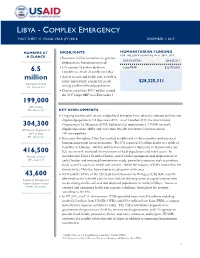
YEMEN - COMPLEX EMERGENCY FACT SHEET #7, FISCAL YEAR (FY) 2016 JANUARY 1, 2016 LIBYA - COMPLEX EMERGENCY FACT SHEET #1, FISCAL YEAR (FY) 2018 DECEMBER 1, 2017 NUMBERS AT HIGHLIGHTS HUMANITARIAN FUNDING FOR THE LIBYA RESPONSE IN FY 2016–2017 A GLANCE Insecurity in Libya continues to generate USAID/OFDA1 $4,625,311 displacement, humanitarian needs UN records 23 civilian deaths in State/PRM2 $23,700,000 6.5 October as a result of conflict in Libya million Access to cash and health care, as well as safety and security, remain key needs $28,325,311 Population of Libya UN – September 2017 among conflict-affected populations Donors contribute $85.7 million toward the 2017 Libya HRP as of December 1 199,000 IDPs in Libya IOM – October 2017 KEY DEVELOPMENTS Ongoing conflict, civil unrest, and political instability have adversely affected civilians and displaced populations in Libya since 2011. As of October 2017, the International 304,300 Organization for Migration (IOM) had identified approximately 199,000 internally IDP Returns Registered in displaced persons (IDPs) and more than 304,300 cumulative returnees across 2017 to Date 100 municipalities. IOM – October 2017 Insecurity throughout Libya has resulted in additional civilian casualties and increased humanitarian needs in recent months. The UN reported 23 civilian deaths as a result of hostilities in October. Military activity in northeastern Libya’s city of Darnah since late 416,500 July has severely restricted the movement of local populations and relief actors. In Migrants in Libya northwestern Libya’s Sabratha District, armed clashes prompted rapid displacement in IOM – August 2017 early October and increased humanitarian needs, particularly access to cash to purchase food, as well as access to health care services. -
LET4CAP Law Enforcement Training for Capacity Building LIBYA
G N I N I A R T T N E M E C R O F N E W A L LAW ENFORCEMENT TRAINING FOR CAPACITY BUILDING Co-funded by the Internal Security Fund of the European Union LET4CAP Law Enforcement Training for Capacity Building LIBYA Downloadable Country Booklet DL. 2.5 (Version 1.2) 1 Dissemination level: PU Let4Cap Grant Contract no.: HOME/ 2015/ISFP/AG/LETX/8753 Start date: 01/11/2016 Duration: 33 months Dissemination Level PU: Public X PP: Restricted to other programme participants (including the Commission) RE: Restricted to a group specified by the consortium (including the Commission) Revision history Rev. Date Author Notes 1.0 20/12/2017 SSSA Overall structure and first draft 1.1 23/02/2018 SSSA Second version after internal feedback among SSSA staff 1.2 10/05/2018 SSSA Final version version before feedback from partners LET4CAP_WorkpackageNumber 2 Deliverable_2.5 VER1.2 WorkpackageNumber 2 Deliverable Deliverable 2.5 Downloadable country booklets VER V.1.2 2 LIBYA Country Information Package 3 This Country Information Package has been prepared by Claudia KNERING, under the scientific supervision of Professor Andrea de GUTTRY and Dr. Annalisa CRETA. Scuola Superiore Sant’Anna, Pisa, Italy www.santannapisa.it LET4CAP, co-funded by the Internal Security Fund of the European Union, aims to contribute to more consistent and efficient assistance in law enforcement capacity building to third countries. The Project consists in the design and provision of training interventions drawn on the experience of the partners and fine-tuned after a piloting and consolidation phase.