Download (Pdf)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Financial Stability Report
CENTRAL BANK OF THE REPUBLIC OF ARMENIA FINANCIAL STABILITY REPORT 2017 2018 1 This Financial Stability Report presents an assessment of potential risks that could threaten the stability of financial system of the Republic of Armenia as well as the capacity of the financial system to absorb such risks. More detailed information on Armenia’s macroeconomic environment and financial system analysis is available in the Central Bank’s periodicals, such as Status Report on Monetary Policy Implementation and Armenian Financial System: Development, Regulation, and Supervision. The data published in this report are as of 15.04.2018 The Central Bank of the Republic of Armenia Vazgen Sargsyan 6, Yerevan 0010 Phone: (374 10) 58 38 41 Fax: (374 10) 52 38 52 Internet website: www.cba.am 2 TABLE OF CONTENTS Preface ............................................................................................................................................ 5 1. Developments in the Global Economy ........................................................................................ 8 1.1. Macroeconomic Environment ......................................................................................... 8 1.2. International Financial Markets ...................................................................................... 12 2. Macroeconomic Environment Developments in Armenia ............................................................ 14 2.1. Macroeconomic Developments ......................................................................................14 -

ITU Operational Bulletin
ITU Operational Bulletin www.itu.int/itu-t/bulletin No. 1161 1.XII.2018 (Information received by 21 November 2018) ISSN 1564-5223 (Online) Place des Nations CH-1211 Standardization Bureau (TSB) Radiocommunication Bureau (BR) Genève 20 (Switzerland) Tel: +41 22 730 5211 Tel: +41 22 730 5560 Tel: +41 22 730 5111 Fax: +41 22 730 5853 Fax: +41 22 730 5785 E-mail: [email protected] E-mail: [email protected] / [email protected] E-mail: [email protected] Table of Contents Page GENERAL INFORMATION Lists annexed to the ITU Operational Bulletin: Note from TSB ...................................................................... 3 Approval of ITU-T Recommendations ............................................................................................................ 4 The International Public Telecommunication Numbering Plan (Recommendation ITU-T E.164 (11/2010)): Notes from TSB .................................................................... 5 The International Identification Plan for Public Networks and Subscriptions (Recommendation ITU-T E.212 (09/2016)): Notes from TSB .................................................................... 6 Telephone Service: Gambia (Public Utilities Regulatory Authority (PURA), Serrekunda) ........................................................ 7 Service Restrictions ........................................................................................................................................ 11 Call – Back and alternative calling procedures (Res. 21 Rev. PP – 2006) ...................................................... -

Liste Des Nouvelles Destinations Roaming Au Cameroun
POSTPAID Country Operator Outbound 1 New-Zealand Vodafone New-Zealand Live 2 Albania Vodafone Albania Live 3 Algerie Optimum Telecom Algeria Spa Live 4 Algerie Wataniya Télécom Algérie Live 5 Angola Unitel S.A. Live 6 Armenia MTS Armenia CJSC Live 7 Armenia UCOM LLC Live 8 Armenia VEON Armenia CJSC/ArmenTel Live 9 Australia Vodafone Hutchison Australia Pty Limited Live 10 Australia SingTel Optus Pty Limited Live 11 Australia Vodafone Hutchison Australia Pty Limited Live 12 Austria A1 Telekom Austria AG Live 13 Austria Hutchison Drei Austria GmbH Live 14 Azerbaijan Azerfon LLC Live 15 Azerbaijan Bakcell Limited Liable Company Live 16 Bahrain Zain Bahrain B.S.C Live 17 Bangladesh Grameenphone Ltd Live 18 Belgium Telenet Group BVBA/SPRL Live 19 Belgium ORANGE Belgium nv/SA Live 20 Belgium Proximus PLC Live 21 Benin Etisalat Benin SA Live 22 Benin Spacetel-Benin Live 23 Botswana Orange Botswana (Pty) Ltd Live 24 Brazil Claro S.A Live 25 Brazil TIM Celular S.A. Live 26 Brazil TIM Celular S.A. Live 27 Brazil TIM Celular S.A. Live 28 Bulgaria Telenor Bulgaria EAD Live 29 Burkina Faso Orange Burkina Faso S.A Live 30 Burkina Faso Onatel Live 31 Burkina Faso Telecel Faso S.A. Live 32 Burundi Africell PLC Company Live 33 Burundi Econetleo Live 34 Burundi Africell Live 35 Burundi Lacell SU Live 36 Cambodge metfone/Viettel Live 37 Cambodia Smart Axiata Co., Ltd. Live 38 Canada Rogers Communications Canada Inc. Live 39 Canada Rogers Communications Canada Inc. Live 40 Canada Bell Mobility Inc. Live 41 Canada TELUS Communications Inc. -

