Renal Scintiscanning a Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

What a Difference a Delay Makes! CT Urogram: a Pictorial Essay
Abdominal Radiology (2019) 44:3919–3934 https://doi.org/10.1007/s00261-019-02086-0 SPECIAL SECTION : UROTHELIAL DISEASE What a diference a delay makes! CT urogram: a pictorial essay Abraham Noorbakhsh1 · Lejla Aganovic1,2 · Noushin Vahdat1,2 · Soudabeh Fazeli1 · Romy Chung1 · Fiona Cassidy1,2 Published online: 18 June 2019 © This is a U.S. Government work and not under copyright protection in the US; foreign copyright protection may apply 2019 Abstract Purpose The aim of this pictorial essay is to demonstrate several cases where the diagnosis would have been difcult or impossible without the excretory phase image of CT urography. Methods A brief discussion of CT urography technique and dose reduction is followed by several cases illustrating the utility of CT urography. Results CT urography has become the primary imaging modality for evaluation of hematuria, as well as in the staging and surveillance of urinary tract malignancies. CT urography includes a non-contrast phase and contrast-enhanced nephrographic and excretory (delayed) phases. While the three phases add to the diagnostic ability of CT urography, it also adds potential patient radiation dose. Several techniques including automatic exposure control, iterative reconstruction algorithms, higher noise tolerance, and split-bolus have been successfully used to mitigate dose. The excretory phase is timed such that the excreted contrast opacifes the urinary collecting system and allows for greater detection of flling defects or other abnormali- ties. Sixteen cases illustrating the utility of excretory phase imaging are reviewed. Conclusions Excretory phase imaging of CT urography can be an essential tool for detecting and appropriately characterizing urinary tract malignancies, renal papillary and medullary abnormalities, CT radiolucent stones, congenital abnormalities, certain chronic infammatory conditions, and perinephric collections. -

Urology Services in the ASC
Urology Services in the ASC Brad D. Lerner, MD, FACS, CASC Medical Director Summit ASC President of Chesapeake Urology Associates Chief of Urology Union Memorial Hospital Urologic Consultant NFL Baltimore Ravens Learning Objectives: Describe the numerous basic and advanced urology cases/lines of service that can be provided in an ASC setting Discuss various opportunities regarding clinical, operational and financial aspects of urology lines of service in an ASC setting Why Offer Urology Services in Your ASC? Majority of urologic surgical services are already outpatient Many urologic procedures are high volume, short duration and low cost Increasing emphasis on movement of site of service for surgical cases from hospitals and insurance carriers to ASCs There are still some case types where patients are traditionally admitted or placed in extended recovery status that can be converted to strictly outpatient status and would be suitable for an ASC Potential core of fee-for-service case types (microsurgery, aesthetics, prosthetics, etc.) Increasing Population of Those Aged 65 and Over As of 2018, it was estimated that there were 51 million persons aged 65 and over (15.63% of total population) By 2030, it is expected that there will be 72.1 million persons aged 65 and over National ASC Statistics - 2017 Urology cases represented 6% of total case mix for ASCs Urology cases were 4th in median net revenue per case (approximately $2,400) – behind Orthopedics, ENT and Podiatry Urology comprised 3% of single specialty ASCs (5th behind -

Native Kidney Biopsy
Mohammed E, et al., J Nephrol Renal Ther 2020, 6: 034 DOI: 10.24966/NRT-7313/100034 HSOA Journal of Nephrology & Renal Therapy Review Article Native Kidney Biopsy: An Introduction The burden of non communicable diseases has been a worldwide Update and Best Practice public health challenge, as chronic diseases compose 61% of global deaths and 49% of the global burden of diseases. Currently, many Evidence countries are encountering a fast transformation in the disease pro- file from first generation diseases such as infectious diseases to the encumbrance of non communicable diseases. In addition, Chronic Ehab Mohammed1, Issa Al Salmi1 *, Shilpa Ramaiah1 and Suad Hannawi2 Kidney Disease (CKD) is increasingly recognized as a global public health challenge as 10% of the global population is affected [1,2]. 1Nephrologist, The Renal Medicine Department, The Royal Hospital, Muscat, Oman The scarcity of well-trained renal pathologists, even in high-in- come countries, is a major obstacle to use of biopsy samples. The ISN 2Medicine Department, Ministry of Health and Prevention, Dubai, UAE is working worldwide to enhance development of local renal patholo- gy expertise. Levin et al stated that analysis of kidney biopsy samples can be used to stratify CKD into distinct subgroups of diseases based Abstract on specific histological patterns, when combined with the clinical pre- sentation [3]. Diabetes mellitus and hypertensive nephropathy are the Objectives: To Provide up-to-date guidelines for medical and nurs- commonly identified causes of End-Stage Kidney Disease (ESKD). ing staffs on the pre, during, and post care of a patient undergoing a Also, many patients with glomerulonephritis, systemic lupus erythe- percutaneous-kidney-biopsy-PKB. -
Laparoscopic Nephrectomy
Laparoscopic Nephrectomy Information for Patients This leaflet explains: What is a Nephrectomy? ............................................................................................. 2 Why do I need a nephrectomy? ................................................................................... 3 What are the risks and side effects of laparoscopic nephrectomy? ............................. 3 Occasional risks ....................................................................................................... 3 Rare risks ................................................................................................................. 3 Very Rare Risks ....................................................................................................... 3 Before the operation .................................................................................................... 4 Day of your operation .................................................................................................. 4 How long will the operation take? ................................................................................ 4 After the operation ....................................................................................................... 4 Going home ................................................................................................................. 5 At home ....................................................................................................................... 5 Contacts ..................................................................................................................... -

