Chemical Structure and Mechanism of Action
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Mepivacaine Hydrochloride Injection
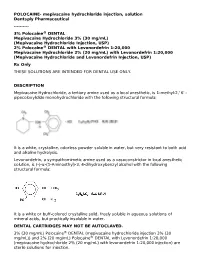
POLOCAINE- mepivacaine hydrochloride injection, solution Dentsply Pharmaceutical ---------- 3% Polocaine® DENTAL Mepivacaine Hydrochloride 3% (30 mg/mL) (Mepivacaine Hydrochloride Injection, USP) 2% Polocaine® DENTAL with Levonordefrin 1:20,000 Mepivacaine Hydrochloride 2% (20 mg/mL) with Levonordefrin 1:20,000 (Mepivacaine Hydrochloride and Levonordefrin Injection, USP) Rx Only THESE SOLUTIONS ARE INTENDED FOR DENTAL USE ONLY. DESCRIPTION Mepivacaine Hydrochloride, a tertiary amine used as a local anesthetic, is 1-methyl-2,' 6' - pipecoloxylidide monohydrochloride with the following structural formula: It is a white, crystalline, odorless powder soluble in water, but very resistant to both acid and alkaline hydrolysis. Levonordefrin, a sympathomimetic amine used as a vasoconstrictor in local anesthetic solution, is (-)-α-(1-Aminoethyl)-3, 4-dihydroxybenzyl alcohol with the following structural formula: It is a white or buff-colored crystalline solid, freely soluble in aqueous solutions of mineral acids, but practically insoluble in water. DENTAL CARTRIDGES MAY NOT BE AUTOCLAVED. 3% (30 mg/mL) Polocaine® DENTAL (mepivacaine hydrochloride injection 3% (30 mg/mL)) and 2% (20 mg/mL) Polocaine® DENTAL with Levonordefrin 1:20,000 (mepivacaine hydrochloride 2% (20 mg/mL) with levonordefrin 1:20,000 injection) are sterile solutions for injection. sterile solutions for injection. COMPOSITION: CARTRIDGE Each mL contains: 2% 3% Mepivacaine Hydrochloride 20 mg 30 mg Levonordefrin 0.05 mg - Sodium Chloride 4 mg 6 mg Potassium metabisulfite 1.2 mg - Edetate disodium 0.25 mg - Sodium Hydroxide q.s. ad pH; Hydrochloric 0.5 mg - Acid Water For Injection, qs. ad. 1 mL 1 mL The pH of the 2% cartridge solution is adjusted between 3.3 and 5.5 with NaOH. -

4% Citanest® Plain Dental (Prilocaine Hydrochloride Injection, USP) for Local Anesthesia in Dentistry
4% Citanest® Plain Dental (Prilocaine Hydrochloride Injection, USP) For Local Anesthesia in Dentistry Rx only DESCRIPTION 4% Citanest Plain Dental (prilocaine HCI Injection, USP), is a sterile, non-pyrogenic isotonic solution that contains a local anesthetic agent and is administered parenterally by injection. See INDICATIONS AND USAGE for specific uses. The quantitative composition is shown in Table 1. 4% Citanest Plain Dental contains prilocaine HCl, which is chemically designated as propanamide, N-(2- methyl-phenyl) -2- (propylamino)-, monohydrochloride and has the following structural formula: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration. The specific quantitative composition is shown in Table 1. TABLE 1. COMPOSITION Product Identification Formula (mg/mL) Prilocaine HCl pH 4% Citanest® Plain Dental 40.0 6.0 to 7.0 Note: Sodium hydroxide or hydrochloric acid may be used to adjust the pH of 4% Citanest Plain Dental Injection. CLINICAL PHARMACOLOGY Mechanism of Action: Prilocaine stabilizes the neuronal membrane by inhibiting the ionic fluxes required for the initiation and conduction of impulses, thereby effecting local anesthetic action. Onset and Duration of Action: When used for infiltration injection in dental patients, the time of onset of anesthesia averages less than 2 minutes with an average duration of soft tissue anesthesia of approximately 2 hours. Based on electrical stimulation studies, 4% Citanest Plain Dental Injection provides a duration of pulpal anesthesia of approximately 10 minutes in maxillary infiltration injections. In clinical studies, this has been found to provide complete anesthesia for procedures lasting an average of 20 minutes. When used for inferior alveolar nerve block, the time of onset of 4% Citanest Plain Dental Injection averages less than three minutes with an average duration of soft tissue anesthesia of approximately 2 ½hours. -

