Certain Conditions Originating in the Perinatal Period (760 – 779.9)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hypocalcemia Associated with Subcutaneous Fat Necrosis of the Newborn: Case Report and Literature Review Alphonsus N
case report Oman Medical Journal [2017], Vol. 32, No. 6: Hypocalcemia Associated with Subcutaneous Fat Necrosis of the Newborn: Case Report and Literature Review Alphonsus N. Onyiriuka 1* and Theodora E. Utomi2 1Endocrine and Metabolic Unit, Department of Child Health, University of Benin Teaching Hospital, Benin City, Nigeria 2Special Care Baby Unit, Department of Nursing Services, St Philomena Catholic Hospital, Benin City, Nigeria ARTICLE INFO ABSTRACT Article history: Subcutaneous fat necrosis of the newborn (SCFNN) is a rare benign inflammatory Received: 4 November 2015 disorder of the adipose tissue but may be complicated by hypercalcemia or less frequently, Accepted: 21 October 2016 hypocalcemia, resulting in morbidity and mortality. Here we report the case of a neonate Online: with subcutaneous fat necrosis who surprisingly developed hypocalcemia instead DOI 10.5001/omj.2017.99 of hypercalcemia. A full-term female neonate was delivered by emergency cesarean section for fetal distress and was subsequently admitted to the Special Care Baby Keywords: Hypocalcemia; Infant, Unit. The mother’s pregnancy was uncomplicated up to delivery. Her anthropometric Newborn; Subcutaneous Fat measurements were birth weight 4.1 kg (95th percentile), length 50 cm (50th percentile), Necrosis; Perinatal Stress. and head circumference 34.5 cm (50th percentile). The Apgar scores were 2, 3, and 8 at 1, 5, 10 minutes, respectively. There was no abnormal facies and she was fed with breast milk only. On the seventh day of life, the infant was found to have multiple nodules located in the neck, upper back, and right arm. The nodules were firm, well circumscribed with no evidence of tenderness. -

N35.12 Postinfective Urethral Stricture, NEC, Female N35.811 Other
N35.12 Postinfective urethral stricture, NEC, female N35.811 Other urethral stricture, male, meatal N35.812 Other urethral bulbous stricture, male N35.813 Other membranous urethral stricture, male N35.814 Other anterior urethral stricture, male, anterior N35.816 Other urethral stricture, male, overlapping sites N35.819 Other urethral stricture, male, unspecified site N35.82 Other urethral stricture, female N35.911 Unspecified urethral stricture, male, meatal N35.912 Unspecified bulbous urethral stricture, male N35.913 Unspecified membranous urethral stricture, male N35.914 Unspecified anterior urethral stricture, male N35.916 Unspecified urethral stricture, male, overlapping sites N35.919 Unspecified urethral stricture, male, unspecified site N35.92 Unspecified urethral stricture, female N36.0 Urethral fistula N36.1 Urethral diverticulum N36.2 Urethral caruncle N36.41 Hypermobility of urethra N36.42 Intrinsic sphincter deficiency (ISD) N36.43 Combined hypermobility of urethra and intrns sphincter defic N36.44 Muscular disorders of urethra N36.5 Urethral false passage N36.8 Other specified disorders of urethra N36.9 Urethral disorder, unspecified N37 Urethral disorders in diseases classified elsewhere N39.0 Urinary tract infection, site not specified N39.3 Stress incontinence (female) (male) N39.41 Urge incontinence N39.42 Incontinence without sensory awareness N39.43 Post-void dribbling N39.44 Nocturnal enuresis N39.45 Continuous leakage N39.46 Mixed incontinence N39.490 Overflow incontinence N39.491 Coital incontinence N39.492 Postural -

