Local Anesthetics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chapter 11 Local Anesthetics
Chapter LOCAL ANESTHETICS 11 Kenneth Drasner HISTORY MECHANISMS OF ACTION AND FACTORS ocal anesthesia can be defined as loss of sensation in AFFECTING BLOCK L a discrete region of the body caused by disruption of Nerve Conduction impulse generation or propagation. Local anesthesia can Anesthetic Effect and the Active Form of the be produced by various chemical and physical means. Local Anesthetic However, in routine clinical practice, local anesthesia is Sodium Ion Channel State, Anesthetic produced by a narrow class of compounds, and recovery Binding, and Use-Dependent Block is normally spontaneous, predictable, and complete. Critical Role of pH Lipid Solubility Differential Local Anesthetic Blockade Spread of Local Anesthesia after Injection HISTORY PHARMACOKINETICS Cocaine’s systemic toxicity, its irritant properties when Local Anesthetic Vasoactivity placed topically or around nerves, and its substantial Metabolism potential for physical and psychological dependence gene- Vasoconstrictors rated interest in identification of an alternative local 1 ADVERSE EFFECTS anesthetic. Because cocaine was known to be a benzoic Systemic Toxicity acid ester (Fig. 11-1), developmental strategies focused Allergic Reactions on this class of chemical compounds. Although benzo- caine was identified before the turn of the century, its SPECIFIC LOCAL ANESTHETICS poor water solubility restricted its use to topical anesthe- Amino-Esters sia, for which it still finds some limited application in Amino-Amide Local Anesthetics modern clinical practice. The -
Europæisk Patentskrift
(19) DANMARK (1°) DK/EP 2968225 T3 (12) Oversættelse af europæisk patentskrift Patent- og Varemærkestyrelsen (51) lnt.CI.: A 61 K 31/137 (2006.01) A 61 K 9/00 (2006.01) A 61 K 31/245 (2006.01) A 61 K 31/445 (2006.01) A 61 K 31/519 (2006.01) A 61 K 31/52 (2006.01) A 61 P 43/00 (2006.01) (45) Oversættelsen bekendtgjort den: 2019-05-27 (80) Dato for Den Europæiske Patentmyndigheds bekendtgørelse om meddelelse af patentet: 2019-02-20 (86) Europæisk ansøgning nr.: 14719486.4 (86) Europæisk indleveringsdag: 2014-03-17 (87) Den europæiske ansøgnings publiceringsdag: 2016-01-20 (86) International ansøgning nr.: US2014030372 (87) Internationalt publikationsnr.: WO2014145580 (30) Prioritet: 2013-03-15 US 201361789054 P (84) Designerede stater: AL AT BE BG CH CY CZ DE DK EE ES Fl FR GB GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL PT RO RS SE SI SK SM TR (73) Patenthaver: The Children's Medical Center Corporation, 55 Shattuck Street, Boston, Massachusetts 02115, USA (72) Opfinder: BERDE, Charles, 14 Doran Road, Bookline, MA 02146, USA KOHANE, Daniel S., 119 Willard Street, Newton, MA 02461, USA (74) Fuldmægtig i Danmark: AWA Denmark A/S, Strandgade 56,1401 København K, Danmark (54) Benævnelse: NEOSAXITOXINKOMBINATIONSFORMULERINGER TIL FORLÆNGET LOKALANÆSTESI (56) Fremdragne publikationer: WO-A2-98/51290 ALBERTO J. RODRIGUEZ-NAVARRO ET AL: "Potentiation of Local Anesthetic Activity of Neosaxitoxin with Bupivacaine or Epinephrine: Development of a Long-Acting Pain Blocker", NEUROTOXICITY RESEARCH, vol. 16, no. 4, 28 July 2009 (2009-07-28), pages 408-415, XP055122925, ISSN: 1029-8428, DOI: 10.1007/s12640-009- 9092-3 cited in the application Anonymous: "NCT01786655 on 2013_02_11: ClinicalTrials.gov Archive",, 11 February 2013 (2013-02-11), XP055122935, Retrieved from the Internet: URL:http://clinicaltrials.gov/archive/NCTO 1786655/2013_02_11 [retrieved on 2014-06-12] CHARLES B. -