208135Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 208135Orig1s000 STATISTICAL REVIEW(S) U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research Office of Translational Sciences Office of Biostatistics S TATISTICAL R EVIEW AND E VALUATION CLINICAL STUDIES NDA/BLA #: 208135 Drug Name: Tetracaine Hydrochloride Ophthalmic Solution 0.5% (STERI-UNIT®) Indication(s): For procedures requiring a rapid and short acting ophthalmic anesthetic Applicant: Alcon research ltd Date(s): Stamp date: April 30, 2015 PDUFA date: February 29, 2016 Review Priority: Standard Biometrics Division: DBIV Statistical Reviewer: Abel Tilahun Eshete Concurring Reviewers: Yan Wang Medical Division: Ophthalmology Clinical Team: Medical Reviewer: Jennifer Harris Project Manager: Michael Puglisi Keywords: Topical anesthesia, Pain scores, Tetracaine . Reference ID: 3875889 Table of Contents 1 EXECUTIVE SUMMARY............................................................................................................................... 4 2 INTRODUCTION............................................................................................................................................. 6 2.1 OVERVIEW ................................................................................................................................................... 6 2.2 SUBMISSION HISTORY .................................................................................................................................. 6 2.3 -

Local Anesthetic Half Life (In Hours) Lidocaine 1.6 Mepivacaine 1.9 Bupivacaine 353.5 Prilocaine 1.6 Articaine 0.5
Local Anesthetics • The first local anesthetics History were cocaine and procaine (Novacain) developed in ltlate 1800’s • They were called “esters” because of their chemical composition • Esters had a slow onset and short half life so they did not last long History • Derivatives of esters called “amides” were developed in the 1930’s • Amides had a faster onset and a longer half life so they lasted longer • AidAmides quiklickly repldlaced esters • In dentistry today, esters are only found in topical anesthetics Generic Local Anesthetics • There are five amide anesthetics used in dentistry today. Their generic names are; – lidocaine – mepivocaine – bupivacaine – prilocaine – artica ine • Each is known by at least one brand name Brand Names • lidocaine : Xylocaine, Lignospan, Alphacaine, Octocaine • mepivocaine: Carbocaine, Arestocaine, Isocaine, Polocaine, Scandonest • prilocaine : Citanest, Citanest Forte • bibupivaca ine: MiMarcaine • articaine: Septocaine, Zorcaine About Local Anesthetic (LA) • Local anesthetic (LA) works by binding with sodium channels in neurons preventing depolarization • LA is inactivated at the injection site when it is absorbed into the blood stream and redistributed throughout the body • If enough LA is absorbed, sodium channels in other parts of the body will be blocked, causing systemic side effects About LA • A clinical effect of LAs is dilation blood vessels, speeding up absorption and distribution • To counteract this dilation so anesthesia is prolonged, , a vasoconstrictor is often added to LAs • However, vasoconstrictors have side effects also Metabolism and Excretion • Most amide LAs are metabolized (inactivated) by the liver and excreted by the kidneys. • Prilocaine is partially metabolized by the lungs • Articaine is partially metabolized by enzymes in the bloo d as well as the liver. -

