Texture E Eat Well with a Soft Diet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Isaiah Davenport House Volunteer Newsletter December 2009 236-8097
Isaiah Davenport House Volunteer Newsletter December 2009 www.davenporthousemuseum.org 236-8097 The Happy Condition DAVENPORT HOUSE CALENDAR November 30 at 10 a.m. and The man who, for life, is blest with a Tuesday, December 1 – Wreath Tuesday, December 1 at 2 p.m. wife, decorating We could use some docents to help Is sure, in a happy condition: 2 p.m. – Review and refresher with the Holly Jolly tours which take Go things as they will, she’s fond of for docents of December inter- place on all nights between Novem- him still, pretation ber 27 and December 23. Old She’s comforter, friend and physician. November 30 through December Town Trolley has a wonderful crew 4 in the afternoon – Prep for of docents and the DH and OTT Pray where is the joy, to trifle and toy! Holiday Bazaar split tour guide duties. Some nights Yet dread some disaster from beauty! Friday, December 4 from 5 to 7 there are two or more trolleys and But sweet is the bliss of a conjugal kiss, p.m. – Annual Christmas Party on Monday, December 7 there will Where love mingles pleasure with – y’all come! be 5! Jamie, Jeff and Raleigh set up duty. Saturday, December 5 from 10 and give tours. So far Jody Leyva, a.m. to 5 p.m. and Sunday, Maria Sanchez and Anthony San- One extravagant Miss won’t cost a December 6 from 1 to 5 p.m. chez have agreed to help as well. man less – Holiday Bazaar at the Ken- Any others of you who can help us Than twenty good wives that are sav- nedy Pharmacy spread the Christmas cheer!? ing; Tuesday, December 8 all day – For, wives they will spare, that their Alliance for Response (Disaster SHOP NEWS : children may share, Planning) Workshop in Savan- - REMEMBER YOUR But Misses forever are craving. -

10229119.Pdf
T.C. ĠSTANBUL AYDIN ÜNĠVERSĠTESĠ FEN BĠLĠMLERĠ ENSTĠTÜSÜ SÜTLÜ TATLI ÜRETĠMĠ YAPAN BĠR ĠġLETMEDE ISO 22000 GIDA GÜVENLĠĞĠ YÖNETĠM SĠSTEMĠNĠN ĠNCELENMESĠ YÜKSEK LĠSANS TEZĠ Burcu ÇEVĠK Gıda Güvenliği Anabilim Dalı Gıda Güvenliği Programı Tez DanıĢmanı Prof. Dr. Haydar ÖZPINAR Aralık, 2018 ii T.C. ĠSTANBUL AYDIN ÜNĠVERSĠTESĠ FEN BĠLĠMLERĠ ENSTĠTÜSÜ SÜTLÜ TATLI ÜRETĠMĠ YAPAN BĠR ĠġLETMEDE ISO 22000 GIDA GÜVENLĠĞĠ YÖNETĠM SĠSTEMĠNĠN ĠNCELENMESĠ YÜKSEK LĠSANS TEZĠ Burcu ÇEVĠK (Y1613.210011) Gıda Güvenliği Anabilim Dalı Gıda Güvenliği Programı Tez DanıĢmanı Prof. Dr. Haydar ÖZPINAR Aralık, 2018 ii iv YEMĠN METNĠ Yüksek Lisans Tezi olarak sunduğum „‟Sütlü Tatlı Üretimi Yapan Bir ĠĢletmede TS EN ISO 22000 Gıda Güvenliği Yönetim Sisteminin Ġncelenmesi‟‟ adlı tezin proje safhasından sonuçlanmasına kadarki bütün süreçlerde bilimsel ahlak ve geleneklere aykırı düĢecek bir yardıma baĢvurulmaksızın yazıldığını ve yararlandığım eserlerin Bibliyografya‟da gösterilenlerden oluĢtuğunu, bunlara atıf yapılarak yararlanılmıĢ olduğunu belirtir ve onurumla beyan ederim. ( / /2018) Burcu ÇEVĠK v vi ÖNSÖZ Yüksek lisans eğitimim boyunca benden bilgilerini, deneyimlerini ve yardımlarını esirgemeyen baĢta değerli tez danıĢmanım Prof. Dr. Haydar ÖZPINAR‟a tez çalıĢmam boyunca yardımlarını esirgemeyen, Dr. Öğr. Üyesi Ayla Ünver ALÇAY‟a ve Dr. Öğr. Üyesi Burcu Çakmak SANCAR‟a çalıĢmalarımda her an yanımda olduğu için değerli arkadaĢlarım Gamze BENLĠKURT ve Çiğdem SÖKMEN‟e Hayatım boyunca benden maddi ve manevi desteklerini esirgemeyen, varlıklarıyla beni onurlandıran -

