Efficacy and Delayed Discomfort of Proxymetacaine and Tetracaine in Its Use in Intravitreal Ranibizumab Injections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

208135Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 208135Orig1s000 STATISTICAL REVIEW(S) U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research Office of Translational Sciences Office of Biostatistics S TATISTICAL R EVIEW AND E VALUATION CLINICAL STUDIES NDA/BLA #: 208135 Drug Name: Tetracaine Hydrochloride Ophthalmic Solution 0.5% (STERI-UNIT®) Indication(s): For procedures requiring a rapid and short acting ophthalmic anesthetic Applicant: Alcon research ltd Date(s): Stamp date: April 30, 2015 PDUFA date: February 29, 2016 Review Priority: Standard Biometrics Division: DBIV Statistical Reviewer: Abel Tilahun Eshete Concurring Reviewers: Yan Wang Medical Division: Ophthalmology Clinical Team: Medical Reviewer: Jennifer Harris Project Manager: Michael Puglisi Keywords: Topical anesthesia, Pain scores, Tetracaine . Reference ID: 3875889 Table of Contents 1 EXECUTIVE SUMMARY............................................................................................................................... 4 2 INTRODUCTION............................................................................................................................................. 6 2.1 OVERVIEW ................................................................................................................................................... 6 2.2 SUBMISSION HISTORY .................................................................................................................................. 6 2.3 -
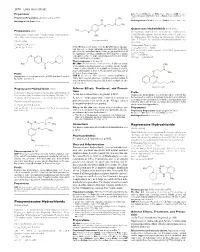
Proxymetacaine Hydrochloride Ropivacaine Hydrochloride
1870 Local Anaesthetics Preparations pore: Alcaine; Switz.: Alcaine; Turk.: Alcaine; Opticaine; USA: Ak-Taine; Alcaine; Ocu-Caine; Ophthetic; Parcaine; Venez.: Alcaine; Oftaine†; Poen- (details are given in Part 3) caina. Proprietary Preparations CH3 Multi-ingredient: Spain: Detraine. O Multi-ingredient: Canad.: Fluoracaine†; USA: Fluoracaine; Fluorocaine. N CH3 O Quinisocaine Hydrochloride (BANM, rINNM) H3C Propipocaine (rINN) O Chinisocainum Hydrochloride; Dimethisoquin Hydrochloride Propipocaína; Propipocaïne; Propipocainum; Propoxypipero- (USAN); Dimethisoquinium Chloride; Hidrocloruro de quinisocaí- NH2 caine. 3-Piperidino-4′-propoxypropiophenone. na; Quinisocaïne, Chlorhydrate de; Quinisocaini Hydrochlori- (proxymetacaine) dum. 2-(3-Butyl-1-isoquinolyloxy)-NN-dimethylethylamine hy- Пропипокаин drochloride. C17H25NO2 = 275.4. Хинизокаина Гидрохлорид CAS — 3670-68-6. NOTE. PROX is a code approved by the BP 2008 for use on single unit doses of eye drops containing proxymetacaine hydrochlo- C17H24N2O,HCl = 308.8. ride where the individual container may be too small to bear all CAS — 86-80-6 (quinisocaine); 2773-92-4 (quinisocaine the appropriate labelling information. PROXFLN is a similar hydrochloride). O code approved for eye drops containing proxymetacaine hydro- ATC — D04AB05. chloride and fluorescein sodium. ATC Vet — QD04AB05. N Pharmacopoeias. In Br. and US. BP 2008 (Proxymetacaine Hydrochloride). A white or almost H3C CH3 white, odourless or almost odourless, crystalline powder. Soluble O in water and in chloroform; very soluble in dehydrated alcohol; N practically insoluble in ether. A 1% solution in water has a pH of O CH Profile 5.7 to 6.4. Protect from light. 3 Propipocaine is a local anaesthetic (p.1850) that has been used USP 31 (Proparacaine Hydrochloride). A white to off-white, or for surface anaesthesia. -

