N35.12 Postinfective Urethral Stricture, NEC, Female N35.811 Other
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hypocalcemia Associated with Subcutaneous Fat Necrosis of the Newborn: Case Report and Literature Review Alphonsus N
case report Oman Medical Journal [2017], Vol. 32, No. 6: Hypocalcemia Associated with Subcutaneous Fat Necrosis of the Newborn: Case Report and Literature Review Alphonsus N. Onyiriuka 1* and Theodora E. Utomi2 1Endocrine and Metabolic Unit, Department of Child Health, University of Benin Teaching Hospital, Benin City, Nigeria 2Special Care Baby Unit, Department of Nursing Services, St Philomena Catholic Hospital, Benin City, Nigeria ARTICLE INFO ABSTRACT Article history: Subcutaneous fat necrosis of the newborn (SCFNN) is a rare benign inflammatory Received: 4 November 2015 disorder of the adipose tissue but may be complicated by hypercalcemia or less frequently, Accepted: 21 October 2016 hypocalcemia, resulting in morbidity and mortality. Here we report the case of a neonate Online: with subcutaneous fat necrosis who surprisingly developed hypocalcemia instead DOI 10.5001/omj.2017.99 of hypercalcemia. A full-term female neonate was delivered by emergency cesarean section for fetal distress and was subsequently admitted to the Special Care Baby Keywords: Hypocalcemia; Infant, Unit. The mother’s pregnancy was uncomplicated up to delivery. Her anthropometric Newborn; Subcutaneous Fat measurements were birth weight 4.1 kg (95th percentile), length 50 cm (50th percentile), Necrosis; Perinatal Stress. and head circumference 34.5 cm (50th percentile). The Apgar scores were 2, 3, and 8 at 1, 5, 10 minutes, respectively. There was no abnormal facies and she was fed with breast milk only. On the seventh day of life, the infant was found to have multiple nodules located in the neck, upper back, and right arm. The nodules were firm, well circumscribed with no evidence of tenderness. -

ICD10 Diagnoses FY2018 AHD.Com
ICD10 Diagnoses FY2018 AHD.com A020 Salmonella enteritis A5217 General paresis B372 Candidiasis of skin and nail A040 Enteropathogenic Escherichia coli A523 Neurosyphilis, unspecified B373 Candidiasis of vulva and vagina infection A528 Late syphilis, latent B3741 Candidal cystitis and urethritis A044 Other intestinal Escherichia coli A530 Latent syphilis, unspecified as early or B3749 Other urogenital candidiasis infections late B376 Candidal endocarditis A045 Campylobacter enteritis A539 Syphilis, unspecified B377 Candidal sepsis A046 Enteritis due to Yersinia enterocolitica A599 Trichomoniasis, unspecified B3781 Candidal esophagitis A047 Enterocolitis due to Clostridium difficile A6000 Herpesviral infection of urogenital B3789 Other sites of candidiasis A048 Other specified bacterial intestinal system, unspecified B379 Candidiasis, unspecified infections A6002 Herpesviral infection of other male B380 Acute pulmonary coccidioidomycosis A049 Bacterial intestinal infection, genital organs B381 Chronic pulmonary coccidioidomycosis unspecified A630 Anogenital (venereal) warts B382 Pulmonary coccidioidomycosis, A059 Bacterial foodborne intoxication, A6920 Lyme disease, unspecified unspecified unspecified A7740 Ehrlichiosis, unspecified B387 Disseminated coccidioidomycosis A080 Rotaviral enteritis A7749 Other ehrlichiosis B389 Coccidioidomycosis, unspecified A0811 Acute gastroenteropathy due to A879 Viral meningitis, unspecified B399 Histoplasmosis, unspecified Norwalk agent A938 Other specified arthropod-borne viral B440 Invasive pulmonary -

GERONTOLOGICAL NURSE PRACTITIONER Review and Resource M Anual
