2021 Billing and Coding Guide Urology Surgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Urological Trauma
Guidelines on Urological Trauma D. Lynch, L. Martinez-Piñeiro, E. Plas, E. Serafetinidis, L. Turkeri, R. Santucci, M. Hohenfellner © European Association of Urology 2007 TABLE OF CONTENTS PAGE 1. RENAL TRAUMA 5 1.1 Background 5 1.2 Mode of injury 5 1.2.1 Injury classification 5 1.3 Diagnosis: initial emergency assessment 6 1.3.1 History and physical examination 6 1.3.1.1 Guidelines on history and physical examination 7 1.3.2 Laboratory evaluation 7 1.3.2.1 Guidelines on laboratory evaluation 7 1.3.3 Imaging: criteria for radiographic assessment in adults 7 1.3.3.1 Ultrasonography 7 1.3.3.2 Standard intravenous pyelography (IVP) 8 1.3.3.3 One shot intraoperative intravenous pyelography (IVP) 8 1.3.3.4 Computed tomography (CT) 8 1.3.3.5 Magnetic resonance imaging (MRI) 9 1.3.3.6 Angiography 9 1.3.3.7 Radionuclide scans 9 1.3.3.8 Guidelines on radiographic assessment 9 1.4 Treatment 10 1.4.1 Indications for renal exploration 10 1.4.2 Operative findings and reconstruction 10 1.4.3 Non-operative management of renal injuries 11 1.4.4 Guidelines on management of renal trauma 11 1.4.5 Post-operative care and follow-up 11 1.4.5.1 Guidelines on post-operative management and follow-up 12 1.4.6 Complications 12 1.4.6.1 Guidelines on management of complications 12 1.4.7 Paediatric renal trauma 12 1.4.7.1 Guidelines on management of paediatric trauma 13 1.4.8 Renal injury in the polytrauma patient 13 1.4.8.1 Guidelines on management of polytrauma with associated renal injury 14 1.5 Suggestions for future research studies 14 1.6 Algorithms 14 1.7 References 17 2. -

What a Difference a Delay Makes! CT Urogram: a Pictorial Essay
Abdominal Radiology (2019) 44:3919–3934 https://doi.org/10.1007/s00261-019-02086-0 SPECIAL SECTION : UROTHELIAL DISEASE What a diference a delay makes! CT urogram: a pictorial essay Abraham Noorbakhsh1 · Lejla Aganovic1,2 · Noushin Vahdat1,2 · Soudabeh Fazeli1 · Romy Chung1 · Fiona Cassidy1,2 Published online: 18 June 2019 © This is a U.S. Government work and not under copyright protection in the US; foreign copyright protection may apply 2019 Abstract Purpose The aim of this pictorial essay is to demonstrate several cases where the diagnosis would have been difcult or impossible without the excretory phase image of CT urography. Methods A brief discussion of CT urography technique and dose reduction is followed by several cases illustrating the utility of CT urography. Results CT urography has become the primary imaging modality for evaluation of hematuria, as well as in the staging and surveillance of urinary tract malignancies. CT urography includes a non-contrast phase and contrast-enhanced nephrographic and excretory (delayed) phases. While the three phases add to the diagnostic ability of CT urography, it also adds potential patient radiation dose. Several techniques including automatic exposure control, iterative reconstruction algorithms, higher noise tolerance, and split-bolus have been successfully used to mitigate dose. The excretory phase is timed such that the excreted contrast opacifes the urinary collecting system and allows for greater detection of flling defects or other abnormali- ties. Sixteen cases illustrating the utility of excretory phase imaging are reviewed. Conclusions Excretory phase imaging of CT urography can be an essential tool for detecting and appropriately characterizing urinary tract malignancies, renal papillary and medullary abnormalities, CT radiolucent stones, congenital abnormalities, certain chronic infammatory conditions, and perinephric collections. -

Urology Services in the ASC