Percutaneous Ultrasound-Guided Renal Biopsy; a Comparison of Axial Vs
Percutaneous ultrasound-guided renal biopsy; A comparison of axial vs. sagittal probe location FARNAZ SHAMSHIRGAR1, SEYED MORTEZA BAGHERI2* 1Resident of Radiology, Iran University of Medical Sciences, Tehran, Iran 2Department of Radiology, Hasheminejad Kidney Center (HKC), Iran University of Medical Sciences, Tehran, Iran Background. Renal biopsy is an important method for diagnosis of renal parenchymal abnormalities. Here, we compare the effectiveness and complications of percutaneous ultrasound- guided renal biopsy using axial vs. sagittal probe locations. Methods. In a cross-sectional survey, in 2012, patients with a nephrologist order were biopsied by a radiology resident. Renal biopsy was done on 15 patients using axial (A group) and the same number of biopsies done with sagittal probe location (S group). The two groups were compared in term of the yields and complications of each method. Results. In the A group, the ratio of glomeruli gathered to the number of obtained samples was significantly higher than in the S group. Nine patients in the A group (60%) required only two samplings, whereas 66.7% in the S group required more than two attempts. Microscopic hematuria was more common in the A; conversely, gross hematuria was less common in the A group. Meagre hematomas were more frequent in the S group .When compared with hemoglobin level before biopsy, its level 24 hours after biopsy was similar within groups. Conclusion. Our study shows that percutaneous ultrasound-guided renal biopsy using axial probe provides better yield with fewer efforts and fewer serious complications. Keywords: Percutaneous renal biopsy, Ultrasound-guided renal biopsy, Ultra-sonography probe location. INTRODUCTION plications and related post therapeutic side effects may cause another complication such as vascular Percutaneous renal biopsy is an important occlusion, acute obstruction of renal output, renal method to diagnose most kidney diseases. -

Renal Scan Prior to Renal Biopsy—
RENAL SCAN PRIOR TO RENAL BIOPSY— A METHOD OF RENAL LOCALIZATION Richard J. Tully, Violet J. Stark, Paul B. Hoffer, and Alexander Gottschalk University of Chicago Hospitals and Clinics, and the A rgonne Cancer Research Hospital, Chicago, Illinois Palpation, percussion, and auscultation are the a generally lower radiation dose to the patient than classical methods of determining organ localization the radiographie procedures. One such technique— by external nontraumatic means. With the need for renal localization prior to renal biopsy—has become more specific information about smaller organs, espe routine at our institution in the last 6 years. cially for needle biopsy or aspiration techniques, more definitive localization of these organs has be METHODS come necessary. The anatomic landmarks used in In our method (7) the patient is given an injection most biopsy techniques are simply not specific of 1.0 mCi of Tc-Fe-ascorbic acid complex and enough to cover individual variation. This has led about 1 hr later is positioned under the gamma cam- to the development of many radiographie procedures and more recently to the use of radionuclide dis Received Oct. 28, 1971; revision accepted Mar. 2, 1972. tribution or ultrasonography for localization. The For reprints contact: Richard J. Tully, University of Chicago, Dept. of Radiology, 950 E. 59 St., Chicago, 111. latter procedures are desirable because they deliver 60637. FIG. 1. A shows patient positioned under camera 1 hr after injection of 0.1 mCi Tc-Fe-ascorbic acid complex in "bi opsy position". B shows small point sources ("Co) positioned on patient's back until they coincide with scan image of renal out line by trial and error method or with use of persistence oscilloscope. -