13 Male Reproductive System Disorders Vaunette Fay, PhD, RN, FNP-BC, GNP-BC GERIATRIC APPRoACH Normal Changes of Aging Male Reproductive System • Decreased testosterone level leads to increased estrogen-to-androgen ratio • Testicular atrophy • Decreased sperm motility; fertility reduced but extant • Increased incidence of gynecomastia Sexual function • Slowed arousal—increased time to achieve erection • Erection less firm, shorter lasting • Delayed ejaculation and decreased forcefulness at ejaculation • Longer interval to achieving subsequent erection Prostate • By fourth decade of life, stromal fibrous elements and glandular tissue hypertrophy, stimulated by dihydrotestosterone (DHT, the active androgen within the prostate); hyperplastic nodules enlarge in size, ultimately leading to urethral obstruction 398 GERONTOLOGICAL NURSE PRACTITIONER Review and Resource M anual Clinical Implications History • Many men are overly sensitive about complaints of the male genitourinary system; men are often not inclined to initiate discussion, seek help; important to take active role in screening with an approach that is open, trustworthy, and nonjudgmental • Sexual function remains important to many men, even at ages over 80 • Lack of an available partner, poor health, erectile dysfunction, medication adverse effects, and lack of desire are the main reasons men do not continue to have sex • Acute and chronic alcohol use can lead to impotence in men • Nocturia is reported in 66% of patients over 65 – Due to impaired ability to concentrate urine, reduced -
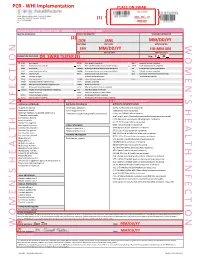
Womens Health Requisition Forms
PCR - WHI Implementation PLACE ON SWAB 10854 Midwest Industrial Blvd. St. Louis, MO 63132 MM DD YY Phone: (314) 200-3040 | Fax (314) 200-3042 (1) CLIA ID #26D0953866 JANE DOE v3 PCR MOLECULAR REQUISITION - WOMEN'S HEALTH INFECTION PRACTICE INFORMATION PATIENT INFORMATION *SPECIMEN INFORMATION (2) DOE JANE MM/DD/YY LAST NAME FIRST NAME DATE COLLECTED W O M E ' N S H E A L T H I F N E C T I O N SSN MM/DD/YY HH:MM AM SSN DATE OF BIRTH TIME COLLECTED REQUESTING PHYSICIAN: DR. SWAB TESTER (3) Sex: F X M (4) Diagnosis Codes X N76.0 Acute vaginitis B37.49 Other urogenital candidiasis A54.9 Gonococcal infection, unspecified N76.1 Subacute and chronic vaginitis N89.8 Other specified noninflammatory disorders of vagina A59.00 Urogenital trichomoniasis, unspecified N76.2 Acute vulvitis O99.820 Streptococcus B carrier state complicating pregnancy A64 Unspecified sexually transmitted disease N76.3 Subacute and chronic vulvitis O99.824 Streptococcus B carrier state complicating childbirth A74.9 Chlamydial infection, unspecified N76.4 Abscess of vulva B95.1 Streptococcus, group B, as the cause Z11.3 Screening for infections with a predmoninantly N76.5 Ulceration of vagina of diseases classified elsewhere sexual mode of trasmission N76.6 Ulceration of vulva Z22.330 Carrier of group B streptococcus Other: N76.81 Mucositis(ulcerative) of vagina and vulva N70.91 Salpingitis, unspecified N76.89 Other specified inflammation of vagina and vulva N70.92 Oophoritis, unspecified N95.2 Post menopausal atrophic vaginitis N71.9 Inflammatory disease of uterus, unspecified -

Dysmenorrhea Due to a Rare Müllerian Anomaly
CASE REPORT Dysmenorrhea due to a rare müllerian anomaly M Agarwal, A Das, AS Singh Department of Obstetrics and Gynecology, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences Shillong, India Abstract Müllerian duct anomalies may produce reproductive failure like abortion and preterm birth, or obstetric problems like malpresentation, retained placenta, etc., or they may be asymptomatic. Unicornuate uterus with a noncommunicating functional rudimentary horn is a type of müllerian anomaly that results in obstruction to menstrual blood flow, leading to endometriosis and dysmenorrhea. Though the majority of cases of dysmenorrhea in adolescents are primary in nature and require only reassurance and symptomatic management, it is important to be aware of rare causes such as müllerian anomalies so that these cases can be properly managed. Hence, we present this case report, with interesting illustrations, so as to increase awareness regarding these anomalies. Key words: Dysmenorrhea, müllerian anomaly, unicornuate uterus Date of Acceptance: 13-Feb-2011 Introduction department with complaints of severe pain in the lower abdomen during her menses for the last 6 months. Apart Unicornuate uterus with a rudimentary horn is a rare type from severe dysmenorrhea there was no other menstrual of müllerian duct malformation and is the result of defective abnormality. Her vitals and per abdominal examination fusion of the malformed duct with the contralateral duct.[1] findings were normal. Ultrasonography of the abdomen The incidence of unicornuate uterus, although not precisely suggested the possibility of unicornuate uterus with right- known, is estimated at 1/1000 women.[2] A noncommunicating sided hematosalpinx and hematometra; also, the right rudimentary horn with a functional endometrial cavity is rare kidney was not visualized. -