Bupivacaine Injection Bp
PRODUCT MONOGRAPH INCLUDING CONSUMER INFORMATION BUPIVACAINE INJECTION BP Bupivacaine hydrochloride 0.25% (2.5 mg/mL) and 0.5% (5 mg/mL) Local Anaesthetic SteriMax Inc. Date of Preparation: 2770 Portland Dr. July 10, 2015 Oakville, ON, L6H 6R4 Submission Control No: 180156 Bupivacaine Injection Page 1 of 28 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION .................................................................... 3 SUMMARY PRODUCT INFORMATION ................................................................................... 3 INDICATIONS AND CLINICAL USE ......................................................................................... 3 CONTRAINDICATIONS .............................................................................................................. 3 WARNINGS AND PRECAUTIONS ............................................................................................. 4 ADVERSE REACTIONS ............................................................................................................... 9 DRUG INTERACTIONS ............................................................................................................. 10 DOSAGE AND ADMINISTRATION ......................................................................................... 13 OVERDOSAGE ........................................................................................................................... 16 ACTION AND CLINICAL PHARMACOLOGY ....................................................................... 18 STORAGE -

A Randomised, Non-Inferiority Study of Chloroprocaine 2% and Ropivacaine
www.nature.com/scientificreports OPEN A randomised, non‑inferiority study of chloroprocaine 2% and ropivacaine 0.75% in ultrasound‑guided axillary block Irene Sulyok1, Claudio Camponovo2, Oliver Zotti1, Werner Haslik3, Markus Köstenberger4, Rudolf Likar4, Chiara Leuratti5, Elisabetta Donati6 & Oliver Kimberger1,7* Chloroprocaine is a short‑acting local anaesthetic with a rapid onset of action and an anaesthesia duration up to 60 min. In this pivotal study success rates, onset and remission of motor and sensory block and safety of chloroprocaine 2% was compared to ropivacaine 0.75% for short‑duration distal upper limb surgery with successful block rates as primary outcome. The study was designed as a prospective, randomised, multi‑centre, active‑controlled, double‑blind, parallel‑group, non‑inferiority study, performed in 4 European hospitals with 211 patients scheduled for short duration distal upper limb surgery under axillary plexus block anaesthesia. Patients received either ultrasound guided axillary block with 20 ml chloroprocaine 2%, or with 20 ml ropivacaine 0.75%. Successful block was defned as block without any supplementation in the frst 45 min calculated from the time of readiness for surgery. 90.8% patients achieved a successful block with chloroprocaine 2% and 92.9% patients with Ropivacaine 0.75%, thus non‑inferiority was demonstrated (10% non inferiority margin; 95% CI − 0.097, 0.039; p = 0.02). Time to onset of block was not signifcantly diferent between the groups. Median time to motor and sensory block regression was signifcantly shorter as was time to home discharge (164 [155–170] min for chloroprocaine versus 380 [209–450] for the ropivacaine group, p < 0.001). -
Mepivacaine Hydrochloride Injection
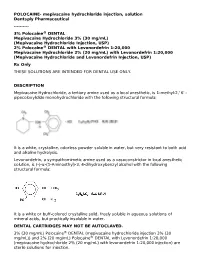
POLOCAINE- mepivacaine hydrochloride injection, solution Dentsply Pharmaceutical ---------- 3% Polocaine® DENTAL Mepivacaine Hydrochloride 3% (30 mg/mL) (Mepivacaine Hydrochloride Injection, USP) 2% Polocaine® DENTAL with Levonordefrin 1:20,000 Mepivacaine Hydrochloride 2% (20 mg/mL) with Levonordefrin 1:20,000 (Mepivacaine Hydrochloride and Levonordefrin Injection, USP) Rx Only THESE SOLUTIONS ARE INTENDED FOR DENTAL USE ONLY. DESCRIPTION Mepivacaine Hydrochloride, a tertiary amine used as a local anesthetic, is 1-methyl-2,' 6' - pipecoloxylidide monohydrochloride with the following structural formula: It is a white, crystalline, odorless powder soluble in water, but very resistant to both acid and alkaline hydrolysis. Levonordefrin, a sympathomimetic amine used as a vasoconstrictor in local anesthetic solution, is (-)-α-(1-Aminoethyl)-3, 4-dihydroxybenzyl alcohol with the following structural formula: It is a white or buff-colored crystalline solid, freely soluble in aqueous solutions of mineral acids, but practically insoluble in water. DENTAL CARTRIDGES MAY NOT BE AUTOCLAVED. 3% (30 mg/mL) Polocaine® DENTAL (mepivacaine hydrochloride injection 3% (30 mg/mL)) and 2% (20 mg/mL) Polocaine® DENTAL with Levonordefrin 1:20,000 (mepivacaine hydrochloride 2% (20 mg/mL) with levonordefrin 1:20,000 injection) are sterile solutions for injection. sterile solutions for injection. COMPOSITION: CARTRIDGE Each mL contains: 2% 3% Mepivacaine Hydrochloride 20 mg 30 mg Levonordefrin 0.05 mg - Sodium Chloride 4 mg 6 mg Potassium metabisulfite 1.2 mg - Edetate disodium 0.25 mg - Sodium Hydroxide q.s. ad pH; Hydrochloric 0.5 mg - Acid Water For Injection, qs. ad. 1 mL 1 mL The pH of the 2% cartridge solution is adjusted between 3.3 and 5.5 with NaOH. -

