List of Covered Drugs)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Summary of Drug Limitations Mary C
RON DESANTIS GOVERNOR SUMMARY OF DRUG LIMITATIONS MARY C. MAYHEW SECRETARY **Medications listed in this document may or may not require a prior authorization. Please view the Preferred Drug List at: http://ahca.myflorida.com/Medicaid/Prescribed_Drug/pharm_thera/fmpdl.shtml** Summary of Drug Limitations Abilify (aripiprazole) 2mg, 5mg, 20mg, 30mg tablets Minimum age = 6; Maximum of 1 tablet per day Abilify (aripiprazole) 10mg, 15mg tablets Minimum age = 6; Maximum of 15mg per day for ages = 6 - 11; Maximum of 30mg per day for ages = 12-17 Maximum of 1 tablet per day Abilify (aripiprazole) Discmelt 10mg, 15mg tabs Minimum age = 6; Maximum of 15mg per day for ages = 6 - 11; Maximum of 30mg per day for ages = 12-17; Maximum of 2 tablets per day Abilify (aripiprazole) 1mg/ml solution Minimum age = 6; Maximum of 15ml per day for ages = 6 - 11; Maximum of 30ml per day for ages = 12-17; Maximum of 30ml per day for ages =/> 18 Abilify Maintena (aripiprazole) syringe/vial Minimum age = 18; Maximum of 1 syringe or vial every 28 days Absorica (isotretinoin) 10mg, 20mg, 25mg,30mg, 35mg, & Minimum age = 12 40mg capsules Abstral (fentanyl citrate) sublingual tablets Minimum age = 18; Maximum of 4 sublingual tablets per day Acanya (benzoyl peroxide/clindamycin)Gel, gel pump Minimum Age= 12 Accolate (zafirlukast) tablets Maximum of 3 tablets per day Aciphex (rabeprazole) 5mg, 10mg sprinkle capsules Minimum age = 1; Maximum age = 11; Maximum of 1 capsule per day Aciphex (rabeprazole) 20mg tablets Minimum age = 1; Maximum of 2 tablets per day Actemra (tocilizumab) 80mg/4ml, 200mg/10ml, Minimum age= 2 400mg/20ml Vials, & 162mg/0.9ml Syringe Actimmune (Interferon Gamma-1b) Maximum of 6ml every 28days Actiq (fentanyl citrate) Lozenges Minimum age = 18; Maximum of 4 lozenges per day Activella (estradiol/norethindrone) tablets Minimum age = 18 Updated 02/28/2019 1 RON DESANTIS GOVERNOR SUMMARY OF DRUG LIMITATIONS MARY C. -

XERMELO™ (Telotristat Ethyl)
PHARMACY COVERAGE GUIDELINES ORIGINAL EFFECTIVE DATE: 5/18/2017 SECTION: DRUGS LAST REVIEW DATE: 5/20/2021 LAST CRITERIA REVISION DATE: 5/20/2021 ARCHIVE DATE: XERMELO™ (telotristat ethyl) Coverage for services, procedures, medical devices and drugs are dependent upon benefit eligibility as outlined in the member's specific benefit plan. This Pharmacy Coverage Guideline must be read in its entirety to determine coverage eligibility, if any. This Pharmacy Coverage Guideline provides information related to coverage determinations only and does not imply that a service or treatment is clinically appropriate or inappropriate. The provider and the member are responsible for all decisions regarding the appropriateness of care. Providers should provide BCBSAZ complete medical rationale when requesting any exceptions to these guidelines. The section identified as “Description” defines or describes a service, procedure, medical device or drug and is in no way intended as a statement of medical necessity and/or coverage. The section identified as “Criteria” defines criteria to determine whether a service, procedure, medical device or drug is considered medically necessary or experimental or investigational. State or federal mandates, e.g., FEP program, may dictate that any drug, device or biological product approved by the U.S. Food and Drug Administration (FDA) may not be considered experimental or investigational and thus the drug, device or biological product may be assessed only on the basis of medical necessity. Pharmacy Coverage Guidelines are subject to change as new information becomes available. For purposes of this Pharmacy Coverage Guideline, the terms "experimental" and "investigational" are considered to be interchangeable. BLUE CROSS®, BLUE SHIELD® and the Cross and Shield Symbols are registered service marks of the Blue Cross and Blue Shield Association, an association of independent Blue Cross and Blue Shield Plans. -
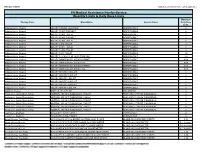
Quantity Limits/Daily Dose Limits