Disseminated Eosinophilic Infiltration of a Newborn Infant, with Perforation of the Terminal Ileum and Bile Duct Obstruction
Arch Dis Child: first published as 10.1136/adc.56.1.66 on 1 January 1981. Downloaded from 66 Shinozaki, Saito, and Shiraki infant who acquired hepatitis from her mother. Br Med J 6 Yoshida A, Tozawa M, Furukawa N, Oya N, Kusunoki T, 1970; iv: 719-21. Kiyosawa N. HBsAg-positive chronic active hepatitis in 3 Bancroft W H, Warkel R L, Talbert A A, Russell P K. a 1 and 1/2 year-old-child (in Japanese). Shonika Shinryo Family with hepatitis-associated antigen. JAMA 1971; 1977;40: 1246-50. 217:1817-20. McCarthy J W. Hepatitis B antigen (HBAg)-positive chronic aggressive hepatitis and cirrhosis in an 8-month- Correspondence to Dr T Shinozaki, Department of old infant. A case report. JPediatr 1973; 83: 638-9. Paediatrics, Teikyo University School of Medicine, 11-1 5 Fujiwara T, Abe M, Tachi N, Jo M, Shiroda M. Kaga, 2 Chome, Itabashi-ku, Tokyo 173, Japan. HBsAg-positive infantile hepatitis associated with chronic aggressive hepatitis (in Japanese). Shonika Rinsho 1975; 28:1303-6. Received 26 November 1979 Disseminated eosinophilic infiltration of a newborn infant, with perforation of the terminal ileum and bile duct obstruction S M MURRAY AND C J WOODS Department ofPathology and Department ofPaediatrics, Victoria Hospital, Blackpool Case report SUMMARY A preterm boy died 4 days after delivery from septicaemia which at necropsy was found to be A white boy, weighing 1490 g, was born by spon- due to perforation of an eosinophilic lesion of the taneous vertex delivery at 35 weeks' gestation to a copyright. terminal ileum. -

A STUDY of RICKETS; Incidence in London
Arch Dis Child: first published as 10.1136/adc.61.10.939 on 1 October 1986. Downloaded from Archives of Disease in Childhood, 1986, 61, 939-940 A STUDY OF RICKETS; Incidence in London. BY DONALD PATERSON, M.B. (Edin.), M.R.C.P. (London), AND RUTH DARBY, M.B., Ch.B. (Birm.). (From the Infants' Hospital, Westminster.) In order to ascertain the incidence of rickets in London a study was attempted during the months of February, MIarch and April of 1925. It was thought that these being the darkest months of the year, following on a long, sunless period, the incidence of rickets would be at its height. Our fir-st difficulty was to define the basis upon which rickets could be diagnosed. We had over and over again diagnosed rickets clinically . Commentary copyright. J 0 FORFAR The Archives of Disease in Childhood, although it radiologically and 110 (32%) showed evidence of became the official journal of the British Paediatric previous rickets clinically, although radiologically Association (BPA), was first published two years the rickets was shown to have healed. No evidence before the founding of the BPA. Appropriately, the of rickets either clinically or radiologically was senior author of this paper on rickets, Dr Donald found in 225 (67%). Interestingly from a social point Paterson, played a leading part in the founding of of view, another paper in the same issue of the the BPA and was its first Secretary. He was a Archives (by Drs W P T Atkinson, Helen Mackay, http://adc.bmj.com/ Canadian who came to Edinburgh University to W L Kinnear, and H L Shaw) showed that children study medicine. -
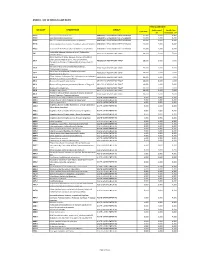
Annex 1: List of Medical Case Rates
ANNEX 1. LIST OF MEDICAL CASE RATES FIRST CASE RATE ICD CODE DESCRIPTION GROUP Professional Health Care Case Rate Fee Institution Fee P91.3 Neonatal cerebral irritability ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.4 Neonatal cerebral depression ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.6 Hypoxic ischemic encephalopathy of newborn ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.8 Other specified disturbances of cerebral status of newborn ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.9 Disturbance of cerebral status of newborn, unspecified ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 Peritonsillar abscess; Abscess of tonsil; Peritonsillar J36 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 cellulitis; Quinsy Other diseases of larynx; Abscess of larynx; Cellulitis of larynx; Disease NOS of larynx; Necrosis of larynx; J38.7 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Pachyderma of larynx; Perichondritis of larynx; Ulcer of larynx Retropharyngeal and parapharyngeal abscess; J39.0 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Peripharyngeal abscess Other abscess of pharynx; Cellulitis of pharynx; J39.1 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Nasopharyngeal abscess Other diseases of pharynx; Cyst of pharynx or nasopharynx; J39.2 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Oedema of pharynx or nasopharynx J85.1 Abscess of lung with pneumonia ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 J85.2 Abscess of lung without pneumonia; Abscess of lung NOS ABSCESS OF RESPIRATORY -
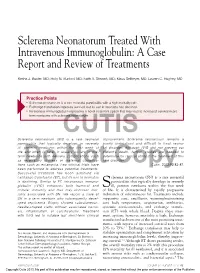
Sclerema Neonatorum Treated with Intravenous Immunoglobulin: a Case Report and Review of Treatments
Sclerema Neonatorum Treated With Intravenous Immunoglobulin: A Case Report and Review of Treatments Kesha J. Buster, MD; Holly N. Burford, MD; Faith A. Stewart, MD; Klaus Sellheyer, MD; Lauren C. Hughey, MD Practice Points Sclerema neonatorum is a rare neonatal panniculitis with a high mortality rate. Exchange transfusion improves survival, but its use in neonates has declined. Intravenous immunoglobulin represents a novel treatment option that may lead to increased survival in pre- term newborns with sclerema neonatorum. Sclerema neonatorum (SN)CUTIS is a rare neonatal improvement. Sclerema neonatorum remains a panniculitis that typically develops in severely poorly understood and difficult to treat neona- ill, preterm newborns within the first week of tal disorder. Although IVIG did not prevent our life and often is fatal. It usually occurs in pre- patient’s death, further studies are needed to term newborns with delivery complications such determine its clinical utility in the treatment of this as respiratory distress or maternal complica- rare disorder. tions such as eclampsia. Few clinical trials have Cutis. 2013;92:83-87. beenDo performed to address Notpotential treatments. Copy Successful treatment has been achieved via exchange transfusion (ET), but its use in neonates clerema neonatorum (SN) is a rare neonatal is declining. Similar to ET, intravenous immuno- panniculitis that typically develops in severely globulin (IVIG) enhances both humoral and Sill, preterm newborns within the first week cellular immunity and thus may decrease mor- of life. It is characterized by rapidly progressive tality associated with SN. We report a case of induration of subcutaneous fat. Treatments include SN in a term newborn who subsequently devel- supportive care, emollients, warming/maintaining oped septicemia. -