Urology Services in the ASC Brad D. Lerner, MD, FACS, CASC Medical Director Summit ASC President of Chesapeake Urology Associates Chief of Urology Union Memorial Hospital Urologic Consultant NFL Baltimore Ravens Learning Objectives: Describe the numerous basic and advanced urology cases/lines of service that can be provided in an ASC setting Discuss various opportunities regarding clinical, operational and financial aspects of urology lines of service in an ASC setting Why Offer Urology Services in Your ASC? Majority of urologic surgical services are already outpatient Many urologic procedures are high volume, short duration and low cost Increasing emphasis on movement of site of service for surgical cases from hospitals and insurance carriers to ASCs There are still some case types where patients are traditionally admitted or placed in extended recovery status that can be converted to strictly outpatient status and would be suitable for an ASC Potential core of fee-for-service case types (microsurgery, aesthetics, prosthetics, etc.) Increasing Population of Those Aged 65 and Over As of 2018, it was estimated that there were 51 million persons aged 65 and over (15.63% of total population) By 2030, it is expected that there will be 72.1 million persons aged 65 and over National ASC Statistics - 2017 Urology cases represented 6% of total case mix for ASCs Urology cases were 4th in median net revenue per case (approximately $2,400) – behind Orthopedics, ENT and Podiatry Urology comprised 3% of single specialty ASCs (5th behind -
Thromboprophylaxis in Urological Surgery
EAU Guidelines on Thromboprophylaxis in Urological Surgery K.A.O. Tikkinen (Chair), R. Cartwright, M.K. Gould, R. Naspro, G. Novara, P.M. Sandset, P. D . Violette, G.H. Guyatt © European Association of Urology 2018 TABLE OF CONTENTS PAGE 1. INTRODUCTION 3 1.1 Aims and objectives 3 1.2 Panel composition 3 1.3 Available publications 3 1.4 Publication history 3 2. METHODS 3 2.1 Guideline methodology 3 3. GUIDELINE 4 3.1 Thromboprophylaxis post-surgery 4 3.1.1 Introduction 4 3.1.2 Outcomes and definitions 4 3.1.3 Timing and duration of thromboprophylaxis 4 3.1.4 Basic principles for recommending (or not recommending) post-surgery thromboprophylaxis 5 3.1.4.1 Effect of prophylaxis on key outcomes 5 3.1.4.2 Baseline risk of key outcomes 5 3.1.4.3 Patient-related risk (and protective) factors 5 3.1.4.4 From evidence to recommendations 6 3.1.5 General statements for all procedure-specific recommendations 7 3.1.6 Recommendations 7 3.2 Peri-operative management of antithrombotic agents in urology 14 3.2.1 Introduction 14 3.2.2 Evidence summary 14 3.2.3 Recommendations 14 4. RESEARCH RECOMMENDATIONS 16 5. REFERENCES 16 6. CONFLICT OF INTEREST 18 7. ACKNOWLEDGEMENTS 18 8. CITATION INFORMATION 18 2 THROMBOPROPHYLAXIS - MARCH 2017 1. INTRODUCTION 1.1 Aims and objectives Due to the hypercoagulable state induced by surgery, serious complications of urological surgery include deep vein thrombosis (DVT) and pulmonary embolism (PE) - together referred to as venous thromboembolism (VTE) - and major bleeding [1-4]. -
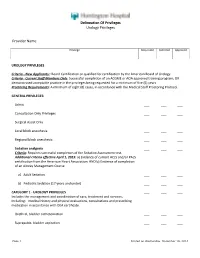
Delineation of Privileges Urology Privileges Provider Name
Delineation Of Privileges Urology Privileges Provider Name: Privilege Requested Deferred Approved UROLOGY PRIVILEGES Criteria - New Applicants:: Board Certification or qualified for certification by the American Board of Urology. Criteria - Current Staff Members Only: Successful completion of an ACGME or AOA approved training program; OR demonstrated acceptable practice in the privileges being requested for a minimum of five (5) years. Proctoring Requirements: A minimum of eight (8) cases, in accordance with the Medical Staff Proctoring Protocol. GENERAL PRIVILEGES: Admit ___ ___ ___ Consultation Only Privileges ___ ___ ___ Surgical Assist Only ___ ___ ___ Local block anesthesia ___ ___ ___ Regional block anesthesia ___ ___ ___ Sedation analgesia ___ ___ ___ Criteria: Requires successful completion of the Sedation Assessment test. Additional criteria effective April 1, 2015: a) Evidence of current ACLS and/or PALS certification from the American Heart Association; AND b) Evidence of completion of an Airway Management Course a) Adult Sedation ___ ___ ___ b) Pediatric Sedation (17 years and under) ___ ___ ___ CATEGORY 1 - UROLOGY PRIVILEGES ___ ___ ___ Includes the management and coordination of care, treatment and services, including: medical history and physical evaluations, consultations and prescribing medication in accordance with DEA certificate. Urethral, bladder catheterization ___ ___ ___ Suprapubic, bladder aspiration ___ ___ ___ Page 1 Printed on Wednesday, December 10, 2014 Delineation Of Privileges Urology Privileges Provider -