Effective 07/20/21 Alphabetical by Brand Name (when applicable) PA Medical Assistance Fee-for-Service Quantity Limits & Daily Dose Limits Maximum Therapy Class Brand Name Generic Name Daily Dose Limit Antipsychotics, Atypical ABILIFY 1 MG/ML SOLUTION ARIPIPRAZOLE 25 Antipsychotics, Atypical ABILIFY 10 MG DISCMELT ARIPIPRAZOLE 2 Antipsychotics, Atypical ABILIFY 10 MG TABLET ARIPIPRAZOLE 1 Antipsychotics, Atypical ABILIFY 15 MG DISCMELT ARIPIPRAZOLE 2 Antipsychotics, Atypical ABILIFY 15 MG TABLET ARIPIPRAZOLE 1 Antipsychotics, Atypical ABILIFY 2 MG TABLET ARIPIPRAZOLE 2 Antipsychotics, Atypical ABILIFY 20 MG TABLET ARIPIPRAZOLE 1 Antipsychotics, Atypical ABILIFY 30 MG TABLET ARIPIPRAZOLE 1 Antipsychotics, Atypical ABILIFY 5 MG TABLET ARIPIPRAZOLE 1.5 Antipsychotics, Atypical ABILIFY 9.75 MG/1.3 ML INJECTION VIAL ARIPIPRAZOLE 3.9 Antipsychotics, Atypical ABILIFY MAINTENA ER 300 MG SYRINGE ARIPIPRAZOLE 0.04 Antipsychotics, Atypical ABILIFY MAINTENA ER 300 MG VIAL ARIPIPRAZOLE 0.04 Antipsychotics, Atypical ABILIFY MAINTENA ER 400 MG SYRINGE ARIPIPRAZOLE 0.04 Antipsychotics, Atypical ABILIFY MAINTENA ER 400 MG VIAL ARIPIPRAZOLE 0.04 Antipsychotics, Atypical ABILIFY MYCITE 10 MG KIT ARIPIPRAZOLE 1 Antipsychotics, Atypical ABILIFY MYCITE 15 MG KIT ARIPIPRAZOLE 1 Antipsychotics, Atypical ABILIFY MYCITE 2 MG KIT ARIPIPRAZOLE 1 Antipsychotics, Atypical ABILIFY MYCITE 20 MG KIT ARIPIPRAZOLE 1 Antipsychotics, Atypical ABILIFY MYCITE 30 MG KIT ARIPIPRAZOLE 1 Antipsychotics, Atypical ABILIFY MYCITE 5 MG KIT ARIPIPRAZOLE 1 Antivirals, Herpes ABREVA 10% -

Mississippi Division of Medicaid Universal Preferred Drug List
MISSISSIPPI DIVISION OF MEDICAID EFFECTIVE 01/01/2021 UNIVERSAL PREFERRED DRUG LIST Version 2021.13a Updated: 8-30-2021 (For All Medicaid, MSCAN and CHIP Beneficiaries) Conduent’s SmartPA Pharmacy Application (SmartPA) is a proprietary electronic prior authorization system used for Medicaid fee for service claims. MSCAN plans may/may not -have electronic PA functionality. However, they must adhere to Medicaid’s PA criteria. THERAPEUTIC PREFERRED AGENTS NON-PREFERRED AGENTS PA CRITERIA DRUG CLASS ACNE AGENTS ANTI-INFECTIVE clindamycin gel (generic Cleocin-T) ACZONE (dapsone) Maximum Age Limit clindamycin lotion AKNE-MYCIN (erythromycin) • 21 years – all agents except clindamycin solution azelaic acid isotretinoins AMZEEQ FOAM (minocycline) AZELEX (azelaic acid) CLEOCIN-T (clindamycin) CLINDAMYCIN PAC (clindamycin) CLINDAGEL (clindamycin) clindamycin foam clindamycin gel daily (generic Clindagel) dapsone ERY (erythromycin) ERYGEL (erythromycin) erythromycin gel, swabs, solution EVOCLIN (clindamycin) KLARON (sulfacetamide) sulfacetamide RETINOIDS RETIN-A (tretinoin) adapalene tretinoin cream AKLIEF (trifarotene) ALTRENO (tretinoin) ARAZLO (tazarotene) ATRALIN (tretinoin) AVITA (tretinoin) DIFFERIN (adapalene) FABIOR (tazarotene) PLIXDA (adapalene) 1 Drug coverage subject to the rules and regulations set forth in Sec. 1927 of Social Security Act.This is not an all-inclusive list of available covered drugs and includes only managed categories. Unless otherwise stated, the listing of a particular brand or generic name includes all dosage forms of that drug. NR indicates a new drug that has not yet been reviewed by the P&T Committee. PREFERRED BRANDS will not count toward the two brand monthly Rx limit. Drugs highlighted in yellow denote a change in PDL status. An * denotes existing users will be grandfathered; grandfathering is defined as approving a Non-Preferred agent for an existing user; all other changes will not qualify for grandfathering. -
Third Quarter 2017 Update
JULY 2017 THIRD QUARTER 2017 UPDATE CHANGES TO THE HIGHMARK DRUG FORMULARIES Following is the Third Quarter 2017 update to the Highmark Drug Formularies and pharmaceutical management procedures. The formularies and pharmaceutical management procedures are updated on a quarterly basis, and the following changes reflect the decisions made in May 2017 by our Pharmacy and Therapeutics Committee. These updates are effective on the dates noted throughout this document. Please reference the guide below to navigate this communication: Section I. Highmark Commercial and Healthcare Reform Formularies A. Changes to the Highmark Comprehensive Formulary and the Highmark