Ten Leading Causes of Death by Age Group,Race/Ethnicity, and Gender
Ten Leading Causes of Death by Age Group, Race/Ethnicity, and Gender Suburban Cook County 2006-2008 Suggested Citation: Cook County Department of Public Health. (2013). Ten Leading Causes of Death Tables 2008. Oak Forest, IL: Community Epidemiology and Health Planning Unit Table of Contents All Suburban Cook County: All Deaths By Gender: Females Males By Race/Ethnicity and Gender: Hispanic Hispanic Females Hispanic Males Non Hispanic Asian/Pacific Islander Non Hispanic Asian/Pacific Islander Females Non Hispanic Asian/Pacific Islander Males Non Hispanic Black Non Hispanic Black Females Non Hispanic Black Males Non Hispanic White Non Hispanic White Females Non Hispanic White Males By District: Cook County Department of Public Health Jurisdiction North District West District Southwest District South District Resources: District Map Rankable Causes of Death Rankable Causes of Infant Death 10 Leading Causes of Death by Age Group, Suburban Cook County, 2006-2008 (Counts/Percent of Total Deaths) All Deaths Rank <1 1-4 5-17 18-24 25-34 35-44 45-54 55-64 65+ Total Unintentional Unintentional Unintentional Unintentional Malignant Malignant Malignant Short Gestation Heart Disease Heart Disease 1 Injury Injury Injury Injury Neoplasms Neoplasms Neoplasms 170 24.9% 24 23.8% 57 24.6% 196 37.0% 281 34.4% 300 19.2% 1,251 31.7% 2,489 38.9% 13,422 28.2% 16,345 26.4% Congenital Congenital Unintentional Malignant Malignant Homicide Homicide Homicide Heart Disease Heart Disease 2 Anomalies Anomalies Injury Neoplasms Neoplasms 127 18.6% 9 8.9% 44 19.0% 135 -