Pyelography in Infants
Arch Dis Child: first published as 10.1136/adc.9.50.119 on 1 April 1934. Downloaded from PYELOGRAPHY IN INFANTS BY W. E. UNDERWOOD, F.R.C.S., Chief Assistant to a Surgical Unit, St. Bartholomew's Hospital. Pyelography in infants is an examination which is essential under certain circumstances, and from it valuable facts may often be obtained which would be undiscovered without this specialized form of investigation. Hitherto the examination has been surrounded by difficulties of such a nature that it is often unsuccessful and the child is submitted to discomfort without result. The object of this paper is to bring forward certain notes on cases where pyelography has been indicated. The observations from a series of sixteen cases have led to the development of a method whereby good pyelograms have been obtained with certainty. Instrumental pyelography in infancy is a procedure not to be advised lightheartedly, but there are occasions where the indications are definite and adequate: in these cases the anticipation of possible information to be gained justifies submitting the infants to what constitutes a major examination. In this series are cases of urinary infection resistant to the usual medical treatment, of renal pain, of renal calculi, and cases of congenital malformation http://adc.bmj.com/ of the urinary tract similar to those described by Poynton and Sheldon'. The term pyelography is used here for brevity rather than accuracy, for it embraces a complete investigation of the urinary tract, including ureterography. Methods of pyelography.-The choice lies between intravenous and on September 30, 2021 by guest. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Development of the ICD-10 Procedure Coding System (ICD-10-PCS)
Development of the ICD-10 Procedure Coding System (ICD-10-PCS) Richard F. Averill, M.S., Robert L. Mullin, M.D., Barbara A. Steinbeck, RHIT, Norbert I. Goldfield, M.D, Thelma M. Grant, RHIA, Rhonda R. Butler, CCS, CCS-P The International Classification of Diseases 10th Revision Procedure Coding System (ICD-10-PCS) has been developed as a replacement for Volume 3 of the International Classification of Diseases 9th Revision (ICD-9-CM). The development of ICD-10-PCS was funded by the U.S. Centers for Medicare and Medicaid Services (CMS).1 ICD-10- PCS has a multiaxial seven character alphanumeric code structure that provides a unique code for all substantially different procedures, and allows new procedures to be easily incorporated as new codes. ICD10-PCS was under development for over five years. The initial draft was formally tested and evaluated by an independent contractor; the final version was released in the Spring of 1998, with annual updates since the final release. The design, development and testing of ICD-10-PCS are discussed. Introduction Volume 3 of the International Classification of Diseases 9th Revision Clinical Modification (ICD-9-CM) has been used in the U.S. for the reporting of inpatient pro- cedures since 1979. The structure of Volume 3 of ICD-9-CM has not allowed new procedures associated with rapidly changing technology to be effectively incorporated as new codes. As a result, in 1992 the U.S. Centers for Medicare and Medicaid Services (CMS) funded a project to design a replacement for Volume 3 of ICD-9-CM. -