Comprehensive Healthcare Reform Formulary B. Changes to the Highmark Progressive Formulary and the Highmark Progressive Healthcare Reform Formulary C. Changes to the Highmark Healthcare Reform Essential Formulary D. Updates to the Pharmacy Utilization Management Programs 1. Prior Authorization Program 2. Managed Prescription Drug Coverage (MRxC) Program 3. Quantity Level Limit (QLL) Programs Section II. Highmark Medicare Part D Formularies A. Changes to the Highmark Medicare Part D 5-Tier Incentive Formulary B. Changes to the Highmark Medicare Part D 5-Tier Closed Formulary C. Additions to the Specialty Tier D. Updates to the Pharmacy Utilization Management Programs 1. Prior Authorization Program 2. Managed Prescription Drug Coverage (MRxC) Program 3. Quantity Level Limit (QLL) Program As an added convenience, you can also search our drug formularies and view utilization management policies on the Provider Resource Center (accessible via NaviNet® or our website). Click the Pharmacy/Formulary Information link from the menu on the left Highmark Blue Shield is an independent licensee of the Blue Cross and Blue Shield Association. -

Xermelo (Telotristat Ethyl)
Prior Authorization Criteria Xermelo (telotristat ethyl) Policy Number: C16325-A CRITERIA EFFECTIVE DATES: ORIGINAL EFFECTIVE DATE LAST REVIEWED DATE NEXT REVIEW DUE BY OR BEFORE 7/2019 12/2/2020 1/26/2022 HCPCS CODING TYPE OF CRITERIA LAST P&T APPROVAL/VERSION J8499 (NOC) RxPA Q1 2021 20210127C16325-A PRODUCTS AFFECTED: Xermelo (telotristat ethyl) DRUG CLASS: Tryptophan hydroxylase inhibitor ROUTE OF ADMINISTRATION: oral PLACE OF SERVICE: Retail Pharmacy AVAILABLE DOSAGE FORMS: 250mg tablets FDA-APPROVED USES: for the treatment of carcinoid syndrome diarrhea in combination with somatostatin analog (SSA) therapy in adults inadequately controlled by SSA therapy COMPENDIAL APPROVED OFF-LABELED USES: None COVERAGE CRITERIA: INITIAL AUTHORIZATION DIAGNOSIS: Carcinoid syndrome diarrhea REQUIRED MEDICAL INFORMATION: A. CARCINOID SYNDROME DIARRHEA: 1. Documentation of member has a carcinoid/neuroendocrine tumor and has a diagnosis of carcinoid syndrome AND 2. Member has been receiving therapy with the FDA-approved maximum (or highest tolerated) dose of a somatostatin analog therapy (SSA) (i.e., octreotide solution/depot or lanreotide depot) for at least 3 months AND 3. Member will continue to receive this SSA therapy in combination with Xermelo; AND 4. Member has had an inadequate response to antidiarrheals (e.g., loperamide); Molina Healthcare, Inc. confidential and proprietary © 2021 This document contains confidential and proprietary information of Molina Healthcare and cannot be reproduced, distributed, or printed without written permission -

XERMELO, INN-Telotristat-Epitrate
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 This medicinal product is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse reactions. See section 4.8 for how to report adverse reactions. 1. NAME OF THE MEDICINAL PRODUCT Xermelo 250 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each film-coated tablet contains telotristat etiprate equivalent to 250 mg telotristat ethyl. Excipient with known effect Each tablet contains 168 mg of lactose. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet. White to off-white film-coated oval tablets (approximately 17 mm long by 7.5 mm wide) with ‘T-E’ debossed on one side and ‘250’ debossed on the other side. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Xermelo is indicated for the treatment of carcinoid syndrome diarrhoea in combination with somatostatin analogue (SSA) therapy in adults inadequately controlled by SSA therapy. 4.2 Posology and method of administration Posology The recommended dose is 250 mg three times daily (tid). Available data suggest that clinical response is usually achieved within 12 weeks of treatment. It is recommended to reassess the benefit of continued therapy in a patient not responding within this time period. Based on the high inter-subject variability observed, accumulation in a subset of patients with carcinoid syndrome cannot be excluded. Therefore, intake of higher doses is not recommended (see section 5.2). Missed doses In the event of a missed dose, patients should take their subsequent dose at the next scheduled time point. -