Effective Endoscopic Holmium Laser Lithotripsy in the Treatment of a Large
Cases and Techniques Library (CTL) E485 The patient was discharged after 15 days with complete resolution of the occlusive Effective endoscopic holmium laser lithotripsy symptoms, and her scheduled chole- in the treatment of a large impacted gallstone cystectomy was canceled. in the duodenum Endoscopy_UCTN_Code_CCL_1AZ_2AD Competing interests: None Fig. 1 Computed tomographic scan shows a large calcified Vincenzo Mirante, Helga Bertani, ring (stone) in the Giuseppe Grande, Mauro Manno, duodenum of an Angelo Caruso, Santi Mangiafico, 87-year-old woman Rita Conigliaro presenting with ab- U.O.C. Gastroenterology and Digestive dominal pain and vomiting of 3 days’ Endoscopy Unit, Nuovo Ospedale Civile duration. Sant'Agostino Estense, Modena, Italy References 1 Reisner RM, Cohen JR. Gallstone ileus: a re- view of 1001 reported cases. Am Surg 1994; 60: 441–446 2 Rodriguez H, Codina C, Girones V et al. Gall- stone ileus: results of analysis of a series of Gallstone ileus is caused by the passage To fragment the stone, we performed an- 40 patients. Gastroenterol Hepatol 2001; – of one or more large gallstones (at least other endoscopic procedure. A holmium 24: 489 494 3 Rigler LG, Borman CN, Noble JF. Gallstone ob- 2.5 cm in size) in the gastrointestinal tract laser (HLS30W Holmium:YAG 30W Laser; struction: pathogenesis and roentgen mani- through a bilioenteric fistula. It accounts Olympus America, Center Valley, Penn- festations. JAMA 1941; 117: 1753 –1759 for 1 % to 4% of all cases of mechanical sylvania, USA) was applied for a total of 4 Goldstein EB, Savel RH, Pachter HL et al. Suc- small-bowel obstruction [1,2]. -

A Systematic Review of Graft Augmentation Urethroplasty Techniques for the Treatment of Anterior Urethral Strictures
EUROPEAN UROLOGY 59 (2011) 797–814 available at www.sciencedirect.com journal homepage: www.europeanurology.com Review – Reconstructive Urology A Systematic Review of Graft Augmentation Urethroplasty Techniques for the Treatment of Anterior Urethral Strictures Altaf Mangera *, Jacob M. Patterson, Christopher R. Chapple Royal Hallamshire Hospital, Sheffield, United Kingdom Article info Abstract Article history: Context: Reconstructive surgeons who perform urethroplasty have a variety of Accepted February 2, 2011 techniques in their armamentarium that may be used according to factors such as Published online ahead of aetiology, stricture position, and length. No one technique is recommended. print on February 11, 2011 Objective: Our aim was to assess the reported outcomes of the various techniques for graft augmentation urethroplasty according to site of surgery. Keywords: Evidence acquisition: We performed an updated systematic review of the Medline Augmentation urethroplasty literature from 1985 to date and classified the data according to the site of surgery Anterior urethral stricture and technique used. Data are also presented on the type of graft used and the Bulbar urethroplasty follow-up methodology used by each centre. Dorsal onlay bulbar Evidence synthesis: More than 2000 anterior urethroplasty procedures have been urethroplasty describedinthe literature.Whenconsidering the bulbar urethra there isnosignificant Ventral onlay bulbar difference between the average success rates of the dorsal and the ventral onlay urethroplasty procedures, 88.4% and 88.8% at42.2 and 34.4 moin 934 and 563 patients,respectively. Penile urethroplasty The lateral onlay technique has only been described in six patients and has a reported success rate of 83% at 77 mo. The Asopa and Palminteri techniques have been described in 89 and 53 patients with a success rate of 86.7% and 90.1% at 28.9 and 21.9 mo, respectively. -

Quality of Life Outcomes After Brachytherapy for Early Prostate Cancer