4% Citanest® Plain Dental (Prilocaine Hydrochloride Injection, USP) for Local Anesthesia in Dentistry
4% Citanest® Plain Dental (Prilocaine Hydrochloride Injection, USP) For Local Anesthesia in Dentistry Rx only DESCRIPTION 4% Citanest Plain Dental (prilocaine HCI Injection, USP), is a sterile, non-pyrogenic isotonic solution that contains a local anesthetic agent and is administered parenterally by injection. See INDICATIONS AND USAGE for specific uses. The quantitative composition is shown in Table 1. 4% Citanest Plain Dental contains prilocaine HCl, which is chemically designated as propanamide, N-(2- methyl-phenyl) -2- (propylamino)-, monohydrochloride and has the following structural formula: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration. The specific quantitative composition is shown in Table 1. TABLE 1. COMPOSITION Product Identification Formula (mg/mL) Prilocaine HCl pH 4% Citanest® Plain Dental 40.0 6.0 to 7.0 Note: Sodium hydroxide or hydrochloric acid may be used to adjust the pH of 4% Citanest Plain Dental Injection. CLINICAL PHARMACOLOGY Mechanism of Action: Prilocaine stabilizes the neuronal membrane by inhibiting the ionic fluxes required for the initiation and conduction of impulses, thereby effecting local anesthetic action. Onset and Duration of Action: When used for infiltration injection in dental patients, the time of onset of anesthesia averages less than 2 minutes with an average duration of soft tissue anesthesia of approximately 2 hours. Based on electrical stimulation studies, 4% Citanest Plain Dental Injection provides a duration of pulpal anesthesia of approximately 10 minutes in maxillary infiltration injections. In clinical studies, this has been found to provide complete anesthesia for procedures lasting an average of 20 minutes. When used for inferior alveolar nerve block, the time of onset of 4% Citanest Plain Dental Injection averages less than three minutes with an average duration of soft tissue anesthesia of approximately 2 ½hours. -