Supplementary Table S2. Food Items Within Each Other Food Group Food
Supplementary Table S1: Individual food items within each major protein source food group Food group Individual food items Red meat beef; lamb; pork Processed meat sausage; bacon; ham Poultry crumbed chicken; chicken/poultry Oily fish oily fish Non‐oily fish white fish; breaded fish; battered fish; tinned tuna Legumes/pulses baked beans; pulses; hummus Vegetarian protein soy burgers/sausages; tofu; Quorn; other vegetarian alternatives alternatives salted peanuts; unsalted peanuts; salted other nuts; unsalted Nuts other nuts low fat hard cheese; hard cheese; soft cheese; blue cheese; low fat Cheese cheese spread; cheese spread; cottage cheese; feta cheese; mozarella cheese; goat cheese; other cheese Yogurt full fat yogurt; low fat yogurt whole milk; semi‐skimmed milk; skimmed milk; powdered milk; Dairy milk goat/sheep milk soya milk with calcium; soya milk without calcium; rice/oat other Plant milk vegetable milk whole eggs; omelette; eggs disaggregated from mayonnaise in Eggs egg sandwiches Supplementary Table S2. Food items within each other food group Food group Individual items stewed/cooked fruit; prunes; other dried fruit; mixed fruit; apple; banana; berries; cherries; grapefruit; grapes; mango; Fruit melon; orange; orange‐like small fruits; peach, nectarine; pear; pineapple; plum; other fruit mixed vegetables; vegetable pieces; coleslaw; mixed side salad; avocado; broad beans; green beans; beetroot; broccoli; butternut squash; cabbage; carrots; cauliflower; celery; Vegetables courgette; cucumber; garlic; leeks; lettuce; mushrooms; -

CAFE BAR & AFTERNOON TEA P 4,5 DESSERT & CHAMPAGNE P 6,7 COCKTAILS P 8,9 WINE LIST P 10, 11 DRINKS P 12, 13 CIGARS P 14, 15
CONTENTS BREAKFAST & PASTRY p 2,3 CAFE BAR & AFTERNOON TEA p 4,5 DESSERT & CHAMPAGNE p 6,7 COCKTAILS p 8,9 WINE LIST p 10, 11 DRINKS p 12, 13 CIGARS p 14, 15 -HUTCHESONS- -SUNDAYS- PROUD MEMBERS OF THE THE HUTCHESONS’ SCOTCH BEEF CLUB ROAST Sliced roast Sirloin of Borders beef, with all the classic trimmings £14.95 Join us in our cafe / bar or brasserie from 12.30pm-4pm 01 • BR EAKFAST • MONDAY - SATURDAY 9-11.30am SUNDAY 10-12.30pm – EGGS – – PASTRY – EGGS BENEDICT £5.95 || £8.95 BUTTERED CROISSANT £2.25 PAIN AU CHOCOLAT £2.25 EGGS ROYAL £6.95 || £9.95 CROISSANT AUX AMANDES £2.75 EGGS FLORENTINE (v) £5.95 || £8.95 CRANBERRY TWIST £2.95 OMELETTE ARNOLD TRIPLE CHOCOLATE MUFFIN £2.95 BENNETT £9.50 WHITE CHOCOLATE AND OMELETTE LEMON MUFFIN £2.95 AUX FINES HERBES (v) £6.95 TOASTED BAGUETTE £2.25 Butter & jam AVOCADO, LEMON AND CHILLI ON TOAST WITH Selection of home-made POACHED EGG (v) £6.95 Fruit Preserves £1.00 SCOTTISH SMOKED SALMON AND SCRAMBLED EGGS £9.95 Toasted english muffin TO GO KEDGEREE £8.95 ALL PASTRY TEA & COFFEE AVAILABLE TO GO STEAK & EGGS £13.95 28 day dry aged Scotch rump steak, fried egg, home fries CARAMELISED 2 BOILED EGGS & SOLDIERS £5.25 PINK GRAPEFRUIT (v) £3.95 PANCAKES (v) £7.50 PORRIDGE & HONEY £4.50 Caramelised banana, chocolate & Canadian maple syrup CHARCUTERIE £9.95 Iberico chorizo, lomo, serrano SIDES £1.50 each & salami Bacon, sausage, egg any style,mushrooms THE FULL VEGETARIAN HUTCHESONS FRY BREAKFAST (v) Pork sausage, bacon, Stornoway black Vegetarian sausage and haggis, pudding, tomato, mushrooms, home -

