Safety Alert: Risks Associated with Ophthalmic Anesthetics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MCQ Base Clinical Pharmacology
MCQ Base Clinical Pharmacology Mechanism of drug action is explored by: A) pharmacokinetics B) pharmacogenetics C) pharmacoeconomics D) pharmacodynamics E) pharmacognosy Therapeutic window is the dosages of a medication (therapeutic serum concentrations ) between: A) TD50 curve and ED50 B) ED50 and T1/2 C) the amount that gives an effect (effective dose) and the amount that gives more adverse effects than desired effects D) the amount that gives minimal adverse effects and the amount that gives more adverse effects E) the amount that gives minimal effect and the amount that gives full therapeutic effect Therapeutic index is the ratio of: A) LD50 over the ED50 B) ED50over the LD50 C) bioavailability over drug dose D) apparent volume of distribution over elimination rate constant E) total clearance over nonrenal (extrarenal) clearance Therapeutic drug monitoring means: A) trough concentration under steady-state condition B) measurement of medication concentrations in blood C) the process of chemical alteration of drugs in the body D) amount of untoward effects following treatment E) development of expected desired effects Therapeutic dose is not related to: A) patient’s age B) rout of administration C) desired therapeutic effect D) organs of elimination E) treatment costs Mean therapeutic doses mentioned in manuals is obtained by the following way: A) calculation of pharmacokinetic features B) clinical investigations C) experimental investigations D) experimental data adopted for human body E) calculation of pharmacodynamic features Find -

208135Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 208135Orig1s000 STATISTICAL REVIEW(S) U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research Office of Translational Sciences Office of Biostatistics S TATISTICAL R EVIEW AND E VALUATION CLINICAL STUDIES NDA/BLA #: 208135 Drug Name: Tetracaine Hydrochloride Ophthalmic Solution 0.5% (STERI-UNIT®) Indication(s): For procedures requiring a rapid and short acting ophthalmic anesthetic Applicant: Alcon research ltd Date(s): Stamp date: April 30, 2015 PDUFA date: February 29, 2016 Review Priority: Standard Biometrics Division: DBIV Statistical Reviewer: Abel Tilahun Eshete Concurring Reviewers: Yan Wang Medical Division: Ophthalmology Clinical Team: Medical Reviewer: Jennifer Harris Project Manager: Michael Puglisi Keywords: Topical anesthesia, Pain scores, Tetracaine . Reference ID: 3875889 Table of Contents 1 EXECUTIVE SUMMARY............................................................................................................................... 4 2 INTRODUCTION............................................................................................................................................. 6 2.1 OVERVIEW ................................................................................................................................................... 6 2.2 SUBMISSION HISTORY .................................................................................................................................. 6 2.3 -
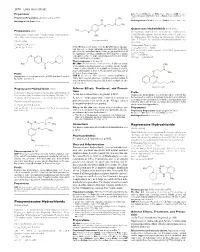
Proxymetacaine Hydrochloride Ropivacaine Hydrochloride
1870 Local Anaesthetics Preparations pore: Alcaine; Switz.: Alcaine; Turk.: Alcaine; Opticaine; USA: Ak-Taine; Alcaine; Ocu-Caine; Ophthetic; Parcaine; Venez.: Alcaine; Oftaine†; Poen- (details are given in Part 3) caina. Proprietary Preparations CH3 Multi-ingredient: Spain: Detraine. O Multi-ingredient: Canad.: Fluoracaine†; USA: Fluoracaine; Fluorocaine. N CH3 O Quinisocaine Hydrochloride (BANM, rINNM) H3C Propipocaine (rINN) O Chinisocainum Hydrochloride; Dimethisoquin Hydrochloride Propipocaína; Propipocaïne; Propipocainum; Propoxypipero- (USAN); Dimethisoquinium Chloride; Hidrocloruro de quinisocaí- NH2 caine. 3-Piperidino-4′-propoxypropiophenone. na; Quinisocaïne, Chlorhydrate de; Quinisocaini Hydrochlori- (proxymetacaine) dum. 2-(3-Butyl-1-isoquinolyloxy)-NN-dimethylethylamine hy- Пропипокаин drochloride. C17H25NO2 = 275.4. Хинизокаина Гидрохлорид CAS — 3670-68-6. NOTE. PROX is a code approved by the BP 2008 for use on single unit doses of eye drops containing proxymetacaine hydrochlo- C17H24N2O,HCl = 308.8. ride where the individual container may be too small to bear all CAS — 86-80-6 (quinisocaine); 2773-92-4 (quinisocaine the appropriate labelling information. PROXFLN is a similar hydrochloride). O code approved for eye drops containing proxymetacaine hydro- ATC — D04AB05. chloride and fluorescein sodium. ATC Vet — QD04AB05. N Pharmacopoeias. In Br. and US. BP 2008 (Proxymetacaine Hydrochloride). A white or almost H3C CH3 white, odourless or almost odourless, crystalline powder. Soluble O in water and in chloroform; very soluble in dehydrated alcohol; N practically insoluble in ether. A 1% solution in water has a pH of O CH Profile 5.7 to 6.4. Protect from light. 3 Propipocaine is a local anaesthetic (p.1850) that has been used USP 31 (Proparacaine Hydrochloride). A white to off-white, or for surface anaesthesia. -

