Meta-Xylene: Identification of a New Antigenic Entity in Hypersensitivity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Mepivacaine Hydrochloride Injection
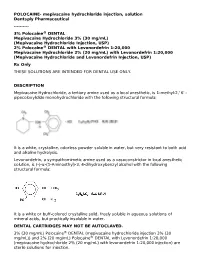
POLOCAINE- mepivacaine hydrochloride injection, solution Dentsply Pharmaceutical ---------- 3% Polocaine® DENTAL Mepivacaine Hydrochloride 3% (30 mg/mL) (Mepivacaine Hydrochloride Injection, USP) 2% Polocaine® DENTAL with Levonordefrin 1:20,000 Mepivacaine Hydrochloride 2% (20 mg/mL) with Levonordefrin 1:20,000 (Mepivacaine Hydrochloride and Levonordefrin Injection, USP) Rx Only THESE SOLUTIONS ARE INTENDED FOR DENTAL USE ONLY. DESCRIPTION Mepivacaine Hydrochloride, a tertiary amine used as a local anesthetic, is 1-methyl-2,' 6' - pipecoloxylidide monohydrochloride with the following structural formula: It is a white, crystalline, odorless powder soluble in water, but very resistant to both acid and alkaline hydrolysis. Levonordefrin, a sympathomimetic amine used as a vasoconstrictor in local anesthetic solution, is (-)-α-(1-Aminoethyl)-3, 4-dihydroxybenzyl alcohol with the following structural formula: It is a white or buff-colored crystalline solid, freely soluble in aqueous solutions of mineral acids, but practically insoluble in water. DENTAL CARTRIDGES MAY NOT BE AUTOCLAVED. 3% (30 mg/mL) Polocaine® DENTAL (mepivacaine hydrochloride injection 3% (30 mg/mL)) and 2% (20 mg/mL) Polocaine® DENTAL with Levonordefrin 1:20,000 (mepivacaine hydrochloride 2% (20 mg/mL) with levonordefrin 1:20,000 injection) are sterile solutions for injection. sterile solutions for injection. COMPOSITION: CARTRIDGE Each mL contains: 2% 3% Mepivacaine Hydrochloride 20 mg 30 mg Levonordefrin 0.05 mg - Sodium Chloride 4 mg 6 mg Potassium metabisulfite 1.2 mg - Edetate disodium 0.25 mg - Sodium Hydroxide q.s. ad pH; Hydrochloric 0.5 mg - Acid Water For Injection, qs. ad. 1 mL 1 mL The pH of the 2% cartridge solution is adjusted between 3.3 and 5.5 with NaOH. -

4% Citanest® Plain Dental (Prilocaine Hydrochloride Injection, USP) for Local Anesthesia in Dentistry
4% Citanest® Plain Dental (Prilocaine Hydrochloride Injection, USP) For Local Anesthesia in Dentistry Rx only DESCRIPTION 4% Citanest Plain Dental (prilocaine HCI Injection, USP), is a sterile, non-pyrogenic isotonic solution that contains a local anesthetic agent and is administered parenterally by injection. See INDICATIONS AND USAGE for specific uses. The quantitative composition is shown in Table 1. 4% Citanest Plain Dental contains prilocaine HCl, which is chemically designated as propanamide, N-(2- methyl-phenyl) -2- (propylamino)-, monohydrochloride and has the following structural formula: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration. The specific quantitative composition is shown in Table 1. TABLE 1. COMPOSITION Product Identification Formula (mg/mL) Prilocaine HCl pH 4% Citanest® Plain Dental 40.0 6.0 to 7.0 Note: Sodium hydroxide or hydrochloric acid may be used to adjust the pH of 4% Citanest Plain Dental Injection. CLINICAL PHARMACOLOGY Mechanism of Action: Prilocaine stabilizes the neuronal membrane by inhibiting the ionic fluxes required for the initiation and conduction of impulses, thereby effecting local anesthetic action. Onset and Duration of Action: When used for infiltration injection in dental patients, the time of onset of anesthesia averages less than 2 minutes with an average duration of soft tissue anesthesia of approximately 2 hours. Based on electrical stimulation studies, 4% Citanest Plain Dental Injection provides a duration of pulpal anesthesia of approximately 10 minutes in maxillary infiltration injections. In clinical studies, this has been found to provide complete anesthesia for procedures lasting an average of 20 minutes. When used for inferior alveolar nerve block, the time of onset of 4% Citanest Plain Dental Injection averages less than three minutes with an average duration of soft tissue anesthesia of approximately 2 ½hours. -