5 Minced and Moist Food Level 5
Name: ………………………………………………………… Tel: 01225 824333 Date: ……………………………………………..…………… Speech & Language Therapist: …………………………. Minced and Moist Food 5 Level 5 5 General description: Food is soft, tender and moist. Needs very little chewing and no biting. Food has been mashed up before serving. Small lumps visible within the food (no greater than 4mm in size). Lumps are easy to squash with the tongue. It usually requires a smooth sauce, gravy or custard, which should be very thick. No mixed (thick - thin) textures e.g. cereal in milk, mince in gravy, dried fruit in sponge. No thin loose fluid. No hard, tough, chewy (toffee), fibrous (dry roasted meat), stringy (pineapple, celery), dry, crispy, crunchy (toast, flaky pastry) or crumbly bits (bread crusts, dry biscuits). No pips, seeds, pith, membrane, e.g. citrus fruit, tomatoes. No skins or outer shells e.g. on peas, grapes. No husks. No skin e.g. on sausages (use skinless ones), bone or gristle. No round or long-shaped foods e.g. grapes, sweets. No hard chunks e.g. pieces of apple. No sticky foods e.g. cheese chunks, marshmallows. Check before serving/eating: • No hard pieces, crusts or skins have formed during cooking/heating/standing. • Fluid/gravy/sauce/custard in or on the food has not thinned out or separated off. Please turn over for more information Based on Dysphagia Diet Food Texture Descriptors March 2012 and IDDSI (International Dysphagia Diet Standardisation Initiative) Framework – April 2018 Minced and Moist Food 5 Level 5 5 Meat • Must be finely minced – pieces approximately 4mm. No hard bits of mince. • Serve in a very thick, smooth sauce or gravy. -

Jellies and Syllabub . . . and How Different Our Worlds Are
Delightful Holiday Concoctions – Jellies and Syllabub . And how different our worlds are . By Jamie Credle, Davenport House Have you noticed when visiting one of the fine 18th century houses such as those in Colonial Williamsburg the arrangement of small cylindrical glasses with colorful jellies and creams inside that centers the festive table? In the grandest of homes, such as the Governor’s Palace, these glasses are often arranged in a dessert pyramid of glass salvers. Sometimes placed around the jellies and creams are sweetmeats and cakes. Because of their placement one expects that they were a highlight both for the eye and as well as the appetite. And then you wonder, ―What is that gelatinous mixture? Is that Jell-O?‖ Without refrigeration or electric mixers or prepackaged gelatin, how did that work? The two ―treats‖ noted by historians and historic cookbooks as filling these glasses are fruit flavored jellies and syllabub, both of which have long culinary histories and may be completely unfamiliar to the modern foodie. One source notes that syllabub, served either as a frothy dessert or beverage, was a 16th century invention. The determination on whether it is a drink or a dessert is how much wine is used in the recipe. Less would get you a spoonable dessert and more would result in a sweet drink of punch. Authorities have noted that the ―bub‖ in syllabub ―was a medieval slang for a bubbly drink.‖ The usual ingredients in syllabub are cream, whipped egg whites, lemon juice, lemon zest, sugar, nutmeg and an alcohol (cider, wine or champagne). -