Evidence-Based Guidelines for Treating Depressive Disorders with Antidepressants
JOP0010.1177/0269881115581093Journal of PsychopharmacologyCleare et al. 581093research-article2015 BAP Guidelines Evidence-based guidelines for treating depressive disorders with antidepressants: A revision of the 2008 British Association Journal of Psychopharmacology 2015, Vol. 29(5) 459 –525 for Psychopharmacology guidelines © The Author(s) 2015 Reprints and permissions: sagepub.co.uk/journalsPermissions.nav DOI: 10.1177/0269881115581093 jop.sagepub.com Anthony Cleare1, CM Pariante2 and AH Young3 With expert co-authors (in alphabetical order): IM Anderson4, D Christmas5, PJ Cowen6, C Dickens7, IN Ferrier8, J Geddes9, S Gilbody10, PM Haddad11, C Katona12, G Lewis12, A Malizia13, RH McAllister-Williams14, P Ramchandani15, J Scott16, D Taylor17, R Uher18 and the members of the Consensus Meeting19 Endorsed by the British Association for Psychopharmacology Abstract A revision of the 2008 British Association for Psychopharmacology evidence-based guidelines for treating depressive disorders with antidepressants was undertaken in order to incorporate new evidence and to update the recommendations where appropriate. A consensus meeting involving experts in depressive disorders and their management was held in September 2012. Key areas in treating depression were reviewed and the strength of evidence and clinical implications were considered. The guidelines were then revised after extensive feedback from participants and interested parties. A literature review is provided which identifies the quality of evidence upon which the recommendations -

Evaluation of Liposomal Delivery System for Topical Anesthesia
THERAPEUTICS FOR THE CLINICIAN Evaluation of Liposomal Delivery System for Topical Anesthesia Mohamed L. Elsaie, MD, MBA; Leslie S. Baumann, MD Local anesthesia is an integral aspect of cutane- infiltrative anesthetics, now can be accomplished ous surgery. Its effects provide a reversible loss safely and comfortably with the use of topi- of sensation in a limited area of skin, allowing cal anesthetics.1 Topical anesthetics originated in dermatologists to perform diagnostic and thera- South America; native Peruvians noted perioral peutic procedures safely, with minimal discomfort numbness when chewing the leaf of the cocoa plant and risk to the patient. Moreover, the skin acts (Erythroxylon coca). The active alkaloid, cocaine, was as a major target as well as principle barrier for isolated by Niemann in 1860 and applied to con- topical/transdermal (TT) drug delivery. The stra- junctival mucosa for topical anesthesia by Koller in tum corneum (SC) plays a crucial role in barrier 1884. The development of similar benzoic acid esters function for TT drug delivery. Despite the major continued until 1943 when Loefgren synthesized lido- research and development efforts in TT systems caine hydrochloride, the first amide anesthetic.2 and their implementation for use of topical anes- We review the administration of local anes- thetics, low SC permeability limits the useful- thetics, specifically the liposomal delivery system ness of topical delivery, which has led to other for topical anesthesia, based on a review of the delivery system developments, including vesicu- literature and clinical experience. lar systems such as liposomes, niosomes, and proniosomes, with effectiveness relying on their Anatomy physiochemical properties. -