Local Anesthetic Half Life (In Hours) Lidocaine 1.6 Mepivacaine 1.9 Bupivacaine 353.5 Prilocaine 1.6 Articaine 0.5
Local Anesthetics • The first local anesthetics History were cocaine and procaine (Novacain) developed in ltlate 1800’s • They were called “esters” because of their chemical composition • Esters had a slow onset and short half life so they did not last long History • Derivatives of esters called “amides” were developed in the 1930’s • Amides had a faster onset and a longer half life so they lasted longer • AidAmides quiklickly repldlaced esters • In dentistry today, esters are only found in topical anesthetics Generic Local Anesthetics • There are five amide anesthetics used in dentistry today. Their generic names are; – lidocaine – mepivocaine – bupivacaine – prilocaine – artica ine • Each is known by at least one brand name Brand Names • lidocaine : Xylocaine, Lignospan, Alphacaine, Octocaine • mepivocaine: Carbocaine, Arestocaine, Isocaine, Polocaine, Scandonest • prilocaine : Citanest, Citanest Forte • bibupivaca ine: MiMarcaine • articaine: Septocaine, Zorcaine About Local Anesthetic (LA) • Local anesthetic (LA) works by binding with sodium channels in neurons preventing depolarization • LA is inactivated at the injection site when it is absorbed into the blood stream and redistributed throughout the body • If enough LA is absorbed, sodium channels in other parts of the body will be blocked, causing systemic side effects About LA • A clinical effect of LAs is dilation blood vessels, speeding up absorption and distribution • To counteract this dilation so anesthesia is prolonged, , a vasoconstrictor is often added to LAs • However, vasoconstrictors have side effects also Metabolism and Excretion • Most amide LAs are metabolized (inactivated) by the liver and excreted by the kidneys. • Prilocaine is partially metabolized by the lungs • Articaine is partially metabolized by enzymes in the bloo d as well as the liver. -

Hyperinflation Management Medications Requiring Prior Authorization for Medical Necessity
July 2021 Effective 07/01/2021 Hyperinflation Management Medications Requiring Prior Authorization for Medical Necessity Below is a list of medicines by drug class that will not be covered without a prior authorization for medical necessity. If you continue using one of these drugs without prior approval for medical necessity, you may be required to pay the full cost. If you are currently using one of the drugs requiring prior authorization for medical necessity, ask your d octor to choose one of the generic or brand formulary options listed below. Category * Drugs Requiring Prior Formulary Options Drug Class Authorization for Medical Necessity 1 Allergies Dexchlorpheniramine levocetirizine Antihistamines Diphen Elixir (NDC^ 69067009204 only) RyClora CARBINOXAMINE TABLET 6 MG Anti-convulsants topiramate ext-rel capsule carbamazepine, carbamazepine ext-rel, (generics for QUDEXY XR only) clobazam, divalproex sodium, divalproex sodium ext-rel, gabapentin, lamotrigine, lamotrigine ext-rel, levetiracetam, levetiracetam ext-rel, oxcarbazepine, phenobarbital, phenytoin, phenytoin sodium extended, primidone, rufinamide, tiagabine, topiramate, valproic acid, zonisamide, FYCOMPA, OXTELLAR XR, TROKENDI XR, VIMPAT, XCOPRI ZONEGRAN carbamazepine, carbamazepine ext-rel, divalproex sodium, divalproex sodium ext-rel, gabapentin, lamotrigine, lamotrigine ext-rel, levetiracetam, levetiracetam ext-rel, oxcarbazepine, phenobarbital, phenytoin, phenytoin sodium extended, primidone, tiagabine, topiramate, valproic acid, zonisamide, FYCOMPA, OXTELLAR XR, TROKENDI -
Ep 1931310 B1
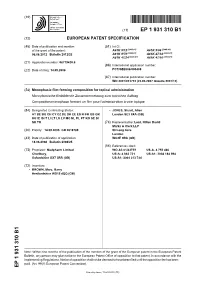
(19) & (11) EP 1 931 310 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61K 9/12 (2006.01) A61K 9/06 (2006.01) 06.06.2012 Bulletin 2012/23 A61K 9/70 (2006.01) A61K 47/32 (2006.01) A61K 47/24 (2006.01) A61K 47/10 (2006.01) (21) Application number: 06779420.6 (86) International application number: (22) Date of filing: 14.09.2006 PCT/GB2006/003408 (87) International publication number: WO 2007/031753 (22.03.2007 Gazette 2007/12) (54) Monophasic film-forming composition for topical administration Monophasische filmbildende Zusammensetzung zum topischen Auftrag Composition monophase formant un film pour l’administration à voie topique (84) Designated Contracting States: • JONES, Stuart, Allen AT BE BG CH CY CZ DE DK EE ES FI FR GB GR London SE3 0XA (GB) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI SK TR (74) Representative: Lord, Hilton David Marks & Clerk LLP (30) Priority: 14.09.2005 GB 0518769 90 Long Acre London (43) Date of publication of application: WC2E 9RA (GB) 18.06.2008 Bulletin 2008/25 (56) References cited: (73) Proprietor: Medpharm Limited WO-A2-01/43722 US-A- 4 752 466 Charlbury, US-A- 4 863 721 US-A1- 2004 184 994 Oxfordshire OX7 3RR (GB) US-A1- 2004 213 744 (72) Inventors: • BROWN, Marc, Barry Hertfordshire WD19 4QQ (GB) Note: Within nine months of the publication of the mention of the grant of the European patent in the European Patent Bulletin, any person may give notice to the European Patent Office of opposition to that patent, in accordance with the Implementing Regulations. -