Transcription of 2664/3/1K Series Anne Talbot's Recipe Books Series
Transcription of 2664/3/1K Series Anne Talbot’s recipe books Series Introduction Table of Contents Transcription of 2664/3/1K Series Anne Talbot’s recipe books ........................................ 1 Series Introduction ............................................................................................................. 1 Introduction ....................................................................................................................... 2 The Collection ............................................................................................................................ 2 Documents in the Series / Introduction / Appendixes ................................................................ 2 Talbot Family ............................................................................................................................. 4 Sharington Talbot ......................................................................................................................................... 4 Sir Gilbert Talbot (c.1606 – 1695) ................................................................................................................. 4 Sir John Talbot (1630 – 1714) and Anne Talbot (1665 – 1720) ..................................................................... 4 Conventions used in the transcription ........................................................................................ 6 For example ................................................................................................................................................. -

GCSE RECIPE BOOK Term 1
GCSE RECIPE Student Group BOOK Teacher Target Grade Term 1 How to “Max Up” your skills! Basic level skills Medium level skills High level skills Assembling with shop Bought puff or filo pastry Skilled Pastry (Short bought ingredients Simple sauces (bolognaise, chilli) crust, pate Sucre, choux , This recipe book will be (e.g. bought meringues, Simple whisked desserts puff) bread, sauces Vegetable & fruit dishes requiring Roux based sauces used during your Basic desserts even sizes for appearance (béchamel, velouté) practical lessons as part Salads All in one sauces & batters (cheese Meringues and pavlovas Sandwiches sauce, custard, pancakes) Complex meat and fish of your GCSE course. Baked potato Simple cakes cookery (meat or fish is The recipes use the Blended soups Simple meat & fish cookery stuffed or a sauce is used) Simple starters Basic yeast dough Complex decorated cakes following symbols to Milk puddings Rich yeast dough show how difficult they Pasta & tortilla making Typical Simple fruit crumble Pies & pastry dishes using shop Apple / Lemon meringue are in terms of skill dishes Jacket potato with bought pastry pie, Bakewell / French cheese / beans Samosas, spring rolls, risotto apple tart, Millefuille levels. Pasta dishes using Shepherds / cottage pie Éclairs / profiteroles bought pasta & Pancakes Eton mess readymade sauces Stir fry, fruit salad & soups Quiche, meat or fish pie Sweet & sour using Blancmange, custard, rice pudding Lasagne, tagilatelle, readymade sauces Lasagne & cannelloni -