Prostate Cancer and Prostatic Diseases (1999) 2 Suppl 3, S19±S20 ß 1999 Stockton Press All rights reserved 1365±7852/99 $15.00 http://www.stockton-press.co.uk/pcan Quality of life outcomes after brachytherapy for early prostate cancer MS Litwin1, JM Brandeis1, CM Burnison1 and E Reiter1 1UCLA Departments of Urology, Health Services, and Radiation Oncology, UCLA, California, USA Despite the absence of empirical evidence, there is a XRT. Sildena®l appeared to have little effect in the radical popular perception that brachytherapy results in less prostatectomy patients. However, brachytherapy patients impairment of health-related quality of life. This study not receiving hormonal ablation or XRT who took silde- compared general and disease-speci®c health-related na®l had better sexual function and bother scores than quality of life in men who had undergone either brachy- those patients who did not. therapy (with and without pre-treatment XRT) or radical prostatectomy, and in healthy age-matched controls. Method Conclusion We surveyed all patients with clinical T2 or less prostate General health-related quality of life did not differ greatly cancer who had undergone interstitial seed brachyther- between the three groups, but there were variations in apy at UCLA during the previous 3±17 months. Each was disease-speci®c (urinary, bowel and sexual) health-related paired with two randomly selected, temporally matched quality of life. Radical prostatectomy patients had the radical prostatectomy patients. Healthy, age-matched worst urinary function (leakage), but brachytherapy controls were drawn from the literature. Surgery and patients were also signi®cantly worse than the controls. -

Cystectomy and Neo Bladder Surgery
Form: D-5379 Cystectomy and Neo Bladder Surgery A guide for patients and families Reading this booklet can help you prepare for your surgery, hospital stay and recovery after surgery. We encourage you to take an active role in your care. If you have any questions, please ask a member of your health care team. Inside this booklet page Learning about your surgery ...................................................3 Preparing for surgery ...............................................................5 Your hospital stay ......................................................................9 Getting ready to leave the hospital .........................................17 Your recovery after surgery .....................................................19 Who to call if you have questions ............................................29 When to get medical help ........................................................30 2 Learning about your surgery What is a Cystectomy? Cystectomy is surgery to remove your bladder. This is usually done to control bladder cancer. Depending on the extent of the cancer, the bladder and some surrounding organs may need to be removed. • The prostate gland, seminal vesicles and nerve bundles may also be removed. • The ovaries, fallopian tubes, uterus, cervix and part of the vagina may also be removed. What is a Neo Bladder? Words to know A neo bladder is a pouch made from a Neo means new. piece of your bowel that is placed where A neo bladder is a new bladder. your bladder was removed. A neo bladder is commonly called a pouch, because a piece The pouch acts like a bladder, collecting of your bowel is made into a urine that comes down the ureters from pouch that can store urine. the kidneys. When you pass urine, it The medical name for this is a leaves the pouch through your urethra. -

Prostate Biopsy in the Staging of Prostate Cancer
Prostate Cancer and Prostatic Diseases (1997) 1, 54±58 ß 1997 Stockton Press All rights reserved 1365±7852/97 $12.00 Review Prostate Biopsy in the staging of prostate cancer L Salomon, M Colombel, J-J Patard, D Gasman, D Chopin & C-C Abbou Service d'Urologie, CHU, Henri Mondor, CreÂteil, France The use of prostate biopsies was developed in parallel with progress in our knowledge of prostate cancer and the use of prostate-speci®c antigen (PSA). Prostate biopsies were initially indicated for the diagnosis of cancer, by the perineal approach under general anesthesia. Nowadays prostate biopsies are not only for diagnostic purposes but also to determine the prognosis, particularly before radical prostatectomy. They are performed in patients with elevated PSA levels, by the endorectal approach, sometimes under local anesthesia.