Pdf; Chi 2015 DPP Air in Cars.Pdf; Dodson 2014 DPP Dust CA.Pdf; Kasper-Sonnenberg 2014 Phth Metabolites.Pdf; EU Cosmetics Regs 2009.Pdf
Bouge, Cathy (ECY) From: Nancy Uding <[email protected]> Sent: Friday, January 13, 2017 10:24 AM To: Steward, Kara (ECY) Cc: Erika Schreder Subject: Comments re. 2016 CSPA Rule Update - DPP Attachments: DPP 131-18-0 exposure.pdf; Chi 2015 DPP air in cars.pdf; Dodson 2014 DPP dust CA.pdf; Kasper-Sonnenberg 2014 phth metabolites.pdf; EU Cosmetics Regs 2009.pdf Please accept these comments from Toxic-Free Future concerning the exposure potential of DPP for consideration during the 2016 CSPA Rule update. Regards, Nancy Uding -- Nancy Uding Grants & Research Specialist Toxic-Free Future 206-632-1545 ext.123 http://toxicfreefuture.org 1 JES-00888; No of Pages 9 JOURNAL OF ENVIRONMENTAL SCIENCES XX (2016) XXX– XXX Available online at www.sciencedirect.com ScienceDirect www.elsevier.com/locate/jes Determination of 15 phthalate esters in air by gas-phase and particle-phase simultaneous sampling Chenchen Chi1, Meng Xia1, Chen Zhou1, Xueqing Wang1,2, Mili Weng1,3, Xueyou Shen1,4,⁎ 1. College of Environmental & Resource Sciences, Zhejiang University, Hangzhou 310058, China 2. Zhejiang National Radiation Environmental Technology Co., Ltd., Hangzhou 310011, China 3. School of Environmental and Resource Sciences, Zhejiang Agriculture and Forestry University, Hangzhou 310058, China 4. Zhejiang Provincial Key Laboratory of Organic Pollution Process and Control, Hangzhou 310058, China ARTICLE INFO ABSTRACT Article history: Based on previous research, the sampling and analysis methods for phthalate esters (PAEs) Received 24 December 2015 were improved by increasing the sampling flow of indoor air from 1 to 4 L/min, shortening the Revised 14 January 2016 sampling duration from 8 to 2 hr. -

Local Anesthetics
Local Anesthetics Introduction and History Cocaine is a naturally occurring compound indigenous to the Andes Mountains, West Indies, and Java. It was the first anesthetic to be discovered and is the only naturally occurring local anesthetic; all others are synthetically derived. Cocaine was introduced into Europe in the 1800s following its isolation from coca beans. Sigmund Freud, the noted Austrian psychoanalyst, used cocaine on his patients and became addicted through self-experimentation. In the latter half of the 1800s, interest in the drug became widespread, and many of cocaine's pharmacologic actions and adverse effects were elucidated during this time. In the 1880s, Koller introduced cocaine to the field of ophthalmology, and Hall introduced it to dentistry Overwiev Local anesthetics (LAs) are drugs that block the sensation of pain in the region where they are administered. LAs act by reversibly blocking the sodium channels of nerve fibers, thereby inhibiting the conduction of nerve impulses. Nerve fibers which carry pain sensation have the smallest diameter and are the first to be blocked by LAs. Loss of motor function and sensation of touch and pressure follow, depending on the duration of action and dose of the LA used. LAs can be infiltrated into skin/subcutaneous tissues to achieve local anesthesia or into the epidural/subarachnoid space to achieve regional anesthesia (e.g., spinal anesthesia, epidural anesthesia, etc.). Some LAs (lidocaine, prilocaine, tetracaine) are effective on topical application and are used before minor invasive procedures (venipuncture, bladder catheterization, endoscopy/laryngoscopy). LAs are divided into two groups based on their chemical structure. The amide group (lidocaine, prilocaine, mepivacaine, etc.) is safer and, hence, more commonly used in clinical practice. -