Helping Mothers Defend Their Decision to Breastfeed
University of Central Florida STARS Electronic Theses and Dissertations, 2004-2019 2015 Helping Mothers Defend their Decision to Breastfeed Kandis Natoli University of Central Florida Part of the Nursing Commons Find similar works at: https://stars.library.ucf.edu/etd University of Central Florida Libraries http://library.ucf.edu This Doctoral Dissertation (Open Access) is brought to you for free and open access by STARS. It has been accepted for inclusion in Electronic Theses and Dissertations, 2004-2019 by an authorized administrator of STARS. For more information, please contact [email protected]. STARS Citation Natoli, Kandis, "Helping Mothers Defend their Decision to Breastfeed" (2015). Electronic Theses and Dissertations, 2004-2019. 1392. https://stars.library.ucf.edu/etd/1392 HELPING MOTHERS DEFEND THEIR DECISION TO BREASTFEED by KANDIS M. NATOLI M.S.N. University of Central Florida, 2006 B.S.N. University of Central Florida, 2005 A dissertation submitted in partial fulfillment of the requirements for the Degree of Doctor of Philosophy in Nursing in the College of Nursing at the University of Central Florida Orlando Florida Fall Term 2015 Major Professor: Karen Arioan © 2015 Kandis M. Natoli ii ABSTRACT The United States has established breastfeeding as an important health indicator within the Healthy People agenda. Healthy People target goals for breastfeeding initiation, duration, and exclusivity remain unmet. The US Surgeon General’s Office reports that lack of knowledge and widespread misinformation about breastfeeding are barriers to meeting Healthy People goals. Breastfeeding mothers are vulnerable to messages that cast doubt on their ability to breastfeed. Very little research has examined specific approaches to help people resist negative messages about health beliefs and behaviors. -

Handbook of Pediatric Autopsy Pathology
Handbook of Pediatric Autopsy Pathology Enid Gilbert-Barness • Diane E. Spicer Thora S. Steffensen Handbook of Pediatric Autopsy Pathology Second Edition Foreword by John M. Opitz Enid Gilbert-Barness, AO, MD, MBBS, FRCPA, Thora S. Steffensen, MD FRCPath, DSci(hc), MD(hc), DSci(hc) Department of Pathology Professor of Pathology and Cell Tampa General Hospital Biology, Laboratory Medicine, Pediatrics and Tampa , Florida Obstetrics and Gynecology USA Tampa General Hospital Morsani College of Medicine University of South Florida Tampa , Florida USA Diane E. Spicer, BS, PA(ASCP) Department of Pediatrics-Cardiology University of Florida Valrico , Florida USA ISBN 978-1-4614-6710-6 ISBN 978-1-4614-6711-3 (eBook) DOI 10.1007/978-1-4614-6711-3 Springer New York Heidelberg Dordrecht London Library of Congress Control Number: 2013941138 © Springer Science+Business Media New York 2014 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, speci fi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on micro fi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied speci fi cally for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. Duplication of this publication or parts thereof is permitted only under the provisions of the Copyright Law of the Publisher’s location, in its current version, and permission for use must always be obtained from Springer. -

Erythematous Plaque on the Back of a Newborn
PHOTO CHALLENGE Erythematous Plaque on the Back of a Newborn Tam H. Nguyen, DO; Kimberly Tamargo, MD; Matthew Franklin, MD; Lisa N. Gelles, MD An 8-day-old female infant presented with a mass on the lower back that had been present since birth. The patient was wellcopy appearing, alert, and active. Physical examination revealed a 6×5-cm, erythematous, ill-defined, indurated plaque on the lower thoracic back. There was no associ- ated family history of similar findings. Accord- ing to the mother, the patient was feeding well with nonot recent fever, irritability, or lethargy. The patient was born via elective induction of labor at term due to maternal intrauterine infection from chorioamnionitis. The birth was complicated by shoulder dystocia with an Erb palsy, and she was hospitalized for 5 days after delivery for manage- Doment of hypotension and ABO isoimmunization and to rule out sepsis; blood cultures were nega- tive for neonatal infection. WHAT’S THE DIAGNOSIS? a. bacterial cellulitis b. cutis marmorata c. infantile hemangioma d. sclerema neonatorum CUTIS e. subcutaneous fat necrosis PLEASE TURN TO PAGE E6 FOR THE DIAGNOSIS Dr. Nguyen is from the Dermatology Residency Program, Larkin Community Hospital, South Miami, Florida. Drs. Tamargo, Franklin, and Gelles are from MetroHealth Medical Center, Cleveland, Ohio. The authors report no conflict of interest. Correspondence: Tam H. Nguyen, DO ([email protected]). WWW.MDEDGE.COM/DERMATOLOGY VOL. 106 NO. 1 I JULY 2020 E5 Copyright Cutis 2020. No part of this publication may be reproduced, -