Translitterering Och Alternativa Geografiska Namnformer
TRANSLITTERERING OCH ALTERNATIVA GEOGRAFISKA NAMNFORMER Version XX, 27 juli 2015, Stefan Nordblom 1 FÖRORD För många utländska egennamn, i första hand personnamn och geografiska namn, finns det på svenska väl etablerade namnformer. Om det inte finns någon sådan kan utländska egennamn dock vålla bekymmer vid översättning till svenska. Föreliggande material är tänkt att vara till hjälp i sådana situationer och tar upp fall av translitterering1 och transkribering2 samt exonymer3 . Problemen uppstår främst på grund av att olika språk har olika system för translitterering och transkribering från ett visst språk och på grund av att orter kan ha olika namn på olika utländska språk. Eftersom vi oftast översätter från engelska och franska innehåller sammanställningen även translittereringar och exonymer på engelska och franska (samt tyska). Man kan alltså i detta material göra en sökning på sådana namnformer och komma fram till den svenska namnformen. Om man t.ex. i en engelsk text träffar på det geografiska namnet Constance kan man söka på det namnet här och då få reda på att staden (i detta fall på tyska och) på svenska kallas Konstanz. Den efterföljande sammanställningen bygger i huvudsak på följande källor: Institutet för de inhemska språken (FI): bl.a. skriften Svenska ortnamn i Finland - http://kaino.kotus.fi/svenskaortnamn/ Iate (EU-institutionernas termbank) Nationalencyklopedin Nationalencyklopedins kartor Interinstitutionella publikationshandboken - http://publications.europa.eu/code/sv/sv-000100.htm Språkbruk (Tidskrift utgiven av Svenska språkbyrån i Helsingfors) Språkrådet© (1996). Publikation med rekommendationer i term- och språkfrågor som utarbetas av rådets svenska översättningsenhet i samråd med övriga EU-institutioner. TT-språket - info.tt.se/tt-spraket/ I de fall uppgifterna i dessa källor inte överensstämmer med varandra har det i enskilda fall varit nödvändigt att väga, välja och sammanjämka namnförslagen, varvid rimlig symmetri har eftersträvats. -

Operátor Stát MTN Afghanistan Afghanistan Afghan Wireless
Operátor Stát MTN Afghanistan Afghanistan Afghan Wireless Communications Company Afghanistan Etisalat Afghanistan Telecom Development Company Limited Afghanistan Telekom Albania Sh.A Albania ALBtelecom sh.a. Albania Vodafone Albania Sh.A. Albania ATM Mobilis Algeria OPTIMUM TELECOM ALGERIE Spa Algeria Wataniya Algeria s.p.a. Algeria Andorra Telecom, S.A.U. Andorra Unitel Angola Angola Cable & Wireless Anguilla Anguilla APUA imobile (former APUA PCS Ltd.) Antigua and Barbuda Cable & Wireless Antigua Antigua and Barbuda TELECOM ARGENTINA S.A Argentina AMX Argentina S.A. Argentina NII Holdings, Inc. (Nextel Argentina S.R.L.) Argentina Telefonica Moviles Argentina S.A. Argentina VEON Armenia CJSC Armenia MTS Armenia CJSC Armenia Karabakh Telecom Armenia New Millennium Telecom Services NV Aruba Servicio di Telecomunicacion di Aruba (SETAR) N.V. Aruba Telstra Corporation Limited Australia Yes Optus Australia Vodafone Hutchison Australia Pty Limited Australia Hutchison Drei Austria GmbH Austria Hutchison Drei Austria GmbH Austria A1 Telekom Austria AG Austria T-Mobile Austria GmbH Austria A1 Telekom Austria AG Austria A1 Telekom Austria AG Austria T-Mobile Austria GmbH Austria Azercell Telekom B.M. Azerbaijan Azerfon LLC Azerbaijan Bakcell LLC Azerbaijan BTC Bahamas Bahamas Bahrain Telecommunication Company Bahrain Zain Bahrain B.S.C Bahrain Viva Bahrain Robi Axiata Limited Bangladesh Banglalink Digital Communications Ltd. Bangladesh GrameenPhone Limited Bangladesh Teletalk Bangladesh Limited Bangladesh Cable & Wireless Barbados Barbados Mobile TeleSystems Belarus Belarusian Telecommunications Network CJSC Belarus FE VELCOM Belarus Telenet Group BVBA/SPRL Belgium Telenet Group BVBA/SPRL Belgium Orange Belgium SA/NV Belgium Proximus PLC (former Belgacom SA/NV) Belgium Belize Telemedia Limited Belize Etisalat Benin Benin Spacetel-Benin S.A. -