Prescribing Information Carbocaine 1%
Prescribing Information Carbocaine 1% 10 mg/mL, Mepivacaine Hydrochloride Injection, USP Carbocaine 2% 20 mg/mL, Mepivacaine Hydrochloride Injection, USP Local Anesthetic Pfizer Canada Inc. DATE OF REVISION: 17300 Trans-Canada Highway August 2, 2017 Kirkland, Québec NTF: February 14, 2018 H9J 2M5 Control Number: (204807) 1 Prescribing Information Carbocaine 1% 10 mg/mL, Mepivacaine Hydrochloride Injection, USP Carbocaine 2% 20 mg/mL, Mepivacaine Hydrochloride Injection, USP Local Anesthetic Pharmacology: Mepivacaine stabilizes the neuronal membrane and prevents the initiation and transmission of nerve impulses, thereby effecting local anesthesia. Its pharmacological properties are somewhat similar to those of lidocaine, which it resembles chemically. Its action is more rapid in onset and somewhat more prolonged than that of lidocaine. It has been employed for all types of infiltration and regional nerve block anesthesia. Onset of anesthesia is rapid, the time of onset for sensory block ranging from about 3 to 20 minutes depending upon such factors as the anesthetic technique, the type of block, the concentration of the solution and the individual patient. The degree of motor blockade produced is dependent on the concentration of the solution. The 1% concentration will block sensory and sympathetic conduction without loss of motor function and will be effective in small superficial nerve blocks. The 2% concentration of mepivacaine will produce complete sensory and motor block of any nerve group. The duration of anesthesia also varies depending upon the technique and type of block, the concentration and the individual. Mepivacaine will normally provide anesthesia which is adequate for 2 to 2½ hours of surgery. It has been reported that vasoconstrictors do not significantly prolong anesthesia with mepivacaine, but epinephrine (1:200 000) may be added to the mepivacaine solution to promote local hemostasis and to delay systemic absorption of the anesthetic. -

Product Monograph
PRESCRIBING INFORMATION INCLUDING PATIENT MEDICATION INFORMATION PrSANDOZ PROCTOMYXIN HC (Hydrocortisone, Framycetin Sulfate, Cinchocaine Hydrochloride and Esculin) Ointment PrSANDOZ PROCTOMYXIN HC SUPPOSITORIES (Hydrocortisone, Framycetin Sulfate, Cinchocaine Hydrochloride and Esculin) Suppositories Antibacterial – Corticosteroid – Anorectal Therapy Sandoz Canada Inc. Date of Revision 110 Rue de Lauzon November 16, 2018 Boucherville, QC J4B 1E6 Submission Control Number: 220681 PRESCRIBING INFORMATION Sandoz Proctomyxin HC Sandoz Proctomyxin HC Suppositories (Hydrocortisone, Framycetin Sulfate, Cinchocaine Hydrochloride and Esculin) Suppositories and Ointment THERAPEUTIC CLASSIFICATION Antibacterial – Corticosteroid – Anorectal Therapy ACTIONS AND CLINICAL PHARMACOLOGY Framycetin sulfate, also known as neomycin B, is an aminoglycoside antibiotic which forms the major component of neomycin sulfate and has similar actions and uses. Aminoglycosides are taken up into sensitive bacterial cells by an active transport process which is inhibited in anærobic, acidic, or hyperosmolar environments. Within the cell, they bind to the 30S and to some extent to the 50S subunits of the bacterial ribosome, inhibiting protein synthesis and generating errors in the transcription of the genetic code. The manner in which cell death is brought about is imperfectly understood, and other mechanisms may contribute, including effects on membrane permeability. In general, neomycin is active against many ærobic gram-negative bacteria and some aerobic gram-positive bacteria. Bacterial strains susceptible to neomycin include: Escherichia coli, Hæmophilus influenzæ, Moraxella lacunata, indole-positive and indole-negative Proteus, Staphylococcus aureus, S. epidermidis and Serratia. Neomycin is only minimally active against streptococci. Pseudomonas æruginosa is generally resistant to the drug. The drug is inactive against fungi, viruses, and most anærobic bacteria. Natural and acquired resistance to neomycin have been demonstrated in both gram-negative and gram-positive bacteria. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