XI. COMPLICATIONS of PREGNANCY, Childbffith and the PUERPERIUM 630 Hydatidiform Mole Trophoblastic Disease NOS Vesicular Mole Ex
XI. COMPLICATIONS OF PREGNANCY, CHILDBffiTH AND THE PUERPERIUM PREGNANCY WITH ABORTIVE OUTCOME (630-639) 630 Hydatidiform mole Trophoblastic disease NOS Vesicular mole Excludes: chorionepithelioma (181) 631 Other abnormal product of conception Blighted ovum Mole: NOS carneous fleshy Excludes: with mention of conditions in 630 (630) 632 Missed abortion Early fetal death with retention of dead fetus Retained products of conception, not following spontaneous or induced abortion or delivery Excludes: failed induced abortion (638) missed delivery (656.4) with abnormal product of conception (630, 631) 633 Ectopic pregnancy Includes: ruptured ectopic pregnancy 633.0 Abdominal pregnancy 633.1 Tubalpregnancy Fallopian pregnancy Rupture of (fallopian) tube due to pregnancy Tubal abortion 633.2 Ovarian pregnancy 633.8 Other ectopic pregnancy Pregnancy: Pregnancy: cervical intraligamentous combined mesometric cornual mural - 355- 356 TABULAR LIST 633.9 Unspecified The following fourth-digit subdivisions are for use with categories 634-638: .0 Complicated by genital tract and pelvic infection [any condition listed in 639.0] .1 Complicated by delayed or excessive haemorrhage [any condition listed in 639.1] .2 Complicated by damage to pelvic organs and tissues [any condi- tion listed in 639.2] .3 Complicated by renal failure [any condition listed in 639.3] .4 Complicated by metabolic disorder [any condition listed in 639.4] .5 Complicated by shock [any condition listed in 639.5] .6 Complicated by embolism [any condition listed in 639.6] .7 With other -

Newborn Payment Policy Applies to the Following Tufts Health Plan Products
Newborn Payment Policy Applies to the following Tufts Health Plan products: ☒ Tufts Health Plan Commercial (including Tufts Health Freedom Plan)1 ☐ Tufts Medicare Preferred HMO (a Medicare Advantage product) ☐ Tufts Health Plan Senior Care Options (SCO) (a dual-eligible product) The following payment policy applies to Tufts Health Plan contracting inpatient facilities and professional providers who render newborn services in an inpatient setting. In addition to the specific information contained in this policy, providers must adhere to the information outlined in the Professional Services and Facilities Payment Policy. Note: Audit and disclaimer information is located at the end of this document. POLICY Tufts Health Plan covers medically necessary well and sick newborn services, in accordance with the member’s benefits and in accordance with federal and applicable state mandate coverage including, but not limited to the provisions of, Chapter 175 Section 47C, Chapter 175 Section 47F and Chapter 176G Section 4. GENERAL BENEFIT INFORMATION Services and subsequent payment are pursuant to the member's benefit plan document. Member eligibility and benefit specifics should be verified prior to initiating services by logging on to the secure Provider website or by contacting Commercial Provider Services. PREVENTIVE SERVICES Due to the Patient Protection and Affordable Care Act (commonly referred to as federal health care reform), with the exception of groups maintaining “grandfathered” status, all Tufts Health Plan products provide 100% coverage for preventive care services. Grandfathered groups are not subject to this requirement, but many have opted to cover preventive services with no cost sharing. This means that most members will have no cost-sharing responsibility when preventive services are rendered by an in-network provider.