ICD-10-CM TABULAR LIST of DISEASES and INJURIES
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Brief History of Pressure Ulcer Measurement in England: the Last 20 Years
EDITORIAL A brief history of pressure ulcer measurement in England: the last 20 years ressure ulcers (PU) have long been Measuring pressure ulcers: recognised as a challenge to healthcare, are prevalence and incidence a cause of significant pain and distress for During this time, the most reported forms of Ppatients and are costly for healthcare providers measurement have been prevalence and incidence. in term of finances and use of human resource Prevalence is the proportion of a population (Guest et al, 2020). who have a specific characteristic in a given This paper, the first in a series of three, describes time period. Therefore, the prevalence of PUs is the predominant methods that have been used to the proportion of a defined patient population JACQUI FLETCHER OBE capture the prevalence of PUs in England over the with pressure damage during a specified time Clinical Lead Pressure Ulcer last 20 years. The second paper will describe the period. Incidence is the number of specified new Workstream National Wound proposed system for national PU measurement events, during a specified period in a specified Care Strategy Clinical Editor, Wounds UK in England and the third paper will outline population. Therefore, the incidence of pressure proposals for implementing this system to drive damage is the number of people in a defined quality improvement. patient population who develop a new PU during a specified time period. BACKGROUND Prevalence of pressure damage is a good Measurement of the occurrence of PUs (also indicator of the overall burden and clinical known as pressure sores, decubitus ulcers, workload related to pressure damage but does pressure injury and bed sores) has been a part of not identify when and where the PU occurred, nursing activity for many years. -

The Pressure Sore Case: a Medical Perspective
Marquette Elder's Advisor Volume 2 Article 7 Issue 2 Fall The rP essure Sore Case: A Medical Perspective Jeffrey M. Levine Follow this and additional works at: http://scholarship.law.marquette.edu/elders Part of the Elder Law Commons Repository Citation Levine, Jeffrey M. (2000) "The rP essure Sore Case: A Medical Perspective," Marquette Elder's Advisor: Vol. 2: Iss. 2, Article 7. Available at: http://scholarship.law.marquette.edu/elders/vol2/iss2/7 This Featured Article is brought to you for free and open access by the Journals at Marquette Law Scholarly Commons. It has been accepted for inclusion in Marquette Elder's Advisor by an authorized administrator of Marquette Law Scholarly Commons. For more information, please contact [email protected]. The Pressure Sore Case: A Medical Perspective Although bedsores sometimes result dents.7 As a result, malpractice litigation related to pressure sores exploded in the 1990s.1 from inadequate care, not all cases Clinical Practice Guidelines involving pressure ulcers merit a law- Define Pressure Sores suit. This article adopts a medical per- Clinical practice guidelines define a pressure ulcer as "[a]ny skin lesion, usually over a bony promi- spective in its consideration of the pres- nence, caused by unrelieved pressure resulting in damage of underlying tissue." 9 The incidence of sure sore case, particularlywhen evalu- pressure ulcers in nursing homes is 0.20 to 0.56 per 1,000 resident-days, which may increase to 14 per ating deviation from the standard of 1,000 resident-days among those at high risk.' ° Commonly affected sites, comprising approximate- care. -

Dissecting Cellulitis
Patient Information Leaflet Dr Paul Farrant FRCP Consultant Dermatologist Janet Dix (Secretary to Dr Paul Farrant) Tel 01444 412273 Fax 01444 657397 Email [email protected] Web drpaulfarrant.co.uk Dissecting Cellulitis What is dissecting cellulitis? Dissecting cellulitis is a type of scarring hair loss that presents with pustules, boggy swellings, and sinuses within the scalp. What causes dissecting cellulitis? The cause of dissecting cellulitis is not known. It is associated with severe cystic acne known as acne conglobata, and hidradenitis suppurativa, which causes cystic swellings in the armpits and groin. In all of these conditions the hair follicle becomes blocked, dilates and ruptures. This causes an inflammatory response in the skin, which leads to pus formation, swellings and sinus formation. It is not uncommon for bacteria to be isolated from the skin but this is likely to be secondary to the inflammatory process. Is dissecting cellulitis inherited? Dissecting cellulitis is most commonly seen in Afro-Caribbean men but the racial predilection is more likely to be due to the shape and structural differences of Afro-Caribbean hair than a genetic predisposition to the condition. Hair care practices, such as clipping, may also play a role. It is not thought to be an inherited condition. What are the symptoms? Patients with dissecting cellulitis often complain of pain, tenderness and fluid discharge from the affected area. It is associated with hair loss. What does dissecting cellulitis look like? Dissecting Cellulitis is characterised by a localised area of hair loss, pustules, boggy swellings and sinus formation. Gentle pressure on the boggy areas may lead to expression of pus or serous fluid. -