Disseminated Eosinophilic Infiltration of a Newborn Infant, with Perforation of the Terminal Ileum and Bile Duct Obstruction
Arch Dis Child: first published as 10.1136/adc.56.1.66 on 1 January 1981. Downloaded from 66 Shinozaki, Saito, and Shiraki infant who acquired hepatitis from her mother. Br Med J 6 Yoshida A, Tozawa M, Furukawa N, Oya N, Kusunoki T, 1970; iv: 719-21. Kiyosawa N. HBsAg-positive chronic active hepatitis in 3 Bancroft W H, Warkel R L, Talbert A A, Russell P K. a 1 and 1/2 year-old-child (in Japanese). Shonika Shinryo Family with hepatitis-associated antigen. JAMA 1971; 1977;40: 1246-50. 217:1817-20. McCarthy J W. Hepatitis B antigen (HBAg)-positive chronic aggressive hepatitis and cirrhosis in an 8-month- Correspondence to Dr T Shinozaki, Department of old infant. A case report. JPediatr 1973; 83: 638-9. Paediatrics, Teikyo University School of Medicine, 11-1 5 Fujiwara T, Abe M, Tachi N, Jo M, Shiroda M. Kaga, 2 Chome, Itabashi-ku, Tokyo 173, Japan. HBsAg-positive infantile hepatitis associated with chronic aggressive hepatitis (in Japanese). Shonika Rinsho 1975; 28:1303-6. Received 26 November 1979 Disseminated eosinophilic infiltration of a newborn infant, with perforation of the terminal ileum and bile duct obstruction S M MURRAY AND C J WOODS Department ofPathology and Department ofPaediatrics, Victoria Hospital, Blackpool Case report SUMMARY A preterm boy died 4 days after delivery from septicaemia which at necropsy was found to be A white boy, weighing 1490 g, was born by spon- due to perforation of an eosinophilic lesion of the taneous vertex delivery at 35 weeks' gestation to a copyright. terminal ileum. -

Diseases of the Digestive System (KOO-K93)
CHAPTER XI Diseases of the digestive system (KOO-K93) Diseases of oral cavity, salivary glands and jaws (KOO-K14) lijell Diseases of pulp and periapical tissues 1m Dentofacial anomalies [including malocclusion] Excludes: hemifacial atrophy or hypertrophy (Q67.4) K07 .0 Major anomalies of jaw size Hyperplasia, hypoplasia: • mandibular • maxillary Macrognathism (mandibular)(maxillary) Micrognathism (mandibular)( maxillary) Excludes: acromegaly (E22.0) Robin's syndrome (087.07) K07 .1 Anomalies of jaw-cranial base relationship Asymmetry of jaw Prognathism (mandibular)( maxillary) Retrognathism (mandibular)(maxillary) K07.2 Anomalies of dental arch relationship Cross bite (anterior)(posterior) Dis to-occlusion Mesio-occlusion Midline deviation of dental arch Openbite (anterior )(posterior) Overbite (excessive): • deep • horizontal • vertical Overjet Posterior lingual occlusion of mandibular teeth 289 ICO-N A K07.3 Anomalies of tooth position Crowding Diastema Displacement of tooth or teeth Rotation Spacing, abnormal Transposition Impacted or embedded teeth with abnormal position of such teeth or adjacent teeth K07.4 Malocclusion, unspecified K07.5 Dentofacial functional abnormalities Abnormal jaw closure Malocclusion due to: • abnormal swallowing • mouth breathing • tongue, lip or finger habits K07.6 Temporomandibular joint disorders Costen's complex or syndrome Derangement of temporomandibular joint Snapping jaw Temporomandibular joint-pain-dysfunction syndrome Excludes: current temporomandibular joint: • dislocation (S03.0) • strain (S03.4) K07.8 Other dentofacial anomalies K07.9 Dentofacial anomaly, unspecified 1m Stomatitis and related lesions K12.0 Recurrent oral aphthae Aphthous stomatitis (major)(minor) Bednar's aphthae Periadenitis mucosa necrotica recurrens Recurrent aphthous ulcer Stomatitis herpetiformis 290 DISEASES OF THE DIGESTIVE SYSTEM Diseases of oesophagus, stomach and duodenum (K20-K31) Ill Oesophagitis Abscess of oesophagus Oesophagitis: • NOS • chemical • peptic Use additional external cause code (Chapter XX), if desired, to identify cause. -