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -

Hyperinflation Management Medications Requiring Prior Authorization for Medical Necessity
July 2021 Effective 07/01/2021 Hyperinflation Management Medications Requiring Prior Authorization for Medical Necessity Below is a list of medicines by drug class that will not be covered without a prior authorization for medical necessity. If you continue using one of these drugs without prior approval for medical necessity, you may be required to pay the full cost. If you are currently using one of the drugs requiring prior authorization for medical necessity, ask your d octor to choose one of the generic or brand formulary options listed below. Category * Drugs Requiring Prior Formulary Options Drug Class Authorization for Medical Necessity 1 Allergies Dexchlorpheniramine levocetirizine Antihistamines Diphen Elixir (NDC^ 69067009204 only) RyClora CARBINOXAMINE TABLET 6 MG Anti-convulsants topiramate ext-rel capsule carbamazepine, carbamazepine ext-rel, (generics for QUDEXY XR only) clobazam, divalproex sodium, divalproex sodium ext-rel, gabapentin, lamotrigine, lamotrigine ext-rel, levetiracetam, levetiracetam ext-rel, oxcarbazepine, phenobarbital, phenytoin, phenytoin sodium extended, primidone, rufinamide, tiagabine, topiramate, valproic acid, zonisamide, FYCOMPA, OXTELLAR XR, TROKENDI XR, VIMPAT, XCOPRI ZONEGRAN carbamazepine, carbamazepine ext-rel, divalproex sodium, divalproex sodium ext-rel, gabapentin, lamotrigine, lamotrigine ext-rel, levetiracetam, levetiracetam ext-rel, oxcarbazepine, phenobarbital, phenytoin, phenytoin sodium extended, primidone, tiagabine, topiramate, valproic acid, zonisamide, FYCOMPA, OXTELLAR XR, TROKENDI -
Proxymetacaine Hydrochloride Ropivacaine Hydrochloride
1870 Local Anaesthetics Preparations pore: Alcaine; Switz.: Alcaine; Turk.: Alcaine; Opticaine; USA: Ak-Taine; Alcaine; Ocu-Caine; Ophthetic; Parcaine; Venez.: Alcaine; Oftaine†; Poen- (details are given in Part 3) caina. Proprietary Preparations CH3 Multi-ingredient: Spain: Detraine. O Multi-ingredient: Canad.: Fluoracaine†; USA: Fluoracaine; Fluorocaine. N CH3 O Quinisocaine Hydrochloride (BANM, rINNM) H3C Propipocaine (rINN) O Chinisocainum Hydrochloride; Dimethisoquin Hydrochloride Propipocaína; Propipocaïne; Propipocainum; Propoxypipero- (USAN); Dimethisoquinium Chloride; Hidrocloruro de quinisocaí- NH2 caine. 3-Piperidino-4′-propoxypropiophenone. na; Quinisocaïne, Chlorhydrate de; Quinisocaini Hydrochlori- (proxymetacaine) dum. 2-(3-Butyl-1-isoquinolyloxy)-NN-dimethylethylamine hy- Пропипокаин drochloride. C17H25NO2 = 275.4. Хинизокаина Гидрохлорид CAS — 3670-68-6. NOTE. PROX is a code approved by the BP 2008 for use on single unit doses of eye drops containing proxymetacaine hydrochlo- C17H24N2O,HCl = 308.8. ride where the individual container may be too small to bear all CAS — 86-80-6 (quinisocaine); 2773-92-4 (quinisocaine the appropriate labelling information. PROXFLN is a similar hydrochloride). O code approved for eye drops containing proxymetacaine hydro- ATC — D04AB05. chloride and fluorescein sodium. ATC Vet — QD04AB05. N Pharmacopoeias. In Br. and US. BP 2008 (Proxymetacaine Hydrochloride). A white or almost H3C CH3 white, odourless or almost odourless, crystalline powder. Soluble O in water and in chloroform; very soluble in dehydrated alcohol; N practically insoluble in ether. A 1% solution in water has a pH of O CH Profile 5.7 to 6.4. Protect from light. 3 Propipocaine is a local anaesthetic (p.1850) that has been used USP 31 (Proparacaine Hydrochloride). A white to off-white, or for surface anaesthesia. -

Properties and Units in Clinical Pharmacology and Toxicology