Royal Free Hospital Drug Formulary
Royal Free Hospital Drug Formulary Title Formulary Status Section Annotation 5.3 Antiviral drugs‐>5.3.1 HIV infection‐>Nucleoside reverse ABACAVIR On Formulary transcriptase inhibitors As per HIV guidelines. Abidec® On Formulary 9.6 Vitamins‐>9.6.7 Multivitamin preparations 4.10 Drugs used in substance dependence‐>4.10.1 Alcohol ACAMPROSATE CALCIUM On Formulary dependence‐>Acamprosate 6.1 Drugs used in diabetes‐>6.1.2 Antidiabetic drugs‐>6.1.2.3 Other ACARBOSE On Formulary antidiabetic drugs 11.6 Treatment of glaucoma‐>Carbonic anhydrase inhibitors and ACETAZOLAMIDE On Formulary systemic drugs 11.8 Miscellaneous ophthalmic preparations‐>11.8.2 Ocular diagnostic and peri‐operative preparations and photodynamic ACETYLCHOLINE CHLORIDE On Formulary treatment‐>Ocular peri‐operative drugs ACETYLCYSTEINE On Formulary Specific drugs‐>Analgesics (non‐opioid) Acetylcysteine On Formulary Specific drugs‐>Analgesics (non‐opioid)‐>ACETYLCYSTEINE 11.8 Miscellaneous ophthalmic preparations‐>11.8.1 Tear deficiency, ACETYLCYSTEINE On Formulary ocular lubricants, and astringents ACICLOVIR On Formulary 11.3 Anti‐infective eye preparations‐>11.3.3 Antivirals ACICLOVIR On Formulary 13.10 Anti‐infective skin preparations‐>13.10.3 Antiviral preparations 13.10 Anti‐infective skin preparations‐>13.10.3 Antiviral preparations‐ Aciclovir On Formulary >ACICLOVIR 13.5 Preparations for eczema and psoriasis‐>13.5.2 Preparations for ACITRETIN On Formulary psoriasis‐>Oral retinoids for psoriasis Removal and elimination‐>Removal from the gastro‐intestinal tract‐ Actidose‐Aqua® -

Safety Alert: Risks Associated with Ophthalmic Anesthetics
WRHA Pharmacy Program Health Sciences Centre MS-189 820 Sherbrook St. Winnipeg, Manitoba R3A 1R9 CANADA TEL: 204-787-7183 Fax: 204-787-3195 FAX: 204-787-3195 Safety Alert: Risks associated with Ophthalmic Anesthetics The self-administration of ophthalmic anesthetics by patients for the relief of eye pain should be avoided and they should not be given to patients to take home for pain relief. Vision threatening complications of topical anesthetic abuse are common. There is no indication for the use of ophthalmic anesthetics except for diagnostic and short term therapeutic purposes (the removal of a foreign body or ocular surgery) and therefore, these products should only be used under a physician’s supervision. Eye trauma resulting in a corneal abrasion (epithelial injury) is a common complaint in the Emergency department (1). A superficial corneal injury can cause intense pain causing a patient to seek medical help or immediate relief from available over the counter remedies. In Canada, only two topical ophthalmic anesthetic drugs are available commercially as single entities, proparacaine (proxymetacaine) and tetracaine (available in bottle and minim forms). Benoxinate (oxybuprocaine) is only available in combination with fluorescein (3). Lidocaine is also used in ophthalmic surgical procedures however, it is not available in the Canadian market as an ophthalmic preparation. Topical ophthalmic anesthetics function by blocking nerve conduction when applied to the cornea and conjunctiva. The ocular surface is innervated by the multiple branches of the trigeminal nerve. The cornea is supplied by the long and short ciliary nerves, the nasociliary nerve and the lacrimal nerve (4). Topical anesthetics reduce sodium permeability preventing generation and conduction of nerve impulses, increasing excitation threshold, and slowing the nerve impulse propagation. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

(12) United States Patent (10) Patent No.: US 8,026,285 B2 Bezwada (45) Date of Patent: Sep
US008O26285B2 (12) United States Patent (10) Patent No.: US 8,026,285 B2 BeZWada (45) Date of Patent: Sep. 27, 2011 (54) CONTROL RELEASE OF BIOLOGICALLY 6,955,827 B2 10/2005 Barabolak ACTIVE COMPOUNDS FROM 2002/0028229 A1 3/2002 Lezdey 2002fO169275 A1 11/2002 Matsuda MULT-ARMED OLGOMERS 2003/O158598 A1 8, 2003 Ashton et al. 2003/0216307 A1 11/2003 Kohn (75) Inventor: Rao S. Bezwada, Hillsborough, NJ (US) 2003/0232091 A1 12/2003 Shefer 2004/0096476 A1 5, 2004 Uhrich (73) Assignee: Bezwada Biomedical, LLC, 2004/01 17007 A1 6/2004 Whitbourne 2004/O185250 A1 9, 2004 John Hillsborough, NJ (US) 2005/0048121 A1 3, 2005 East 2005/OO74493 A1 4/2005 Mehta (*) Notice: Subject to any disclaimer, the term of this 2005/OO953OO A1 5/2005 Wynn patent is extended or adjusted under 35 2005, 0112171 A1 5/2005 Tang U.S.C. 154(b) by 423 days. 2005/O152958 A1 7/2005 Cordes 2005/0238689 A1 10/2005 Carpenter 2006, OO13851 A1 1/2006 Giroux (21) Appl. No.: 12/203,761 2006/0091034 A1 5, 2006 Scalzo 2006/0172983 A1 8, 2006 Bezwada (22) Filed: Sep. 3, 2008 2006,0188547 A1 8, 2006 Bezwada 2007,025 1831 A1 11/2007 Kaczur (65) Prior Publication Data FOREIGN PATENT DOCUMENTS US 2009/0076174 A1 Mar. 19, 2009 EP OO99.177 1, 1984 EP 146.0089 9, 2004 Related U.S. Application Data WO WO9638528 12/1996 WO WO 2004/008101 1, 2004 (60) Provisional application No. 60/969,787, filed on Sep. WO WO 2006/052790 5, 2006 4, 2007. -