Earnings Release 1Q21 Results
Earnings Release 1Q21 results 29 APRIL 2 0 2 1 STRONG PERFORMANCE ACROSS THE GROUP SEES VEON RAISE FULL YEAR GUIDANCE 2 Earnings Release 1Q21 results Amsterdam (29 April 2021) - VEON Ltd. (VEON) announces results for the first quarter ended 31 March 2021: 1Q21 HIGHLIGHTS: • Acceleration of Group revenue and EBITDA growth on a local currency basis despite one less day in 1Q21 compared to 1Q20 • Beeline Russia reporting full quarter growth, with 1Q21 revenues up 1.4% YoY with one less trading day • Ukraine, Kazakhstan and Pakistan in aggregate reporting +13.4% YoY revenue growth, beating their inflation rate • Digital services continue to expand their reach, with more than 23 million monthly active users across our products • Continued progress in optimizing our capital structure with a lower cost of debt and lengthened maturities for our funding • FY2021 guidance increased to mid-single-digit revenue and EBITDA local currency growth, from previous guidance of low to mid-single-digit revenue and EBITDA local currency growth - Q1 results at upper end of full-year guidance. The 4.3% YoY growth in Group total revenues in local currency in 1Q21 indicates an acceleration of growth, following 1.4% YoY growth that the Group recorded in 4Q20. Reported revenues declined 5.1% due to currency headwinds. In Russia we saw further improvement in revenue trends, with 1Q21 YoY local currency growth of 1.4% being the third successive quarter of improving revenue trends. - Group EBITDA increased by 4.4% YoY in local currency terms, while reported Group EBITDA declined 4.9% YoY due to adverse currency movements. -