Minutes of the CHMP Meeting 11-14 November 2019
27 January 2020 EMA/CHMP/5161/2020 Inspections, Human Medicines Pharmacovigilance and Committees Division Committee for medicinal products for human use (CHMP) Final Minutes for the meeting on 11-14 November 2019 Chair: Harald Enzmann – Vice-Chair: Bruno Sepodes Disclaimers Some of the information contained in the minutes is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scopes listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also vary during the course of the review. Additional details on some of these procedures will be published in the CHMP meeting highlights once the procedures are finalised and start of referrals will also be available. Of note, the minutes are a working document primarily designed for CHMP members and the work the Committee undertakes. Note on access to documents Some documents mentioned in the minutes cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on- going procedures for which a final decision has not yet been adopted. They will become public when adopted or considered public according to the principles stated in the Agency policy on access to documents (EMA/127362/2006). Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2019. -
2020 NANETS Guidelines Compendium
NANETS GUIDELINES 2020 TABLE OF CONTENTS Introduction ............................................................................................................................. 3 NANETS Overview .................................................................................................................... 4 Consensus Guidelines for Surveillance and Medical Management of Pancreatic Neuroendocrine Tumors (2020)................................................. 5 Consensus Paper on the Surgical Management of Pancreatic Neuroendocrine Tumors (2020) ..................................................................... 34 NANETS/SNMMI Consensus Statement on Patient Selection and Appropriate Use of 177Lu-DOTATATEPeptide Receptor Radionuclide Therapy (2020) ............................. 83 NANETS/SNMMI Procedure Standard for Somatostatin Receptor Based Peptide Receptor Radionuclide Therapy with 177Lu-DOTATATE (2019) ............................... 94 The Surgical Management of Small Bowel Neuroendocrine Tumors (2017) ..................................................................... 105 Consensus Guidelines for Surveillance and Medical Management of Midgut Neuroendocrine Tumors (2017) ................................................... 131 Appropriate Use Criteria for Somatostatin Receptor PET Imaging in Neuroendocrine Tumors (Joint with SNMMI, 2017) .................................. 143 Consensus Guidelines for the Management and Treatment of Neuroendocrine Tumors (2013)............................................................ -

XERMELO Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION -------------------------------CONTRAINDICATIONS---------------------------- These highlights do not include all the information needed to use None. (4) XERMELO safely and effectively. See full prescribing information for XERMELO. -----------------------WARNINGS AND PRECAUTIONS----------------------- Constipation: Xermelo reduces bowel movement frequency; monitor patients XERMELO (telotristat ethyl) tablets, for oral use for constipation and/or severe persistent or worsening abdominal pain. Initial U.S. Approval: 2017 Discontinue Xermelo if severe constipation or abdominal pain develops. (5.1) ----------------------------INDICATIONS AND USAGE--------------------------- ------------------------------ADVERSE REACTIONS------------------------------ Xermelo is a tryptophan hydroxylase inhibitor indicated for the treatment of Most common adverse reactions (≥5%) are nausea, headache, increased GGT, carcinoid syndrome diarrhea in combination with somatostatin analog (SSA) depression, flatulence, decreased appetite, peripheral edema, and pyrexia. therapy in adults inadequately controlled by SSA therapy. (1) (6.1) ----------------------DOSAGE AND ADMINISTRATION---------------------- To report SUSPECTED ADVERSE REACTIONS, contact Lexicon • The recommended dosage of Xermelo in adult patients is 250 mg three Pharmaceuticals, Inc. at 1-844-539-7427 or FDA at 1-800-FDA-1088 or times daily for patients whose diarrhea is inadequately controlled by a www.fda.gov/medwatch SSA therapy. (2) • Take Xermelo with food. -