EAACI/ESCD Skin Allergy Meeting 2017 (SAM 2017)
Clin Transl Allergy 2017, 7(Suppl 4):47 DOI 10.1186/s13601-017-0184-5 Clinical and Translational Allergy MEETING ABSTRACTS Open Access EAACI/ESCD Skin Allergy Meeting 2017 (SAM 2017) Zurich, Switzerland. 27 – 29 April 2017 Published: 15 December 2017 Thursday, 27 April 2017 O02 Assessment of aggregate consumer exposure to isothiazolinones O01 via cosmetics and detergents Methylisothiazolinone contact allergy: a real outbreak Elena Garcia Hidalgo, Natalie Von Goetz, Konrad Hungerbühler Luis Amaral1, Emidio Silva2, Marcio Oliveira3, Ana Paula Cunha4 ETH Zürich, Zürich, Switzerland 1Serviço de Imunoalergologia, Centro Hospitalar de São João E.P.E., Porto, Correspondence: Elena Garcia Hidalgo ‑ [email protected] Portugal; 2Serviço de Medicina do Trabalho e Saúde Ocupacional, Centro Clinical and Translational Allergy 2017, 7(Supple 4):O02 Hospitalar do Baixo Vouga E.P.E., Aveiro, Portugal; 3Serviço de Saúde Ocu‑ pacional, Centro Hospitalar de São João E.P.E., Porto, Portugal; 4Serviço de Background: Isothiazoliones can cause allergic contact dermati- Dermatologia, Centro Hospitalar de São João E.P.E., Porto, Portugal tis and are present in a variety of consumer products, such as cos- Correspondence: Luis Amaral ‑ [email protected] metics, detergents and do-it-yourself products. Skin sensitization Clinical and Translational Allergy 2017, 7(Supple 4):O01 is induced following dermal exposure to a sensitizer in an amount exceeding the sensitization threshold. The critical determinant of Background: Methylisothiazolinone (MI) is used as a preservative in exposure for evaluating skin sensitization risks is dose per unit area occupational, domestic products and, since 2005, in cosmetics. It is a of exposed skin. -

Guidelines of Care for the 10 Most Common Dermatologic Diseases
1 Guidelines of Care for the 10 most common dermatologic diseases: Copyright by the American Academy of Dermatology, Inc. Disclaimer Adherence to these guidelines will not ensure successful treatment in every situation. Further, these guidelines should not be deemed inclusive of all proper methods of care or exclusive of other methods of care reasonably directed to obtaining the same results. The ultimate judgment regarding the propriety of any specific procedure must be made by the physician in light of all the circumstances presented by the individual patient. For the benefit of members of the American Academy of Dermatology who practice in countries outside the jurisdiction of the United States, the listed treatments may include agents that not currently approved by the U.S. Food and Drug Administration. 1. Acne Vulgaris 2. Alopecia Areata 3. Atopic Dermatitis 4. Contact Dermatitis 5. Cutaneous Adverse Drug Reactions 6. Nail Disorders 7. Psoriasis 8. Superficial Mycotic Infections of the Skin: Mucocutaneous Candidiasis, Onychomycosis, Piedra, Pityriasis, Tinea Capitis , Tinea Barbae, Tinea Corporis, Tinea Cruris, Tinea Faciei, Tinea Manuum, and Tinea Pedis. 9. Vitiligo 10. Warts: Human Papillomavirus 1 2 1- Guidelines of Care for Acne Vulgaris* Reference: 1990 by the American Academy of Dermatology, Inc. I. Introduction The American Academy of Dermatology’s Committee on Guidelines of Care is developing guidelines of care for our profession. The development of guidelines will promote the continued delivery of quality care and assist those outside our profession in understanding the complexities and boundaries of care provided by dermatologists. II. Definition Acne vulgaris is a follicular disorder that affects susceptible pilosebaceous follicles, primarily of the face, neck, and upper trunk, and is characterized by both noninflammatory and inflammatory lesions. -