Türk Mutfağindaki Sütlü Tatlilarin Değerlendirilmesi Ve Inovasyonu
TÜRK MUTFAĞINDAKİ SÜTLÜ TATLILARIN DEĞERLENDİRİLMESİ VE İNOVASYONU Pamukkale Üniversitesi Sosyal Bilimler Enstitüsü Yüksek Lisans Tezi Gastronomi ve Mutfak Sanatları Ana Bilim Dalı Gastronomi ve Mutfak Sanatları Programı Raşit BAKAN Danışman: Prof. Dr. Nurten ÇEKAL Mart 2021 DENİZLİ Bu tezin tasarımı, hazırlanması, yürütülmesi, araştırmalarının yapılması ve bulgularının analizlerinde bilimsel etiğe ve akademik kurallara özenle riayet edildiğini; bu çalışmanın doğrudan birincil ürünü olmayan bulguların, verilerin ve materyallerin bilimsel etiğe uygun olarak kaynak gösterildiğini ve alıntı yapılan çalışmalara atıfta bulunulduğunu beyan ederim. İmza Raşit BAKAN i ÖNSÖZ Bu tez çalışması Pamukkale Üniversitesi Bilimsel Araştırma Projeleri Koordinasyon Birimi tarafından proje ile desteklenmiştir. Yüksek Lisans öğrenimim boyunca beni destekleyen ve akademik yardımlarını hiçbir zaman benden esirgemeyen, görüş ve düşünceleri ile beni yönlendiren, çalışmalarımı inceleyen değerli danışmanım Prof. Dr. Nurten ÇEKAL'a sonsuz teşekkürlerimi sunarım. Hayatımın her anında, maddi manevi her anlamda arkamda olduklarını bana hissettiren, hiçbir karşılık beklemeksizin bana sonsuz güvenen ve beni yetiştirmek için tüm gayretiyle gece gündüz demeden çalışan annem, babam ve ağabeyime sonsuz teşekkürler. Şimdiye kadar benim üzerimde emeği geçen ve bana destek olan tüm aile büyüklerime, ismini burada saymakla bitiremeyeceğim arkadaşlarıma ve öğretmenlerime teşekkürü de kendime bir borç bilirim. Çalışmamın tamamlanma süreci için değerli düşüncelerini ve manevi desteğini -

Product Information Baking Mixture
Product information Baking mixture - Instant pudding Article number: 301177 mix Powder – highly productive filling quantity: 1000 g Vanilla cream powder Blancmange without cooking! Description In powder for bakeable and freezeable dessert cream fillings. Instant blanc-mange is a soft basic cream for e. g. yeast cake, butter cream and blancmange desserts With our convenience products you buy professional high-quality products. The baking mixtures are produced of finest raw material in Germany. All products are easy to process, taste delicious and are always a success. In plastic can. With instructions and recipe suggestions. The item is excluded from the exchange. Manual Nutrition Facts Possible applications: For the production of a fast soft base cream for almond-coated Nutritional value per 100 g yeastcake, butter cream and blancmange desserts without cooking. For an angelcake cream physiological energy value 1666 kJ / filling mix whipped cream under the base cream. For a butter cream mix soft butter under the 371 kcal base cream. Blancmange recipes with cooked blancmange can be exchanged for this instant blancmange. fat 4.3 g hereof saturated fatty acids 2.5 g Basic recipe: For 500 ml water (milk, sour fruit juice or wine)weight out 175 g Instant carbohydrates 85.5 g blancmange. Stir the powder with the egg-whisk into the liquid strongly and let the blancmange hereof sugar 54.5 g rest for 5 minutes. Then process depending on recipe. Fibres 0.4 g For blancmange pretzel and Pastries with blancmange fillings: Mix 350 ml liquid with 150 g protein 3.3 g Instant Blancmange (yields 500 ml blancmange). -