Local Anesthetic Half Life (In Hours) Lidocaine 1.6 Mepivacaine 1.9 Bupivacaine 353.5 Prilocaine 1.6 Articaine 0.5
Local Anesthetics • The first local anesthetics History were cocaine and procaine (Novacain) developed in ltlate 1800’s • They were called “esters” because of their chemical composition • Esters had a slow onset and short half life so they did not last long History • Derivatives of esters called “amides” were developed in the 1930’s • Amides had a faster onset and a longer half life so they lasted longer • AidAmides quiklickly repldlaced esters • In dentistry today, esters are only found in topical anesthetics Generic Local Anesthetics • There are five amide anesthetics used in dentistry today. Their generic names are; – lidocaine – mepivocaine – bupivacaine – prilocaine – artica ine • Each is known by at least one brand name Brand Names • lidocaine : Xylocaine, Lignospan, Alphacaine, Octocaine • mepivocaine: Carbocaine, Arestocaine, Isocaine, Polocaine, Scandonest • prilocaine : Citanest, Citanest Forte • bibupivaca ine: MiMarcaine • articaine: Septocaine, Zorcaine About Local Anesthetic (LA) • Local anesthetic (LA) works by binding with sodium channels in neurons preventing depolarization • LA is inactivated at the injection site when it is absorbed into the blood stream and redistributed throughout the body • If enough LA is absorbed, sodium channels in other parts of the body will be blocked, causing systemic side effects About LA • A clinical effect of LAs is dilation blood vessels, speeding up absorption and distribution • To counteract this dilation so anesthesia is prolonged, , a vasoconstrictor is often added to LAs • However, vasoconstrictors have side effects also Metabolism and Excretion • Most amide LAs are metabolized (inactivated) by the liver and excreted by the kidneys. • Prilocaine is partially metabolized by the lungs • Articaine is partially metabolized by enzymes in the bloo d as well as the liver. -

Subject Index
52_1107_1136_SI 16.11.2005 9:35 Uhr Seite 1107 Subject Index A – tape 264, 368, 940 α-adjustment 154 AAS, see atomic absorption spectrophotometry adrenocorticotrophic hormone (ACTH) 21 abietic acid 909, 943 adverse drug reaction 401 abrasion 174, 283 aeroallergen 391 absorption through appendage 169 – atopic eczema 391 α-acaridial 329 – avoidance 391 accident 889 aerospace 726 acebutolol hydrochloride 909 African aceclofenac 909 –ebony783 acetaldehyde 943 – mahagony 783 acetone 118, 666 – red padauk wood 783 acetylacetone 697 Agave acetylsalicylic acid 84, 909 – americana 354 Achillea millefolium (yarrow extract) 909 – tequilana 225 aciclovir 909 age 279 acid 110 agent orange 806 – black 48 (CI 65005) 909 AGEP 404 – dye 689 Agfa TSS 355 – halogenated 259 aggravation 204 –hydrochloric261 agricultural worker 272 –nitric261 agriculture 725 –red AICD, see activation-induced cell death – – 14 (azorubine) 909 airborne – – 118 (CI 26410) 909 – allergic contact dermatitis 218, 228, 315, 467, 477, 484, 598, ––359909 627, 654, 788 – violet 17 (CI 42650) 909 – contact urticaria 753, 758 – yellow – irritant contact dermatitis 625 – – 36 (CI 13065, metanil yellow) 909 aircraft manufacture 560 – – 61 (CI 18968) 909 airway symptom 520 acitretin 341 alachlor 953 acneiform alantolactone 55, 789, 909, 954 – folliculitis 229 alclometasone-17,21-dipropionate 909 –lesion265 alclometasone-17-propionate 58 acrodermatitis enteropathica 241 alcohol, see also ethyl 909 acrovesicular dermatitis 401 aldehyde 110, 607, 886 acrylamide 592, 944 algicide 562 acrylate -