Pediatric and Adolescent Dermatology
Pediatric and adolescent dermatology Management and referral guidelines ICD-10 guide • Acne: L70.0 acne vulgaris; L70.1 acne conglobata; • Molluscum contagiosum: B08.1 L70.4 infantile acne; L70.5 acne excoriae; L70.8 • Nevi (moles): Start with D22 and rest depends other acne; or L70.9 acne unspecified on site • Alopecia areata: L63 alopecia; L63.0 alopecia • Onychomycosis (nail fungus): B35.1 (capitis) totalis; L63.1 alopecia universalis; L63.8 other alopecia areata; or L63.9 alopecia areata • Psoriasis: L40.0 plaque; L40.1 generalized unspecified pustular psoriasis; L40.3 palmoplantar pustulosis; L40.4 guttate; L40.54 psoriatic juvenile • Atopic dermatitis (eczema): L20.82 flexural; arthropathy; L40.8 other psoriasis; or L40.9 L20.83 infantile; L20.89 other atopic dermatitis; or psoriasis unspecified L20.9 atopic dermatitis unspecified • Scabies: B86 • Hemangioma of infancy: D18 hemangioma and lymphangioma any site; D18.0 hemangioma; • Seborrheic dermatitis: L21.0 capitis; L21.1 infantile; D18.00 hemangioma unspecified site; D18.01 L21.8 other seborrheic dermatitis; or L21.9 hemangioma of skin and subcutaneous tissue; seborrheic dermatitis unspecified D18.02 hemangioma of intracranial structures; • Tinea capitis: B35.0 D18.03 hemangioma of intraabdominal structures; or D18.09 hemangioma of other sites • Tinea versicolor: B36.0 • Hyperhidrosis: R61 generalized hyperhidrosis; • Vitiligo: L80 L74.5 focal hyperhidrosis; L74.51 primary focal • Warts: B07.0 verruca plantaris; B07.8 verruca hyperhidrosis, rest depends on site; L74.52 vulgaris (common warts); B07.9 viral wart secondary focal hyperhidrosis unspecified; or A63.0 anogenital warts • Keratosis pilaris: L85.8 other specified epidermal thickening 1 Acne Treatment basics • Tretinoin 0.025% or 0.05% cream • Education: Medications often take weeks to work AND and the patient’s skin may get “worse” (dry and red) • Clindamycin-benzoyl peroxide 1%-5% gel in the before it gets better. -

Download WAO White Book on Allergy
WORLD ALLERGY ORGANIZATION WAWAOO WhiteWhite BookBook onon AllergyAllergy WAO White Book on Allergy World Allergy Organization (WAO) White Book on Allergy Copyright 2011 World Allergy Organization WAO White Book on Allergy Editors Prof. Ruby Pawankar, MD, PhD Prof. Giorgio Walter Canonica, MD WAO President Elect (2010-2011) WAO Past President (2010-2011) Allergy and Rhinology Allergy & Respiratory Diseases Nippon Medical School Department of Internal Medicine 1-1-5 Sendagi, Bunkyo-ku University of Genoa Tokyo 113-8603 Padiglione Maragliano, Largo Rosanna Benzi 10 JAPAN 1-16132 Genoa ITALY Prof. Stephen T. Holgate, BSc, MD, DSc, FMed Sci Prof. Richard F. Lockey, MD Member, WAO Board of Directors (2010-2011) WAO President (2010-2011) Medical Research Council Clinical Professor of Division of Allergy & Immunology Immunopharmacology Joy McCann Culverhouse Chair in Allergy & Immunology Infection, Inflammation and Immunity University of South Florida College of Medicine School of Medicine James Haley Veterans Administration Medical Center (111D) University of Southampton 13000 Bruce B. Downs Boulevard Level F, South Block Tampa, Florida 33612 Southampton General Hospital USA Tremona Road Southampton SO16 6YD United Kingdom Acknowledgement On behalf of the World Allergy Organization (WAO), the editors and authors of the WAO White Book on Allergy express their gratitude to the charity, Asthma, Allergy, Inflammation Research (AAIR) and Asian Allergy Asthma Foundation (AAAF) for their support in the production of this publication. The Editors of the White book extend their gratitude to His Excellency Dr. APJ Abdul Kalam, Former President of India and Madame Ilora Finlay Baronness of the House of Lords for their Forewords to the White Book and to the International Primary Care Respiratory Group (IPCRG) and European Federation of Allergy and Airways Diseases Patients ‘Associations (EFA) for their supporting statements. -