OUH Formulary Approved for Use in Breast Surgery
Oxford University Hospitals NHS Foundation Trust Formulary FORMULARY (Y): the medicine can be used as per its licence. RESTRICTED FORMULARY (R): the medicine can be used as per the agreed restriction. NON-FORMULARY (NF): the medicine is not on the formulary and should not be used unless exceptional approval has been obtained from MMTC. UNLICENSED MEDICINE – RESTRICTED FORMULARY (UNR): the medicine is unlicensed and can be used as per the agreed restriction. SPECIAL MEDICINE – RESTRICTED FORMULARY (SR): the medicine is a “special” (unlicensed) and can be used as per the agreed restriction. EXTEMPORANEOUS PREPARATION – RESTRICTED FORMULARY (EXTR): the extemporaneous preparation (unlicensed) can be prepared and used as per the agreed restriction. UNLICENSED MEDICINE – NON-FORMULARY (UNNF): the medicine is unlicensed and is not on the formulary. It should not be used unless exceptional approval has been obtained from MMTC. SPECIAL MEDICINE – NON-FORMULARY (SNF): the medicine is a “special” (unlicensed) and is not on the formulary. It should not be used unless exceptional approval has been obtained from MMTC. EXTEMPORANEOUS PREPARATION – NON-FORMULARY (EXTNF): the extemporaneous preparation (unlicensed) cannot be prepared and used unless exceptional approval has been obtained from MMTC. CLINICAL TRIALS (C): the medicine is clinical trial material and is not for clinical use. NICE TECHNOLOGY APPRAISAL (NICETA): the medicine has received a positive appraisal from NICE. It will be available on the formulary from the day the Technology Appraisal is published. Prescribers who wish to treat patients who meet NICE criteria, will have access to these medicines from this date. However, these medicines will not be part of routine practice until a NICE TA Implementation Plan has been presented and approved by MMTC (when the drug will be given a Restricted formulary status). -

Clonidine As Adjuvant for Oxybuprocaine, Bupivacaine Or
1 Clonidine as adjuvant for oxybuprocaine, bupivacaine or dextrorphan has a significant peripheral action in intensifying and prolonging analgesia in response to local dorsal cutaneous noxious pinprick in rats Yu-Wen Chen, Ph.D.,1,2 Chin-Chen Chu, M.D., Ph.D.,3 Yu-Chung Chen, M.S.,4 Ching-Hsia Hung, Ph.D.,5,* Meng-I Hsueh, B.S.,1 Jhi-Joung Wang, M.D., Ph.D.3 1 Department of Physical Therapy, China Medical University, Taichung, Taiwan 2 Graduate Institute of Neural and Cognitive Sciences, China Medical University, Taichung, Taiwan 3 Department of Medical Research, Chi-Mei Medical Center, Tainan, Taiwan 4 Division of Physical Therapy, Department of Physical Medicine and Rehabilitation, Cheng Hsin General Hospital, Taipei, Taiwan 5 Institute & Department of Physical Therapy, National Cheng Kung University, Tainan, Taiwan *Address correspondence and reprint requests to: Ching-Hsia Hung, PhD, Department of Physical Therapy, National Cheng Kung University, No.1 Ta-Hsueh Road, Tainan, Taiwan Tel: 886-6-2353535 ext 5939 Fax: 886-6-2370411 E-mail: [email protected] 2 Abstract The aim of the study was to evaluate co-administration of clonidine with oxybuprocaine (ester type), bupivacaine (amide type) or dextrorphan (non-ester or non-amide type) and to see whether it could have a peripheral action in enhancing local anesthesia on infiltrative cutaneous analgesia in rats. Cutaneous analgesia was evaluated by a block of the cutaneous trunci muscle reflex (CTMR) in response to local dorsal cutaneous noxious pinprick in rats. The analgesic effect of the addition of clonidine with oxybuprocaine, bupivacaine or dextrorphan by subcutaneous injection was evaluated. -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -

Sodium Channel Na Channels;Na+ Channels
Sodium Channel Na channels;Na+ channels Sodium channels are integral membrane proteins that form ion channels, conducting sodium ions (Na +) through a cell's plasma membrane. They are classified according to the trigger that opens the channel for such ions, i.e. either a voltage-change (Voltage-gated, voltage-sensitive, or voltage-dependent sodium channel also called VGSCs or Nav channel) or a binding of a substance (a ligand) to the channel (ligand-gated sodium channels). In excitable cells such as neurons, myocytes, and certain types of glia, sodium channels are responsible for the rising phase of action potentials. Voltage-gated Na+ channels can exist in any of three distinct states: deactivated (closed), activated (open), or inactivated (closed). Ligand-gated sodium channels are activated by binding of a ligand instead of a change in membrane potential. www.MedChemExpress.com 1 Sodium Channel Inhibitors & Modulators (+)-Kavain (-)-Sparteine sulfate pentahydrate Cat. No.: HY-B1671 ((-)-Lupinidine (sulfate pentahydrate)) Cat. No.: HY-B1304 Bioactivity: (+)-Kavain, a main kavalactone extracted from Piper Bioactivity: (-)-Sparteine sulfate pentahydrate ((-)-Lupinidine sulfate methysticum, has anticonvulsive properties, attenuating pentahydrate) is a class 1a antiarrhythmic agent and a sodium vascular smooth muscle contraction through interactions with channel blocker. It is an alkaloid, can chelate the bivalents voltage-dependent Na + and Ca 2+ channels [1]. (+)-Kav… calcium and magnesium. Purity: 99.98% Purity: 98.0% Clinical Data: No Development Reported Clinical Data: Launched Size: 10mM x 1mL in DMSO, Size: 10mM x 1mL in DMSO, 5 mg, 10 mg 50 mg A-803467 Ajmaline Cat. No.: HY-11079 (Cardiorythmine; (+)-Ajmaline) Cat. No.: HY-B1167 Bioactivity: A 803467 is a selective Nav1.8 sodium channel blocker with an Bioactivity: Ajmaline is an alkaloid that is class Ia antiarrhythmic agent. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

2021 Equine Prohibited Substances List
2021 Equine Prohibited Substances List . Prohibited Substances include any other substance with a similar chemical structure or similar biological effect(s). Prohibited Substances that are identified as Specified Substances in the List below should not in any way be considered less important or less dangerous than other Prohibited Substances. Rather, they are simply substances which are more likely to have been ingested by Horses for a purpose other than the enhancement of sport performance, for example, through a contaminated food substance. LISTED AS SUBSTANCE ACTIVITY BANNED 1-androsterone Anabolic BANNED 3β-Hydroxy-5α-androstan-17-one Anabolic BANNED 4-chlorometatandienone Anabolic BANNED 5α-Androst-2-ene-17one Anabolic BANNED 5α-Androstane-3α, 17α-diol Anabolic BANNED 5α-Androstane-3α, 17β-diol Anabolic BANNED 5α-Androstane-3β, 17α-diol Anabolic BANNED 5α-Androstane-3β, 17β-diol Anabolic BANNED 5β-Androstane-3α, 17β-diol Anabolic BANNED 7α-Hydroxy-DHEA Anabolic BANNED 7β-Hydroxy-DHEA Anabolic BANNED 7-Keto-DHEA Anabolic CONTROLLED 17-Alpha-Hydroxy Progesterone Hormone FEMALES BANNED 17-Alpha-Hydroxy Progesterone Anabolic MALES BANNED 19-Norandrosterone Anabolic BANNED 19-Noretiocholanolone Anabolic BANNED 20-Hydroxyecdysone Anabolic BANNED Δ1-Testosterone Anabolic BANNED Acebutolol Beta blocker BANNED Acefylline Bronchodilator BANNED Acemetacin Non-steroidal anti-inflammatory drug BANNED Acenocoumarol Anticoagulant CONTROLLED Acepromazine Sedative BANNED Acetanilid Analgesic/antipyretic CONTROLLED Acetazolamide Carbonic Anhydrase Inhibitor BANNED Acetohexamide Pancreatic stimulant CONTROLLED Acetominophen (Paracetamol) Analgesic BANNED Acetophenazine Antipsychotic BANNED Acetophenetidin (Phenacetin) Analgesic BANNED Acetylmorphine Narcotic BANNED Adinazolam Anxiolytic BANNED Adiphenine Antispasmodic BANNED Adrafinil Stimulant 1 December 2020, Lausanne, Switzerland 2021 Equine Prohibited Substances List . Prohibited Substances include any other substance with a similar chemical structure or similar biological effect(s).