A STUDY of RICKETS; Incidence in London
Arch Dis Child: first published as 10.1136/adc.61.10.939 on 1 October 1986. Downloaded from Archives of Disease in Childhood, 1986, 61, 939-940 A STUDY OF RICKETS; Incidence in London. BY DONALD PATERSON, M.B. (Edin.), M.R.C.P. (London), AND RUTH DARBY, M.B., Ch.B. (Birm.). (From the Infants' Hospital, Westminster.) In order to ascertain the incidence of rickets in London a study was attempted during the months of February, MIarch and April of 1925. It was thought that these being the darkest months of the year, following on a long, sunless period, the incidence of rickets would be at its height. Our fir-st difficulty was to define the basis upon which rickets could be diagnosed. We had over and over again diagnosed rickets clinically . Commentary copyright. J 0 FORFAR The Archives of Disease in Childhood, although it radiologically and 110 (32%) showed evidence of became the official journal of the British Paediatric previous rickets clinically, although radiologically Association (BPA), was first published two years the rickets was shown to have healed. No evidence before the founding of the BPA. Appropriately, the of rickets either clinically or radiologically was senior author of this paper on rickets, Dr Donald found in 225 (67%). Interestingly from a social point Paterson, played a leading part in the founding of of view, another paper in the same issue of the the BPA and was its first Secretary. He was a Archives (by Drs W P T Atkinson, Helen Mackay, http://adc.bmj.com/ Canadian who came to Edinburgh University to W L Kinnear, and H L Shaw) showed that children study medicine. -
Urologic Emergencies
Urologic emergencies Csaba Pusztai MD Emergency life threatening can lead to persistent impairment contagious – dangerous to others (STD) causes severe pain or discomfort Urologic emergencies renal trauma, bladder rupture, testicular torsion, anuria, renal occlusion, renal colic, severe pyelonephritis, renal abscess, perirenal abscess, Fournier’s gangrene, retroperitoneal hematoma, priapism, penile fracture, scrotal trauma, paraphimosis, urinary retention, ureter occlusion, foreign body, gonorrhoea, syphilis, AV fistula ... Contents Discussed: Not discussed: Urologic trauma STD Scrotal emergencies Renal colic Urosepsis Acute renal failure Urinary retention Penile emergencies Miscellaneous Mind urologic trauma, if Blunt trauma to the abdomen/perineum – hematuria – diminished urine output – genital or flank mass Penetrating wound of abdomen/perineum – 20% w/o macrohematuria Deceleration injury – motor vehicle accident Suspicius signs X-XII. rib fracture pelvic bone fracture flank mass, discoloration, wound lower abdominal mass, tenderness genital swelling and discoloration inability to void blood at the urethral meatus Evaluating urologic trauma Kidney – CT > US > IVP > angiography Bladder – RCG > CT > IVP > US Urethra – RUG Testis – US (>5 MHz) Renal injury - staging American College of Surgeons Committee on Trauma Grade I Contusion Microscopic or gross haematuria urologic studies normal Haematoma Subcapsular, nonexpanding haematoma without parenhymal laceration Grade II Haematoma Nonexpanding perirenal haematoma -

Lesions of the Female Urethra: a Review
Please do not remove this page Lesions of the Female Urethra: a Review Heller, Debra https://scholarship.libraries.rutgers.edu/discovery/delivery/01RUT_INST:ResearchRepository/12643401980004646?l#13643527750004646 Heller, D. (2015). Lesions of the Female Urethra: a Review. In Journal of Gynecologic Surgery (Vol. 31, Issue 4, pp. 189–197). Rutgers University. https://doi.org/10.7282/T3DB8439 This work is protected by copyright. You are free to use this resource, with proper attribution, for research and educational purposes. Other uses, such as reproduction or publication, may require the permission of the copyright holder. Downloaded On 2021/09/29 23:15:18 -0400 Heller DS Lesions of the Female Urethra: a Review Debra S. Heller, MD From the Department of Pathology & Laboratory Medicine, Rutgers-New Jersey Medical School, Newark, NJ Address Correspondence to: Debra S. Heller, MD Dept of