Wound Classification
Wound Classification Presented by Dr. Karen Zulkowski, D.N.S., RN Montana State University Welcome! Thank you for joining this webinar about how to assess and measure a wound. 2 A Little About Myself… • Associate professor at Montana State University • Executive editor of the Journal of the World Council of Enterstomal Therapists (JWCET) and WCET International Ostomy Guidelines (2014) • Editorial board member of Ostomy Wound Management and Advances in Skin and Wound Care • Legal consultant • Former NPUAP board member 3 Today We Will Talk About • How to assess a wound • How to measure a wound Please make a note of your questions. Your Quality Improvement (QI) Specialists will follow up with you after this webinar to address them. 4 Assessing and Measuring Wounds • You completed a skin assessment and found a wound. • Now you need to determine what type of wound you found. • If it is a pressure ulcer, you need to determine the stage. 5 Assessing and Measuring Wounds This is important because— • Each type of wound has a different etiology. • Treatment may be very different. However— • Not all wounds are clear cut. • The cause may be multifactoral. 6 Types of Wounds • Vascular (arterial, venous, and mixed) • Neuropathic (diabetic) • Moisture-associated dermatitis • Skin tear • Pressure ulcer 7 Mixed Etiologies Many wounds have mixed etiologies. • There may be both venous and arterial insufficiency. • There may be diabetes and pressure characteristics. 8 Moisture-Associated Skin Damage • Also called perineal dermatitis, diaper rash, incontinence-associated dermatitis (often confused with pressure ulcers) • An inflammation of the skin in the perineal area, on and between the buttocks, into the skin folds, and down the inner thighs • Scaling of the skin with papule and vesicle formation: – These may open, with “weeping” of the skin, which exacerbates skin damage. -

Urticaria from Wikipedia, the Free Encyclopedia Jump To: Navigation, Search "Hives" Redirects Here
Urticaria From Wikipedia, the free encyclopedia Jump to: navigation, search "Hives" redirects here. For other uses, see Hive. Urticaria Classification and external resourcesICD-10L50.ICD- 9708DiseasesDB13606MedlinePlus000845eMedicineemerg/628 MeSHD014581Urtic aria (or hives) is a skin condition, commonly caused by an allergic reaction, that is characterized by raised red skin wheals (welts). It is also known as nettle rash or uredo. Wheals from urticaria can appear anywhere on the body, including the face, lips, tongue, throat, and ears. The wheals may vary in size from about 5 mm (0.2 inches) in diameter to the size of a dinner plate; they typically itch severely, sting, or burn, and often have a pale border. Urticaria is generally caused by direct contact with an allergenic substance, or an immune response to food or some other allergen, but can also appear for other reasons, notably emotional stress. The rash can be triggered by quite innocent events, such as mere rubbing or exposure to cold. Contents [hide] * 1 Pathophysiology * 2 Differential diagnosis * 3 Types * 4 Related conditions * 5 Treatment and management o 5.1 Histamine antagonists o 5.2 Other o 5.3 Dietary * 6 See also * 7 References * 8 External links [edit] Pathophysiology Allergic urticaria on the shin induced by an antibiotic The skin lesions of urticarial disease are caused by an inflammatory reaction in the skin, causing leakage of capillaries in the dermis, and resulting in an edema which persists until the interstitial fluid is absorbed into the surrounding cells. Urticarial disease is thought to be caused by the release of histamine and other mediators of inflammation (cytokines) from cells in the skin. -