Pure Appl. Chem., Vol. 72, No. 3, pp. 479–552, 2000. © 2000 IUPAC INTERNATIONAL FEDERATION OF CLINICAL CHEMISTRY AND LABORATORY MEDICINE SCIENTIFIC DIVISION COMMITTEE ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)# and INTERNATIONAL UNION OF PURE AND APPLIED CHEMISTRY CHEMISTRY AND HUMAN HEALTH DIVISION CLINICAL CHEMISTRY SECTION COMMISSION ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)§ PROPERTIES AND UNITS IN THE CLINICAL LABORATORY SCIENCES PART XII. PROPERTIES AND UNITS IN CLINICAL PHARMACOLOGY AND TOXICOLOGY (Technical Report) (IFCC–IUPAC 1999) Prepared for publication by HENRIK OLESEN1, DAVID COWAN2, RAFAEL DE LA TORRE3 , IVAN BRUUNSHUUS1, MORTEN ROHDE1, and DESMOND KENNY4 1Office of Laboratory Informatics, Copenhagen University Hospital (Rigshospitalet), Copenhagen, Denmark; 2Drug Control Centre, London University, King’s College, London, UK; 3IMIM, Dr. Aiguader 80, Barcelona, Spain; 4Dept. of Clinical Biochemistry, Our Lady’s Hospital for Sick Children, Crumlin, Dublin 12, Ireland #§The combined Memberships of the Committee and the Commission (C-NPU) during the preparation of this report (1994–1996) were as follows: Chairman: H. Olesen (Denmark, 1989–1995); D. Kenny (Ireland, 1996); Members: X. Fuentes-Arderiu (Spain, 1991–1997); J. G. Hill (Canada, 1987–1997); D. Kenny (Ireland, 1994–1997); H. Olesen (Denmark, 1985–1995); P. L. Storring (UK, 1989–1995); P. Soares de Araujo (Brazil, 1994–1997); R. Dybkær (Denmark, 1996–1997); C. McDonald (USA, 1996–1997). Please forward comments to: H. Olesen, Office of Laboratory Informatics 76-6-1, Copenhagen University Hospital (Rigshospitalet), 9 Blegdamsvej, DK-2100 Copenhagen, Denmark. E-mail: [email protected] Republication or reproduction of this report or its storage and/or dissemination by electronic means is permitted without the need for formal IUPAC permission on condition that an acknowledgment, with full reference to the source, along with use of the copyright symbol ©, the name IUPAC, and the year of publication, are prominently visible. -
Ep 1931310 B1
(19) & (11) EP 1 931 310 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61K 9/12 (2006.01) A61K 9/06 (2006.01) 06.06.2012 Bulletin 2012/23 A61K 9/70 (2006.01) A61K 47/32 (2006.01) A61K 47/24 (2006.01) A61K 47/10 (2006.01) (21) Application number: 06779420.6 (86) International application number: (22) Date of filing: 14.09.2006 PCT/GB2006/003408 (87) International publication number: WO 2007/031753 (22.03.2007 Gazette 2007/12) (54) Monophasic film-forming composition for topical administration Monophasische filmbildende Zusammensetzung zum topischen Auftrag Composition monophase formant un film pour l’administration à voie topique (84) Designated Contracting States: • JONES, Stuart, Allen AT BE BG CH CY CZ DE DK EE ES FI FR GB GR London SE3 0XA (GB) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI SK TR (74) Representative: Lord, Hilton David Marks & Clerk LLP (30) Priority: 14.09.2005 GB 0518769 90 Long Acre London (43) Date of publication of application: WC2E 9RA (GB) 18.06.2008 Bulletin 2008/25 (56) References cited: (73) Proprietor: Medpharm Limited WO-A2-01/43722 US-A- 4 752 466 Charlbury, US-A- 4 863 721 US-A1- 2004 184 994 Oxfordshire OX7 3RR (GB) US-A1- 2004 213 744 (72) Inventors: • BROWN, Marc, Barry Hertfordshire WD19 4QQ (GB) Note: Within nine months of the publication of the mention of the grant of the European patent in the European Patent Bulletin, any person may give notice to the European Patent Office of opposition to that patent, in accordance with the Implementing Regulations. -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

Meta-Xylene: Identification of a New Antigenic Entity in Hypersensitivity