Prolonged Duration Topical Corneal Anesthesia with the Cationic Lidocaine Derivative QX-314
https://doi.org/10.1167/tvst.8.5.28 Article Prolonged Duration Topical Corneal Anesthesia With the Cationic Lidocaine Derivative QX-314 Alan G. Woodruff1,2, Claudia M. Santamaria1, Manisha Mehta1,2, Grant L. Pemberton1, Kathleen Cullion1,2,4, and Daniel S. Kohane1,2,3 1 Kohane Lab for Biomaterials and Drug Delivery, Department of Anesthesia, Perioperative and Pain Medicine, Division of Critical Care, Boston Children’s Hospital, Boston, MA, USA 2 Harvard Medical School, Boston, MA, USA 3 David H. Koch Institute, Massachusetts Institute of Technology, Cambridge, MA, USA 4 Department of Medicine, Division of Medicine Critical Care, Boston Children’s Hospital, Harvard Medical School, Boston, MA, USA Correspondence: Daniel S. Kohane, Purpose: Topical corneal local anesthetics are short acting and may impair corneal Laboratory for Biomaterials and healing. In this study we compared corneal anesthesia and toxicity of topically applied Drug Delivery, Department of Anes- N-ethyl lidocaine (QX-314) versus the conventional local anesthetic, proparacaine thesia, Division of Critical Care (PPC). Medicine, Boston Children’s Hospi- tal, Harvard Medical School, 61 Methods: Various concentrations of QX-314 and 15 mM (0.5%) PPC were topically Binney Street, Room 361, Boston, applied to rat corneas. Corneal anesthesia was assessed with a Cochet-Bonnet MA 02115, USA. e-mail: Daniel. esthesiometer at predetermined time points. PC12 cells were exposed to the same [email protected] solutions to assess cytotoxicity. Repeated topical corneal administration in rats was then used to assess for histologic evidence of toxicity. Finally, we created uniform Received: 6 May 2019 corneal epithelial defects in rats and assessed the effect of repeated administration of Accepted: 15 August 2019 these compounds on the defect healing rate. -

First Part Examination Mock Exam
FIRST PART EXAMINATION MOCK EXAM This Mock Examination is prepared to provide candidates, tutors and their Supervisors of Training with information about the way the Examiners will assess the performance of candidates in the Examination. Example questions provided are to be used as a guide only as to what may be expected. Candidates should discuss the exam with their tutors so that they may prepare appropriately for future examinations. It should be read in conjunction with the Notes to Candidates document. WRITTEN EXAM GLOSSARY OF TERMS Calculate Work out or estimate using mathematical principles Classify Divide into categories; organise, arrange Compare Examine similarities and differences Define Give the precise meaning Describe Give a detailed account of Explain Make plain, interpret, and account for Interpret Explain the meaning or significance Outline Provide a summary of the important points Relate Show a connection between Understand Appreciate the details of; comprehend 1 FIRST PART EXAMINATION MOCK EXAM SHORT ANSWER QUESTIONS MORNING PAPER (A) Start each answer on a new page and indicate the question number. It is not necessary to rewrite the question in your answer book. (B) You should aim to allocate ten minutes to answer each SAQ. (C) The questions are worth equal marks. (D) Short Answer Questions with more than one part have the proportion of marks indicated for each part. (E) Record your candidate number and each question number on the cover of each book and hand in all answer books. 2 Please answer Questions 1 and 2 in the blue answer booklet 1. Describe the anatomy of the left subclavian vein. -