Pathology-UH/E158 Rutgers-New Jersey Medical School 185 South Orange Ave Newark, NJ, 07103 Tel 973-972-0751 Fax 973-972-5724 [email protected] There are no conflicts of interest. The entire manuscript was conceived of and written by the author. Word count 3754 1 Heller DS Precis: Lesions of the female urethra are reviewed. Key words: Female, urethral neoplasms, urethral lesions 2 Heller DS Abstract: Objectives: The female urethra may become involved by a variety of conditions, which may be challenging to providers who treat women. Mass-like urethral lesions need to be distinguished from other lesions arising from the anterior(ventral) vagina. Methods: A literature review was conducted. A Medline search was used, using the terms urethral neoplasms, urethral diseases, and female. -

Left Twisted Hydrosalpinx Presenting As Acute Abdomen
The Journal of Obstetrics and Gynecology of India January/February 2011 pg 81 - 82 Case Report Left Twisted Hydrosalpinx Presenting as Acute Abdomen Pawar Uddhav1, Ghanekar Mahendra2 Department of Obstetrics and Gynaecology, Goa Medical College, Goa . A 30-year-old para 3 not sterilized was admitted on hemorrhage within i.e. in other words a left twisted 18.01.2006 with a history of acute pain in the abdomen hematosalpinx (Fig. 1 & 2 – the red arrow showing the of one day duration. She was in the 10th day post hematosalpinx and the gloved hand holding the uterus). menstrual cycle.. There was no history of dysmenorrhea. From the rest of her history all other The left ovary was normal and rest of the pelvic non gynecological causes of acute abdomen were ruled structures did not reveal any pathology. Left out. salpingectomy was done and as the patient desired ligation, right sided tubal ligation was also carried out. On examination her vitals were stable barring a mild The patient was discharged on 24.01.2006. The tachycardia; pulse rate=94/min. Per abdomen postoperative period was uneventful. The patient was examination there was tenderness in the left iliac fossa, given IV ofloxacin and IV-metronidazole for 24 hrs and no guarding or rigidity and bowel sounds were present. then switched over to oral ofloxacin for 10 days. She Bimanual pelvic examination revealed normal sized was asked to follow up with the histopathology reports uterus with tender cystic mass in left adnexa after 15 days. She followed up on 11.02.2006. The report approximately 4X4 cm and cervical motion tenderness was: gross - tube dilated and tortuous appearing bluish was positive. -
Common Benign Disorders of Bladder and Urethra
Common Benign Disorders of Bladder and Urethra 陳 宏 一 Hong-I, Chen, M.D., PhD., M.M.M., EMBA 軍醫局 局長 (2004--2008) 三 軍 總 醫 院 院 長 (2001-2004) 國 防 醫 學 院 醫 學 系 M67 (1973) 英 國 牛 津 大 學 神經藥理學 博 士 (1990) 美 國 杜 蘭 大 學 醫務管理 碩士 (2000) 國 立 台 灣 大 學 管理學院 EMBA (2006) H.I. Chen 1 Disorder of the Bladder, Prostate, Urethra, Seminal Vesicle, Penis, & Genitalia ◆ Anatomy and Histology (LOW URINARY TRACT) ◆ Physiology and Pharmacology ◆ Disorder ◆ Diagnosis and Treatment ◆ Prognosis H.I. Chen 2 Anatomy H.I. Chen 3 Prostate: blood supply H.I. Chen 4 H.I. Chen 5 H.I. Chen 6 H.I. Chen 7 H.I. Chen 8 H.I. Chen 9 H.I. Chen 10 Bladder : Disorders, Diagnosis & Treatment, Prognosis (interstitial cystitis) ◆ Acquired diseases of the bladder: A. Interstitial cystitis (Hunner’s ulcer, submucous fibrosis): a. fibrosis of the vesical wall, middle aged woman, loss of bladder capacity. b. frequency, urgency, nocturia and pelvic pain with bladder distention, urine is usually normal. c. small ulcers or cracks in the mucous membrane. d. microscopic hematuria may be noted. H.I. Chen 11 Bladder : Disorders, Diagnosis & Treatment, Prognosis (interstitial cystitis) e. ureterovesical junctions is destroyed, leading to vesicalureteral reflux, hydroureteronephrosis and pyelonephritis may then ensue. f. cystoscopy is usually diagnostic, as the bladder fills, increasing suprapubic pain is experienced. g. Treatment: There appears to be no definitive treatment for interstitial cystitis. H.I. Chen 12 Bladder : Disorders, Diagnosis & Treatment, Prognosis (interstitial cystitis) @ hydraulic overdistention with or without anesthesia.