The Role of Pressure Ulcers in the Fight Against Antimicrobial Resistance
The role of pressure ulcer prevention in the fight against antimicrobial resistance Every year over 25,000 patients die in the EU alone as a result of infections caused by antibiotic- resistant bacteria. Globally the number of deaths due to antimicrobial resistance (AMR) was estimated to be 700,0001 in 2014 and that number has been calculated to rise to at least 10 million by 2050. The continuing emergence of AMR has become a recurring topic in the international health agenda as the increasingly serious threat to cross-border public health is recognised. From WHO to OECD, international bodies are constantly monitoring, reporting and formulating strategies to contain AMR. AMR is defined by WHO as the ability of microorganisms to survive antimicrobial treatments; consequently, prophylactic and therapeutic regimens are ineffective in controlling infections caused by resistant bacteria, fungi, parasites and viruses.2 The situation has deteriorated dramatically in the past decade with AMR reaching levels of 80% in some countries.3 How has this happened? Whereas greater investment and skill in reporting of AMR may be one reason, an important consideration is that AMR is a natural and inevitable process which is aggravated by the inappropriate use of antimicrobial agents. Healthcare authorities have been aware of the consequences of overuse of antibiotics in animal and human health, yet relatively few actions have been implemented to slow the process down.4 The good news is that the EU has made a significant step forward to gain a global lead in the fight against AMR. In June 2017 the Commission adopted the ambitious EU One Health Action Plan against AMR5 (as requested by the Member States in the Council Conclusions of 17 June 2016). -
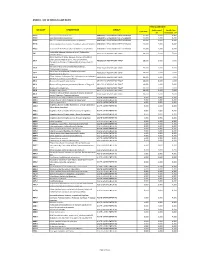
Annex 1: List of Medical Case Rates
ANNEX 1. LIST OF MEDICAL CASE RATES FIRST CASE RATE ICD CODE DESCRIPTION GROUP Professional Health Care Case Rate Fee Institution Fee P91.3 Neonatal cerebral irritability ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.4 Neonatal cerebral depression ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.6 Hypoxic ischemic encephalopathy of newborn ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.8 Other specified disturbances of cerebral status of newborn ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 P91.9 Disturbance of cerebral status of newborn, unspecified ABNORMAL SENSORIUM IN THE NEWBORN 12,000 3,600 8,400 Peritonsillar abscess; Abscess of tonsil; Peritonsillar J36 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 cellulitis; Quinsy Other diseases of larynx; Abscess of larynx; Cellulitis of larynx; Disease NOS of larynx; Necrosis of larynx; J38.7 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Pachyderma of larynx; Perichondritis of larynx; Ulcer of larynx Retropharyngeal and parapharyngeal abscess; J39.0 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Peripharyngeal abscess Other abscess of pharynx; Cellulitis of pharynx; J39.1 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Nasopharyngeal abscess Other diseases of pharynx; Cyst of pharynx or nasopharynx; J39.2 ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 Oedema of pharynx or nasopharynx J85.1 Abscess of lung with pneumonia ABSCESS OF RESPIRATORY TRACT 10,000 3,000 7,000 J85.2 Abscess of lung without pneumonia; Abscess of lung NOS ABSCESS OF RESPIRATORY -

Early Diagnosis and Treatment of Discoid Lupus Erythematosus
J Am Board Fam Med: first published as 10.3122/jabfm.2009.02.080075 on 5 March 2009. Downloaded from BRIEF REPORT Early Diagnosis and Treatment of Discoid Lupus Erythematosus Suresh Panjwani, MD, MSc, FRACGP Discoid lupus erythematosus is a chronic dermatological disease that can lead to scarring, hair loss, and hyperpigmentation changes in skin if it is not treated early and promptly. It has a prolonged course and can have a considerable effect on quality of life. Early recognition and treatment improves the prog- nosis. The diagnosis is usually made by clinical examination. In some cases histopathology may be re- quired to confirm the diagnosis. The histology is that of an inflammatory interface dermatosis. There is insufficient evidence for which treatment is most effective. Because lesions are induced or exacerbated by ultraviolet exposure, photoprotective measures are important. Potent topical steroids and antima- larials are the mainstay of treatment. Some cases of discoid lupus erythematosus can be refractory to standard therapy; in these cases retinoids, thalidomide, and topical tacrolimus offer alternatives, as do immunosuppressives like azathioprine, cyclosporine, mycophenolate mofetil, and methotrexate. (J Am Board Fam Med 2009;22:206–213.) Lupus erythematosus (LE) is thought to be an 5% of patients with discoid lupus may develop autoimmune disease among other connective tissue SLE1 and 25% of patients with SLE may develop diseases like scleroderma, rheumatoid arthritis, typical chronic discoid lesions at some time during copyright.