(DMT), Harmine, Harmaline and Tetrahydroharmine: Clinical and Forensic Impact
pharmaceuticals Review Toxicokinetics and Toxicodynamics of Ayahuasca Alkaloids N,N-Dimethyltryptamine (DMT), Harmine, Harmaline and Tetrahydroharmine: Clinical and Forensic Impact Andreia Machado Brito-da-Costa 1 , Diana Dias-da-Silva 1,2,* , Nelson G. M. Gomes 1,3 , Ricardo Jorge Dinis-Oliveira 1,2,4,* and Áurea Madureira-Carvalho 1,3 1 Department of Sciences, IINFACTS-Institute of Research and Advanced Training in Health Sciences and Technologies, University Institute of Health Sciences (IUCS), CESPU, CRL, 4585-116 Gandra, Portugal; [email protected] (A.M.B.-d.-C.); ngomes@ff.up.pt (N.G.M.G.); [email protected] (Á.M.-C.) 2 UCIBIO-REQUIMTE, Laboratory of Toxicology, Department of Biological Sciences, Faculty of Pharmacy, University of Porto, 4050-313 Porto, Portugal 3 LAQV-REQUIMTE, Laboratory of Pharmacognosy, Department of Chemistry, Faculty of Pharmacy, University of Porto, 4050-313 Porto, Portugal 4 Department of Public Health and Forensic Sciences, and Medical Education, Faculty of Medicine, University of Porto, 4200-319 Porto, Portugal * Correspondence: [email protected] (D.D.-d.-S.); [email protected] (R.J.D.-O.); Tel.: +351-224-157-216 (R.J.D.-O.) Received: 21 September 2020; Accepted: 20 October 2020; Published: 23 October 2020 Abstract: Ayahuasca is a hallucinogenic botanical beverage originally used by indigenous Amazonian tribes in religious ceremonies and therapeutic practices. While ethnobotanical surveys still indicate its spiritual and medicinal uses, consumption of ayahuasca has been progressively related with a recreational purpose, particularly in Western societies. The ayahuasca aqueous concoction is typically prepared from the leaves of the N,N-dimethyltryptamine (DMT)-containing Psychotria viridis, and the stem and bark of Banisteriopsis caapi, the plant source of harmala alkaloids. -

Royal Free Hospital Drug Formulary
Royal Free Hospital Drug Formulary Title Formulary Status Section Annotation 5.3 Antiviral drugs‐>5.3.1 HIV infection‐>Nucleoside reverse ABACAVIR On Formulary transcriptase inhibitors As per HIV guidelines. Abidec® On Formulary 9.6 Vitamins‐>9.6.7 Multivitamin preparations 4.10 Drugs used in substance dependence‐>4.10.1 Alcohol ACAMPROSATE CALCIUM On Formulary dependence‐>Acamprosate 6.1 Drugs used in diabetes‐>6.1.2 Antidiabetic drugs‐>6.1.2.3 Other ACARBOSE On Formulary antidiabetic drugs 11.6 Treatment of glaucoma‐>Carbonic anhydrase inhibitors and ACETAZOLAMIDE On Formulary systemic drugs 11.8 Miscellaneous ophthalmic preparations‐>11.8.2 Ocular diagnostic and peri‐operative preparations and photodynamic ACETYLCHOLINE CHLORIDE On Formulary treatment‐>Ocular peri‐operative drugs ACETYLCYSTEINE On Formulary Specific drugs‐>Analgesics (non‐opioid) Acetylcysteine On Formulary Specific drugs‐>Analgesics (non‐opioid)‐>ACETYLCYSTEINE 11.8 Miscellaneous ophthalmic preparations‐>11.8.1 Tear deficiency, ACETYLCYSTEINE On Formulary ocular lubricants, and astringents ACICLOVIR On Formulary 11.3 Anti‐infective eye preparations‐>11.3.3 Antivirals ACICLOVIR On Formulary 13.10 Anti‐infective skin preparations‐>13.10.3 Antiviral preparations 13.10 Anti‐infective skin preparations‐>13.10.3 Antiviral preparations‐ Aciclovir On Formulary >ACICLOVIR 13.5 Preparations for eczema and psoriasis‐>13.5.2 Preparations for ACITRETIN On Formulary psoriasis‐>Oral retinoids for psoriasis Removal and elimination‐>Removal from the gastro‐intestinal tract‐ Actidose‐Aqua® -