Quick Practice Guides Index with Few Exceptions, the Quick Practice Guides in PCF Are Restricted to a Maximum of 2 Pages in Order to Facilitate Everyday Use
PCF4_Cover_MAY.qxp 8/18/11 2:57 PM Page 2 Quick Practice Guides Index With few exceptions, the Quick Practice Guides in PCF are restricted to a maximum of 2 pages in order to facilitate everyday use. Before using them, it is important to study the associated text in order to fully understand their rationale. Page Chapter 1: Gastro-intestinal system Management of death rattle (noisy respiratory secretions) 8 Opioid-induced constipation 38 Bowel management in paraplegia and tetraplegia 40 Chapter 4: Central nervous system Depression 187 Psychostimulants in depressed patients with a short prognosis 209 Management of nausea and vomiting 225 Chapter 5: Analgesics Management of procedure-related pain 379 Use of transdermal buprenorphine 388 Use of transdermal fentanyl patches 398 Use of methadone for cancer pain 422 Chapter 6: Infections Cellulitis in lymphoedema 459 Chapter 16 Management of death rattle (noisy respiratory secretions) repeat 637 Chapter 20 Setting up a McKinley T34 syringe pump for CSCI 673 Setting up a Graseby MS16A or MS26 syringe driver for CSCI 676 Chapter 22 Administration of drugs by enteral feeding tube 700 PCF4 PALLIATIVE CARE FORMULARY This first print-run of PCF4 has been made possible, in part, by Help the Hospices, the leading charity supporting hospice care throughout the United Kingdom. www.helpthehospices.org.uk Published by palliativedrugs.com Ltd. Palliativedrugs.com Ltd Hayward House Study Centre Nottingham University Hospitals NHS Trust, City Campus Nottingham NG5 1PB United Kingdom www.palliativedrugs.com # palliativedrugs.com Ltd 2011 The moral rights of the editors have been asserted. PCF3 2007, reprinted 2008, 2009 PCF2 2002, reprinted 2003 PCF1 1998 All rights reserved. -

Contact Dermatitis to Medications and Skin Products
Clinical Reviews in Allergy & Immunology (2019) 56:41–59 https://doi.org/10.1007/s12016-018-8705-0 Contact Dermatitis to Medications and Skin Products Henry L. Nguyen1 & James A. Yiannias2 Published online: 25 August 2018 # Springer Science+Business Media, LLC, part of Springer Nature 2018 Abstract Consumer products and topical medications today contain many allergens that can cause a reaction on the skin known as allergic contact dermatitis. This review looks at various allergens in these products and reports current allergic contact dermatitis incidence and trends in North America, Europe, and Asia. First, medication contact allergy to corticosteroids will be discussed along with its five structural classes (A, B, C, D1, D2) and their steroid test compounds (tixocortol-21-pivalate, triamcinolone acetonide, budesonide, clobetasol-17-propionate, hydrocortisone-17-butyrate). Cross-reactivities between the steroid classes will also be examined. Next, estrogen and testosterone transdermal therapeutic systems, local anesthetic (benzocaine, lidocaine, pramoxine, dyclonine) antihistamines (piperazine, ethanolamine, propylamine, phenothiazine, piperidine, and pyrrolidine), top- ical antibiotics (neomycin, spectinomycin, bacitracin, mupirocin), and sunscreen are evaluated for their potential to cause contact dermatitis and cross-reactivities. Finally, we examine the ingredients in the excipients of these products, such as the formaldehyde releasers (quaternium-15, 2-bromo-2-nitropropane-1,3 diol, diazolidinyl urea, imidazolidinyl urea, DMDM hydantoin), the non- formaldehyde releasers (isothiazolinones, parabens, methyldibromo glutaronitrile, iodopropynyl butylcarbamate, and thimero- sal), fragrance mixes, and Myroxylon pereirae (Balsam of Peru) for contact allergy incidence and prevalence. Furthermore, strategies, recommendations, and two online tools (SkinSAFE and the Contact Allergen Management Program) on how to avoid these allergens in commercial skin care products will be discussed at the end.