Tunus'ta Arap Bahari
Dayı T.C. SÜLEYMAN DEMİRELÜNİVERSİTESİ SOSYAL BİLİMLER ENSTİTÜSÜ KAMU YÖNETİMİ ANABİLİM DALI TUNUS’TA ARAP BAHARI: FRANSA’NIN TUNUS YAŞAMINA ETKİSİ ÜZERİNDEN BİR DEĞERLENDİRME Bülent KARAATLI DOKTORA TEZİ DANIŞMAN Prof.Dr. Murat OKÇU ISPARTA 2015 T.C. SÜLEYMAN DEMİRELÜNİVERSİTESİ SOSYAL BİLİMLER ENSTİTÜSÜ KAMU YÖNETİMİ ANABİLİM DALI TUNUS’TA ARAP BAHARI: FRANSA’NIN TUNUS YAŞAMINA ETKİSİ ÜZERİNDEN BİR DEĞERLENDİRME Bülent KARAATLI 0740203055 DOKTORA TEZİ DANIŞMAN Prof.Dr. Murat OKÇU ISPARTA 2015 ii ii ÖZET TUNUS’TA ARAP BAHARI: FRANSA’NIN TUNUS YAŞAMINA ETKİSİ ÜZERİNDEN BİR DEĞERLENDİRME Bülent KARAATLI Süleyman Demirel Üniversitesi, Kamu Yönetimi Bölümü Doktora Tezi 454 sayfa, Haziran 2015. Danışman: Prof.Dr. Murat OKÇU “Arap Baharı” olarak anılan Kuzey Afrika ve Ortadoğu’daki olaylar, Tunus’ta başlamış, müteakiben Mısır, Cezayir, Fas, Libya, Yemen, Bahreyn, Suudi Arabistan, Ürdün, Umman, Suriye ve Kuveyt’e sıçramıştır. Olaylar, ülkelerin sahip oldukları kendine özgü toplumsal kültür, siyasi birikim, tecrübe, kurumsal yapı gibi özellikler neticesinde her ülkede farklı bir yönde evrilmiş ve süreç her ülkede farklı yaşanmıştır. Tunus’ta, diğer ülkelerle karşılaştırıldığında daha az şiddetin ve ölümün yaşandığı olaylar sonucu Cumhurbaşkanı Bin ALİ yönetimi bırakmak zorunda kalmış, geçici hükümet kurulmuş, Kurucu Meclis seçimleri yapılmış ve bu seçimler bu sürecin içerisinde yer alan ülkelerde yapılan ilk serbest ve adil seçimler olarak tarihe geçmiştir. Kurucu Meclis öncülüğünde kurulan Anayasa Komisyonu ülkedeki her kesime hitap eden ve eski tecrübelerden ders alınarak hazırlanan Anayasayı tamamlamıştır. Müteakiben de Tunus bu anayasaya göre yeni Başbakan ve Cumhurbaşkanını seçerek hem bölge ülkelerine örnek olmuş hem de diğer ülkelerden farklılığını ortaya koymuştur. Çalışma, Tunus’un tüm bu farklılığı kazanmasında tarihi süreç içerisinde Fransa ile karşılıklı ilişkiler sonucu oluşan eğitimli ve güçlü orta sınıf, kendine özgü sosyal ve siyasi kültür, tecrübe ve kurumsal yapı gibi özelliklerin etkisinin büyük olduğu savıyla yapılmıştır. -
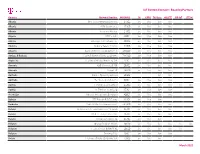
Iot Custom Connect - Roaming Partners
IoT Custom Connect - Roaming Partners Country Column1 Network Provider Column2MCCMNCColumn10 Column32G Column4GPRS Column53G Data Column64G/LTE Column7NB-IoT LTE-M Albania One Telecommunications sh.a 27601 live live live live Albania ALBtelecom sh.a. 27603 live live live live Albania Vodafone Albania 27602 live live live live Algeria ATM Mobilis 60301 live live live live Algeria Wataniya Telecom Algerie 60303 live live live live Andorra Andorra Telecom S.A.U. 21303 live live live live Anguilla Cable and Wireless (Anguilla) Ltd 365840 live live live live Antigua & Barbuda Cable & Wireless (Antigua) Limited 344920 live live live live Argentina Telefónica Móviles Argentina S.A. 72207 live live live live Armenia VEON Armenia CJSC 28301 live live live live Armenia Ucom LLC 28310 live live live live Australia SingTel Optus Pty Limited 50502 live live Australia Telstra Corporation Ltd 50501 live live live live Austria T-Mobile Austria GmbH 23203 live live live live live live Austria A1 Telekom Austria AG 23201 live live live live Azerbaijan Bakcell Limited Liable Company 40002 live live live live Bahrain STC Bahrain B.S.C Closed 42604 live live live Barbados Cable & Wireless Barbados Ltd. 342600 live live live live Belarus Belarusian Telecommunications Network 25704 live live live live Belarus Mobile TeleSystems JLLC 25702 live live live live Belarus Unitary Enterprise A1 25701 live live live Belgium Orange Belgium NV/SA 20610 live live live live live live Belgium Telenet Group BVBA/SPRL 20620 live live live live live Belgium Proximus PLC 20601 live live live live Bolivia Telefonica Celular De Bolivia S.A. 73603 live live live March 2021 IoT Custom Connect - Roaming Partners Country Column1 Network Provider Column2MCCMNCColumn10 Column32G Column4GPRS Column53G Data Column64G/LTE Column7NB-IoT LTE-M Bosnia and Herzegovina PUBLIC ENTERPRISE CROATIAN TELECOM Ltd. -

Earnings Release 2Q21 Results
Earnings Release 2Q21 results 3 0 AUGUST 2021 STRONG GROWTH IN REVENUE AND EBITDA ACROSS THE GROUP FULL-YEAR 2021 REVENUE AND EBITDA GUIDANCE RAISED 2 Earnings Release 2Q21 results Amsterdam (30 August 2021) - VEON Ltd. (VEON) announces results for the second quarter ended 30 June 2021: 2Q21 HIGHLIGHTS: • A return to growth of Group revenue and EBITDA on a reported basis and continued acceleration on a local currency basis • Beeline Russia reports growth in total revenue, service revenue and EBITDA, up in local currency terms 6.2%, 2.7% and 2.2% YoY respectively • Strong revenue performance on a local currency basis for the Group • Digital services continue to expand their reach, with more than 38 million monthly active users across our digital product offerings • Continued progress in optimizing our capital structure, lowering cost of debt, lengthening maturities and increasing local currency funding • FY2021 revenue guidance increased to high single-digit growth, and FY2021 EBITDA guidance increased to mid to high single-digit growth on a local currency basis - Strong 2Q21 Group results, with reported revenues up 9.2% YoY, with growth in local currency revenues of 11.3% YoY; an acceleration from the 4.2% YoY growth recorded in 1Q21. Russia did show improved execution in its quarterly revenue trends, with 2Q21 local currency growth of 6.2% YoY. - Reported Group EBITDA increased by 8.7% YoY, while in local currency terms EBITDA increased 10.7% YoY. This solid result was driven by robust local-currency EBITDA performance in Ukraine (+17% YoY), Kazakhstan (+21% YoY) and Pakistan (+14.5% YoY). -