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -

Medicines Used Across Wirral Health Economy
Medicines used across Wirral Health Economy Below is a list of medicines that are approved for use on Wirral. Some medicines may only be prescribed in hospital, others may be prescribed by your GP. The list is updated every time a new medicine is approved for use in Wirral. Some medicines have been recommended by the National Institute for Health and Care Excellence (NICE). The middle column of the table below indicates recommendations made by NICE — eg, TA234 means that the medicine was reviewed in NICE technology appraisal number 234. Some of the medicines we use are recommended by specialists working from the Walton Centre NHS Foundation Trust or from the Cheshire and Wirral Partnership NHS Foundation Trust. These medicines are included in our formulary — however; the prescriber retains responsibility for the appropriate use of these medicines. These formularies are obtainable here: http://www.panmerseyapc.nhs.uk/formulary/documents/04- 0800_antiepileptic_drugs.pdf http://www.panmerseyapc.nhs.uk/formulary/documents/04-09- 00_parkinsonism.pdf http://www.cwp.nhs.uk/pages/629-pharmacy-and-medicines-information Subject to NICE Drug Name recommendation Abatacept TA195, TA280 Acamprosate Acarbose Accu-Chek Inform II® AccuSol® 35 Potassium 4mmol/L Acetazolamide Acetylcysteine Acencoumarol Acetic acid 5% solution Acetone Acitretin Aciclovir Wirral Medicines Formulary Author: Medicines Management Team Approved by: Wirral Drug and Therapeutics Panel Last updated: June 2015 Version 10 Aclinidium Actilite® Activated Charcoal Activon® - see -

Properties and Units in Clinical Pharmacology and Toxicology
Pure Appl. Chem., Vol. 72, No. 3, pp. 479–552, 2000. © 2000 IUPAC INTERNATIONAL FEDERATION OF CLINICAL CHEMISTRY AND LABORATORY MEDICINE SCIENTIFIC DIVISION COMMITTEE ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)# and INTERNATIONAL UNION OF PURE AND APPLIED CHEMISTRY CHEMISTRY AND HUMAN HEALTH DIVISION CLINICAL CHEMISTRY SECTION COMMISSION ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)§ PROPERTIES AND UNITS IN THE CLINICAL LABORATORY SCIENCES PART XII. PROPERTIES AND UNITS IN CLINICAL PHARMACOLOGY AND TOXICOLOGY (Technical Report) (IFCC–IUPAC 1999) Prepared for publication by HENRIK OLESEN1, DAVID COWAN2, RAFAEL DE LA TORRE3 , IVAN BRUUNSHUUS1, MORTEN ROHDE1, and DESMOND KENNY4 1Office of Laboratory Informatics, Copenhagen University Hospital (Rigshospitalet), Copenhagen, Denmark; 2Drug Control Centre, London University, King’s College, London, UK; 3IMIM, Dr. Aiguader 80, Barcelona, Spain; 4Dept. of Clinical Biochemistry, Our Lady’s Hospital for Sick Children, Crumlin, Dublin 12, Ireland #§The combined Memberships of the Committee and the Commission (C-NPU) during the preparation of this report (1994–1996) were as follows: Chairman: H. Olesen (Denmark, 1989–1995); D. Kenny (Ireland, 1996); Members: X. Fuentes-Arderiu (Spain, 1991–1997); J. G. Hill (Canada, 1987–1997); D. Kenny (Ireland, 1994–1997); H. Olesen (Denmark, 1985–1995); P. L. Storring (UK, 1989–1995); P. Soares de Araujo (Brazil, 1994–1997); R. Dybkær (Denmark, 1996–1997); C. McDonald (USA, 1996–1997). Please forward comments to: H. Olesen, Office of Laboratory Informatics 76-6-1, Copenhagen University Hospital (Rigshospitalet), 9 Blegdamsvej, DK-2100 Copenhagen, Denmark. E-mail: [email protected] Republication or reproduction of this report or its storage and/or dissemination by electronic means is permitted without the need for formal IUPAC permission on condition that an acknowledgment, with full reference to the source, along with use of the copyright symbol ©, the name IUPAC, and the year of publication, are prominently visible. -

List of Union Reference Dates A
Active substance name (INN) EU DLP BfArM / BAH DLP yearly PSUR 6-month-PSUR yearly PSUR bis DLP (List of Union PSUR Submission Reference Dates and Frequency (List of Union Frequency of Reference Dates and submission of Periodic Frequency of submission of Safety Update Reports, Periodic Safety Update 30 Nov. 2012) Reports, 30 Nov.