Vegetarianism
LECTURE ON VEGETARIANISM. BY EMERITUS PROFESSOR F. W. NEWMAN. [Delivered at Gloucester, December 2, 1870; J/r. Price, M.P., in the Chair, and reprinted from the Dietetic Reformer, January, 1871.] LONDON: F. PITMAN, PATERNOSTER ROW. 1871. Price One Penny, or Five Shillings per Hundred. THE VEGETARIAN SOCIETY. ESTABLISHED A.D. 1847. $rmtant. J. Haughton, Esq., J.P., Dublin. i Vice^wsi&ents. W. G. Ward, Esq., Ross. i Professor Newman. i SrrasuiTf. John Davie, Esq., Dunfermline. P^onoratg Sewtsm. Mr. T. H. Barker, Manchester; Rev. James Clark, 126, Cross Lane, Salford. g>ecrctarg. Mr. R. Bailey Walker, 13, Cathedral Close, Manchester. SLocal specretanes, London................. Mr. G. Dornbusch, 11, Grove-street Road, South Hackney, N.E. Leeds.................... Mr. John Andrew, 14, Bishopgate-street. Glasgow................ Mr. J. Smith. Colchester .......... Mr. John Beach, Military Road. Dunfermline ...... Mr. J. Clark. Hull .............. Mr. T. D. Hardgrove, 1, Rutland Place. Perth.................... Mr. Henry MTntosh, 36, South Methven-street. Bury....................... Mr. William Hoyle, Tottington. Plymouth............. Mr. E. H. Poster, Homoeopathic Chemist. i Dublin................... Mr. J. A. Mowatt. I Bradford............. Miss M. A. Kellett, Paradise Green, Great Horton. Cardiff................. Mr. J. K. Collett. i ^Foreign CTonrsponlRng SwretariYs. I Mr. Emil Weilshaeuser, Neustadt, Silesia. Baboo Keshub Chunder Sen, Calcutta. Mr. Alfred von Seefeld, Hanover. Rev. Dr. Taylor, 349, North Ninth-street, Philadelphia. ' ipHE -
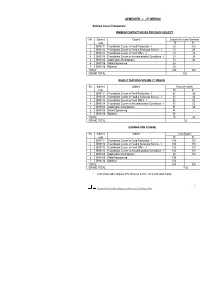
Semester - I (17 Weeks)
SEMESTER - I (17 WEEKS) National Council Component MINIMUM CONTACT HOURS FOR EACH SUBJECT No. Subject Subject Contact Hours per Semester code Th. Pr. 1 BHM111 Foundation Course in Food Production - I 30 120 2 BHM112 Foundation Course in Food & Beverage Service - I 30 60 3 BHM113 Foundation Course in Front Office - I 30 30 4 BHM114 Foundation Course in Accommodation Operations - I 30 30 5 BHM105 Application of Computers 15 60 6 BHM106 Hotel Engineering 60 - 7 BHM116 Nutrition 30 - TOTAL: 225 300 GRAND TOTAL 525 WEEKLY TEACHING SCHEME (17 WEEKS) No. Subject Subject Hours per week code Th. Pr. 1 BHM111 Foundation Course in Food Production - I 02 08 2 BHM112 Foundation Course in Food & Beverage Service - I 02 04 3 BHM113 Foundation Course in Front Office - I 02 02 4 BHM114 Foundation Course in Accommodation Operations - I 02 02 5 BHM105 Application of Computers 01 04 6 BHM106 Hotel Engineering 04 - 7 BHM116 Nutrition 02 - TOTAL: 15 20 GRAND TOTAL 35 EXAMINATION SCHEME No. Subject Subject Term Marks* code Th. Pr. 1 BHM111 Foundation Course in Food Production - I 100 100 2 BHM112 Foundation Course in Food & Beverage Service - I 100 100 3 BHM113 Foundation Course in Front Office - I 100 100 4 BHM114 Foundation Course in Accommodation Operations - I 100 100 5 BHM105 Application of Computers 50 100 6 BHM106 Hotel Engineering 100 - 7 BHM116 Nutrition 100 - TOTAL: 650 500 GRAND TOTAL 1150 * Term marks will comprise 30% Incourse & 70% Term end exam marks. 1 National Council for Hotel Management & Catering Technology, Noida . BHM111 - FOUNDATION COURSE IN FOOD PRODUCTION – I (THEORY) HOURS ALLOTED: 30 MAXIMUM MARKS: 100 S.No.