(1±3) The gold standard is the sextant biopsy technique described by Hodge4,5, which is best to diagnose prostate cancer, particularly in case of T1c disease (patients with serum PSA elevation).6±13 Patients with a strong suspicion of prostate cancer from a negative series of biopsies can undergo a second series14;15 with transition zone biopsy16,17 or lateral biopsy.18,19 Karakiewicz et al 20 and Uzzo et al 21 proposed that the number of prostate biopsies should depend on prostate volume to improve the positivity rate. After the diagnosis of prostate cancer, initial therapy will depend on several prognostic factors. In the case of radical prostatectomy, the results of sextant biopsy provide a wealth of information.22,23 The aim of this report is to present the information given by prostate biopsy in the staging of prostate cancer. -

Comparison of Postoperative Renal Function Between Non-Steroidal
Journal of Clinical Medicine Article Comparison of Postoperative Renal Function between Non-Steroidal Anti-Inflammatory Drug and Opioids for Patient-Controlled Analgesia after Laparoscopic Nephrectomy: A Retrospective Cohort Study Jiwon Han 1 , Young-Tae Jeon 1,2, Ah-Young Oh 1,2 , Chang-Hoon Koo 1, Yu Kyung Bae 1 and Jung-Hee Ryu 1,2,* 1 Department of Anesthesiology and Pain Medicine, Seoul National University Bundang Hospital, 82, Gumi-ro, Bundang-gu, Seongnam-si, Gyeonggi-do 13620, Korea; [email protected] (J.H.); [email protected] (Y.-T.J.); [email protected] (A.-Y.O.); [email protected] (C.-H.K.); [email protected] (Y.K.B.) 2 Department of Anesthesiology and Pain Medicine, Seoul National University College of Medicine, 103, Daehak-ro, Jongno-gu, Seoul 03080, Korea * Correspondence: [email protected]; Tel.: +82-31-787-7497 Received: 7 August 2020; Accepted: 9 September 2020; Published: 13 September 2020 Abstract: Non-steroidal anti-inflammatory drugs (NSAIDs) can be used as opioid alternatives for patient-controlled analgesia (PCA). However, their use after nephrectomy has raised concerns regarding possible nephrotoxicity. This study compared postoperative renal function and postoperative outcomes between patients using NSAID and patients using opioids for PCA in nephrectomy. In this retrospective observational study, records were reviewed for 913 patients who underwent laparoscopic or robot-assisted laparoscopic nephrectomy from 2015 to 2017. After propensity score matching, 247 patients per group were analyzed. Glomerular filtration rate (GFR) percentages (postoperative value divided by preoperative value), blood urea nitrogen (BUN)/creatinine ratios, and serum creatinine percentages were compared at 2 weeks, 6 months, and 1 year after surgery between users of NSAID and users of opioids for PCA. -
Laparoscopic Nephrectomy
Laparoscopic Nephrectomy Information for Patients This leaflet explains: What is a Nephrectomy? ............................................................................................. 2 Why do I need a nephrectomy? ................................................................................... 3 What are the risks and side effects of laparoscopic nephrectomy? ............................. 3 Occasional risks ....................................................................................................... 3 Rare risks ................................................................................................................. 3 Very Rare Risks ....................................................................................................... 3 Before the operation .................................................................................................... 4 Day of your operation .................................................................................................. 4 How long will the operation take? ................................................................................ 4 After the operation ....................................................................................................... 4 Going home ................................................................................................................. 5 At home ....................................................................................................................... 5 Contacts .....................................................................................................................