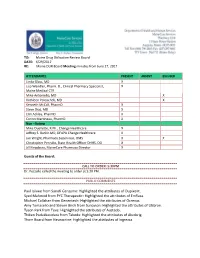
Highlighted the Attributes of Dupixent. Syed Mahmod from PYC Therapeutic: Highlighted the Attributes of Emflaza
TO: Maine Drug Utilization Review Board DATE: 6/29/2017 RE: Maine DUR Board Meeting minutes from June 27, 2017 ATTENDANCE PRESENT ABSENT EXCUSED Linda Glass, MD X Lisa Wendler, Pharm. D., Clinical Pharmacy Specialist, X Maine Medical CTR Mike Antoniello, MD X Kathleen Polonchek, MD X Kenneth McCall, PharmD X Steve Diaz, MD X Erin Ackley, PharmD. X Corinn Martineau, PharmD. X Non –Voting Mike Ouellette, R.Ph., Change Healthcare X Jeffrey S. Barkin MD, DFAPA Change Healthcare X Jan Wright, Pharmacy Supervisor, OMS X X Christopher Pezzullo, State Health Officer DHHS, DO X Jill Kingsbury, MaineCare Pharmacy Director X Guests of the Board: CALL TO ORDER: 5:30PM Dr. Pezzullo called the meeting to order at 5:30 PM. PUBLIC COMMENTS Paul Isikwe from Sanofi Genzyme: Highlighted the attributes of Dupixent. Syed Mahmod from PYC Therapeutic: Highlighted the attributes of Emflaza. Michael Callahan from Genentech: Highlighted the attributes of Ocrevus. Amy Tomasello and Steven Birch from Sunovion: Highlighted the attributes of Utibron. Tyson Park from Teva: Highlighted the attributes of Austedo. Thiken Padukkavidara from Takeda: Highlighted the attributes of Alunbrig. Thom Board from Neurocrine: Highlighted the attributes of Ingrezza. OLD BUSINESS DUR MINUTES The June DUR meeting minutes were accepted as written. MAINECARE UPDATE No update at this time. ELIDEL AND PROTOPIC PREFERED Last meeting conversation during closed session discussed moving Elidel and Protopic to preferred but was not voted on during open session. Motion was made to make Elidel and Protopic preferred. Board Decision: The Board unanimously approved the above motion. RETRO-DUR ADDITIONAL DATA ON CO-PRESCRIBING OF STIMULANTS, BENZODIAZEPINES AND Z DRUGS Stimulants have been shown to markedly improve the symptoms of ADD and ADHD. -

Second Quarter 2019 Update: Changes to the Highmark Drug Formularies
APRIL 2019 SECOND QUARTER 2019 UPDATE CHANGES TO THE HIGHMARK DRUG FORMULARIES Following is the Second Quarter 2019 update to the Highmark Drug Formularies and pharmaceutical management procedures. The formularies and pharmaceutical management procedures are updated on a quarterly basis, and the following changes reflect the decisions made in January 2019 by our Pharmacy and Therapeutics Committee. These updates are effective on the dates noted throughout this document. Please reference the guide below to navigate this communication: Section I. Highmark Commercial and Healthcare Reform Formularies A. Changes to the Highmark Comprehensive Formulary and the Highmark Comprehensive Healthcare Reform Formulary B. Changes to the Highmark Progressive Formulary and the Highmark Progressive Healthcare Reform Formulary C. Changes to the Highmark Healthcare Reform Essential Formulary D. Changes to the Highmark National Select Formulary E. Updates to the Pharmacy Utilization Management Programs 1. Prior Authorization Program 2. Managed Prescription Drug Coverage (MRxC) Program 3. Formulary Program 4. Quantity Level Limit (QLL) Programs Section II. Highmark Medicare Part D Formularies A. Changes to the Highmark Medicare Part D 5-Tier Incentive Formulary B. Changes to the Highmark Medicare Part D 5-Tier Closed Formulary C. Additions to the Specialty Tier D. Updates to the Pharmacy Utilization Management Programs 1. Prior Authorization Program 2. Managed Prescription Drug Coverage (MRxC) Program 3. Formulary Program 4. Quantity Level Limit (QLL) Program As an added convenience, you can also search our drug formularies and view utilization management policies on the Provider Resource Center (accessible via NaviNet® or our website). Click the Pharmacy Program/Formularies link from the menu on the left.