Annual Report 2019 VEON Ltd
Annual Report 2019 VEON Ltd. Claude Debussylaan 88, 1082 MD Amsterdam The Financial Statements are approved by the Audit Committee on behalf of the Board on March 13, 2020 TABLE OF CONTENTS Director's Report............................................................................................................................................................... 3 Information on the Company........................................................................................................................................... 4 Directors and Senior Management and Employees........................................................................................................ 33 Major Shareholders and Related Party Transactions...................................................................................................... 41 How We Manage Risks................................................................................................................................................... 43 Risk factors ..................................................................................................................................................................... 46 Operating and Financial Review and Prospects ............................................................................................................. 71 Additional Information ..................................................................................................................................................... 93 Quantitative and Qualitative Disclosures -

Earnings Release 4Q20 Results
Earnings Release 4Q20 results 18 FEBRUARY 2021 DELIVERING ON EXPECTATIO NS BACK TO GROWTH IN AN UNEXPECTED YEAR 1 Earnings Release 4Q20 results Amsterdam (18 February 2021) - VEON Ltd.(VEON) announces results for the fourth quarter ended 31 Dec 2020: 2020 HIGHLIGHTS: • VEON’s recovery continued as growth on a local currency basis returned in the fourth quarter, amidst unprecedented challenges • Group performance and cost structure were improved by streamlining HQ, empowering local operations and enhancing governance • VEON executed on a record network rollout, driving growth in 4G users of 34% YoY, (+20 million). Data revenues grew by 15.0% YoY in local currency • Portfolio optimization remained a focus, as shown by our exit from Armenia. Further opportunities to unlock value are being explored 2020 saw the global telecoms industry facing unprecedented challenges, as we battled the COVID pandemic with the associated lockdowns and faced a material slowdown in economies. During this time, VEON stepped-up support to our over 200 million customers, addressing their changing demands associated with the new normal • During the last year, the group concluded a major transformation from a centralized entity to a structure with fully empowered country operations governed by the local operating boards. This has enabled us to further strengthen the governance and expedite the decision- making processes across all local business lines • The Group delivered FY 2020 results in line with guidance, with full-year revenue of USD 7,980 million (down 1.6% YoY in local currency) and EBITDA Adj. of USD 3,453 million (down 2.1% YoY in local currency). -
List of Issuer Identifier Numbers for the International Telecommunication Charge Card (In Accordance with Recommendation Itu-T E.118 (05/2006))
Annex to ITU Operational Bulletin No. 1161 – 1.XII.2018 INTERNATIONAL TELECOMMUNICATION UNION TSB TELECOMMUNICATION STANDARDIZATION BUREAU OF ITU _____________________________________________________________________ LIST OF ISSUER IDENTIFIER NUMBERS FOR THE INTERNATIONAL TELECOMMUNICATION CHARGE CARD (IN ACCORDANCE WITH RECOMMENDATION ITU-T E.118 (05/2006)) (POSITION ON 1 DECEMBER 2018) ______________________________________________________________________ Geneva, 2018 List of Issuer Identifier Numbers for the international Telecommunication charge card (In accordance with Recommendation ITU-T E.118) Note from TSB This List replaces the List annexed to Operational Bulletin No. 1088 of 15.XI.2015. It contains all the Issuer Identifier Numbers (IIN) registered by the ITU, which have been notified in the ITU Operational Bulletin up to and including No. 1161 of 1.XII.2018. For your information, this List will be updated by numbered series of amendments published in the ITU Operational Bulletin. This Annex is available for free download on ITU website. An IIN is used to identify a telecommunication company in a country, which is working in an international environment. According to ISO Standard 7812-2 , the criteria for approval and rejection of applications are: "4.3.1 Criteria for approval of an application for a single IIN Applications for a single IIN shall meet all the criteria for approval below and shall not comply with any of the criteria for rejection in 4.3.2 : a) the applicant applying for a single IIN shall not already have an IIN assigned to it in its own right (outside of any card scheme); b) the IIN shall be for immediate use, preferably within 12 months of the date of issue of the IIN; c) the card being issued shall be for use in an international interchange environment (see ISO/IEC 7812-1); d) the applicant shall be a single corporate entity operating under a specific legislative regulation.