Clinical Communications Meta-xylene: identification of a new Our patient is a 53-year-old male who presented in 2003 with antigenic entity in hypersensitivity contact dermatitis after the use of lidocaine and disinfection with reactions to local anesthetics chlorhexidine. In 2006, an extensive skin testing by patch, prick, Kuntheavy Ing Lorenzini, PhDa, intradermal sampling, and graded challenge was performed as b c followed. The patch tests were performed with the thin layer Fabienne Gay-Crosier Chabry, MD , Claude Piguet, PhD , rapid use epicutaneous test, using the caine mix (benzocaine, a and Jules Desmeules, MD tetracaine, and cinchocaine), the paraben mix (methyl, ethyl, propyl, butyl, and benzylparaben), and the Balsam of Peru. The Clinical Implications caine and paraben mix were positive, and the patch test was possibly positive for Balsam of Peru. The prick test performed The authors report a patient who presented delayed with preservative-free lidocaine 20 mg/mL (Lidocaïne HCl hypersensitivity reactions to several local anesthetics, all “Bichsel” 2%, Grosse Apotheke Dr. G. Bichsel, Switzerland) was containing a meta-xylene entity, but not to articaine, negative. The intradermal test, performed with lidocaine 20 mg/ which is a thiophene derivative. Meta-xylene could be the mL containing methylparaben (Xylocain 2%, AstraZeneca, immunogenic epitope. Switzerland) with 1/10 and 1/100 dilutions, was negative. The subcutaneous challenge test was performed with 10 mg of preservative-free lidocaine 20 mg/mL (Lidocaïne HCl “Bichsel” TO THE EDITOR: 2%, Grosse Apotheke Dr. G. Bichsel) and lidocaine 20 mg/mL containing methylparaben (Lidocaïne Streuli 2%, Streuli, Hypersensitivity reactions to local anesthetics (LAs) are rare and Switzerland), both of which were positive and had the appear- represent less than 1% of all adverse reactions to LAs. -

Local Anesthetics
Local Anesthetics Introduction and History Cocaine is a naturally occurring compound indigenous to the Andes Mountains, West Indies, and Java. It was the first anesthetic to be discovered and is the only naturally occurring local anesthetic; all others are synthetically derived. Cocaine was introduced into Europe in the 1800s following its isolation from coca beans. Sigmund Freud, the noted Austrian psychoanalyst, used cocaine on his patients and became addicted through self-experimentation. In the latter half of the 1800s, interest in the drug became widespread, and many of cocaine's pharmacologic actions and adverse effects were elucidated during this time. In the 1880s, Koller introduced cocaine to the field of ophthalmology, and Hall introduced it to dentistry Overwiev Local anesthetics (LAs) are drugs that block the sensation of pain in the region where they are administered. LAs act by reversibly blocking the sodium channels of nerve fibers, thereby inhibiting the conduction of nerve impulses. Nerve fibers which carry pain sensation have the smallest diameter and are the first to be blocked by LAs. Loss of motor function and sensation of touch and pressure follow, depending on the duration of action and dose of the LA used. LAs can be infiltrated into skin/subcutaneous tissues to achieve local anesthesia or into the epidural/subarachnoid space to achieve regional anesthesia (e.g., spinal anesthesia, epidural anesthesia, etc.). Some LAs (lidocaine, prilocaine, tetracaine) are effective on topical application and are used before minor invasive procedures (venipuncture, bladder catheterization, endoscopy/laryngoscopy). LAs are divided into two groups based on their chemical structure. The amide group (lidocaine, prilocaine, mepivacaine, etc.) is safer and, hence, more commonly used in clinical practice.