Post-Percutaneous Renal Biopsy Observation Time; Single Center Experience
Open Access Austin Journal of Nephrology and Hypertension Special Article - Chronic Kidney Disease Post-Percutaneous Renal Biopsy Observation Time; Single Center Experience Habas E1*, Elhabash B2, Rayani A3, Turgman F4 and Tarsien R2 Abstract 1 Department of Internal Medicine, Tripoli Central Background: Percutaneous Renal Biopsy (PRB) should be performed Hospital, Libya to diagnose renal damage, to assess response to treatment and to predict 2Department of Rheumatology, Tripoli Medical Center, prognosis.PRB is a safer procedure and mostly free of complications. Assessing Libya optimal time duration post-PRB is important to predict Post-PRB complication 3Department of Pediatrics, Tripoli Children Hospital, and to reduce the cost of PRB. Pediatric Arab Board, Libya 4Pathologist, Tripoli Central Hospital, University of Aim: To reduce the Post-PRB observation time for optimal outcome and Tripoli, Libya patient’s safety. *Corresponding author: Elmukhtar Habas, Methods: All PRBs were performed at the Nephrology Unit, Tripoli Department of Internal Medicine, Tripoli Central Central Hospital, Libya between May 2008 to December 2015. One hundred Hospital, Facharzt Nephrology, Libya eighteen ultrasound-guided PRBs were done. After explaining the procedure and its possible complications, an informed consent was signed by patients. Received: July 01, 2016; Accepted: August 23, 2016; Coagulation profile PT, PTT, INR, BT, CT and CBC were done before PRB. Published: August 25, 2016 Each biopsy was performed with an automated biopsy gun with a 16 -gauge needle under real-time US. Two biopsy specimens from lower pole of left kidney were taken from native kidneys. All patients were kept under close medical supervision and on bed rest for 2-hours. -
Extraction of Kidney Via Suprapubic Or Inguinal Incision in Total Laparoscopic Donor Nephrectomy
LESS Original Article Laparosc Endosc Surg Sci 2019;26(1):15-18 DOI: 10.14744/less.2019.69772 Extraction of kidney via suprapubic or inguinal incision in total laparoscopic donor nephrectomy 1 1 2 1 Fatih Sümer, Ersin Gündoğan, Neslihan Altunkaya, Mehmet Can Aydın, 1 1 1 1 Sertaç Usta, Sait Murat Doğan, Turgut Pişkin, Cüneyt Kayaalp 1Department of General Surgery, Inönü University Faculty of Medicine, Malatya, Turkey 2Department of Anesthesia, Inonu University Faculty of Medicine, Malatya, Turkey ABSTRACT Introduction: The objective of this study was to investigate the results of the first 48 patients who underwent total laparoscopic transperitoneal donor nephrectomy at a single institution and to present the impact of the kidney extraction site on ischemia time. Materials and Methods: The study included patients who underwent kidney donor surgery between February 2017 and December 2018. Evaluation of the kidney transplantation candidates was performed by the kidney transplantation council. A total of 4 trocars were used for a right-side nephrectomy, and 3 trocars were used for a left-side nephrectomy. The kidneys were extracted through a suprapubic incision in the first 18 cases and through the inguinal region in the last 30 cases. A comparison was made of the demographic charac- teristics and the intraoperative and postoperative results of the 2 groups. Results: Of the study patients, 30 were female and 18 were male, with a mean age of 48.0±9.6 years (range: 30–71 years). All of the patients underwent a total laparoscopic transperitoneal donor nephrectomy. Four patients underwent a right-side nephrectomy and 44 underwent a left-side nephrectomy. -
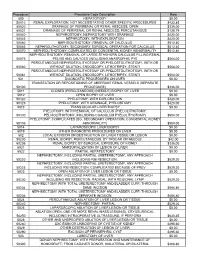
Procedure Procedure Code Description Rate 500
Procedure Procedure Code Description Rate 500 HEPATOTOMY $0.00 50010 RENAL EXPLORATION, NOT NECESSITATING OTHER SPECIFIC PROCEDURES $433.85 50020 DRAINAGE OF PERIRENAL OR RENAL ABSCESS; OPEN $336.00 50021 DRAINAGE OF PERIRENAL OR RENAL ABSCESS; PERCUTANIOUS $128.79 50040 NEPHROSTOMY, NEPHROTOMY WITH DRAINAGE $420.00 50045 NEPHROTOMY, WITH EXPLORATION $420.00 50060 NEPHROLITHOTOMY; REMOVAL OF CALCULUS $512.40 50065 NEPHROLITHOTOMY; SECONDARY SURGICAL OPERATION FOR CALCULUS $512.40 50070 NEPHROLITHOTOMY; COMPLICATED BY CONGENITAL KIDNEY ABNORMALITY $512.40 NEPHROLITHOTOMY; REMOVAL OF LARGE STAGHORN CALCULUS FILLING RENAL 50075 PELVIS AND CALYCES (INCLUDING ANATROPHIC PYE $504.00 PERCUTANEOUS NEPHROSTOLITHOTOMY OR PYELOSTOLITHOTOMY, WITH OR 50080 WITHOUT DILATION, ENDOSCOPY, LITHOTRIPSY, STENTI $504.00 PERCUTANEOUS NEPHROSTOLITHOTOMY OR PYELOSTOLITHOTOMY, WITH OR 50081 WITHOUT DILATION, ENDOSCOPY, LITHOTRIPSY, STENTI $504.00 501 DIAGNOSTIC PROCEDURES ON LIVER $0.00 TRANSECTION OR REPOSITIONING OF ABERRANT RENAL VESSELS (SEPARATE 50100 PROCEDURE) $336.00 5011 CLOSED (PERCUTANEOUS) (NEEDLE) BIOPSY OF LIVER $0.00 5012 OPEN BIOPSY OF LIVER $0.00 50120 PYELOTOMY; WITH EXPLORATION $420.00 50125 PYELOTOMY; WITH DRAINAGE, PYELOSTOMY $420.00 5013 TRANSJUGULAR LIVER BIOPSY $0.00 PYELOTOMY; WITH REMOVAL OF CALCULUS (PYELOLITHOTOMY, 50130 PELVIOLITHOTOMY, INCLUDING COAGULUM PYELOLITHOTOMY) $504.00 PYELOTOMY; COMPLICATED (EG, SECONDARY OPERATION, CONGENITAL KIDNEY 50135 ABNORMALITY) $504.00 5014 LAPAROSCOPIC LIVER BIOPSY $0.00 5019 OTHER DIAGNOSTIC PROCEDURES