Receptor Antagonist
Gut: first published as 10.1136/gut.29.7.890 on 1 July 1988. Downloaded from Gut, 1988, 29, 890-893 Alteration of H2 receptor sensitivity in duodenal ulcer patients after maintenance treatment with an H2 receptor antagonist D B JONES, C W HOWDEN, D W BURGET, CINDY SILLETTI, AND R H HUNT From the Division of Gastroenterology, McMaster University Medical Centre, Hamilton, Ontario, Canada SUMMARY The effects of a specific H2 receptor agonist impromidine, on gastric acid secretion were measured in six patients with duodenal ulcer in clinical remission before and after three months treatment with ranitidine 150 mg nocte. After treatment basal acid output increased from 1 2 to 2-8 mmol/h and after maximal impromidine stimulation from 36-9 (4 7) to 44-2 (6 2) mmol/h (p<002). Intravenous ranitidine 50 mg was given at the end ofthe impromidine infusion on each study day; the antisecretory effect of intravenous ranitidine was accentuated after the treatment with ranitidine from a trough acid output of8 5 (1-2) mmol/h before, to 3-8 (1-5) mmol/h (p<0 05) after, treatment. The increased response to the H2 agonist impromidine and the H2 antagonist ranitidine after treatment with ranitidine suggests an enhanced sensitivity of the H2 receptor. This might be ex- plained on the basis of an increase in the number of H2 receptors ('up-regulation'). http://gut.bmj.com/ The discovery of the histamine H2 receptor on the a highly potent, and specific agonist for the H2 parietal cell' initiated the development of H2 receptor' exhibiting up to 27 times the affinity of receptor antagonists with potent gastric antisecretory histamine.9 In this study we have examined the effect activity and these agents have now become firmly of three months of treatment with ranitidine 150 mg established in the treatment of peptic ulceration.- nocte on impromidine stimulated gastric acid secre- After heaing of duodenal ulcer by the H2 receptor tion in six patients with duodenal ulcer in remission. -

Local Anesthetics – Substances with Multiple Application in Medicine
ISSN 2411-958X (Print) European Journal of January-April 2016 ISSN 2411-4138 (Online) Interdisciplinary Studies Volume 2, Issue 1 Local Anesthetics – Substances with Multiple Application in Medicine Rodica SÎRBU Ovidius University of Constanta, Faculty of Pharmacy, Campus Corp B, University Alley No. 1, Constanta, Romania Emin CADAR UMF Carol Davila Bucharest, Faculty of Pharmacy, Str. Traian Vuia No. 6, Sector 2, Bucharest, Romania Cezar Laurențiu TOMESCU Ovidius University of Constanta, Faculty of Medicine, Campus Corp B, University Alley No. 1, Constanta, Romania Cristina-Luiza ERIMIA Corresponding author, [email protected] Ovidius University of Constanta, Faculty of Pharmacy, Campus Corp B, University Alley No. 1, Constanta, Romania Stelian PARIS Ovidius University of Constanta, Faculty of Pharmacy, Campus Corp B, University Alley No. 1, Constanta, Romania Aneta TOMESCU Ovidius University of Constanta, Faculty of Medicine, Campus Corp B, University Alley No. 1, Constanta, Romania Abstract Local anesthetics are substances which, by local action groups on the runners, cause loss of reversible a painful sensation, delimited corresponding to the application. They allow small surgery, short in duration and the endoscopic maneuvers. May be useful in soothe teething pain of short duration and in the locking of the nervous disorders in medical care. Local anesthesia is a process useful for the carrying out of surgery and of endoscopic maneuvers, to soothe teething pain in certain conditions, for depriving the temporary structures peripheral nervous control. Reversible locking of the transmission nociceptive, the set of the vegetative and with a local anesthetic at the level of the innervations peripheral nerve, roots and runners, a trunk nervous, around the components of a ganglion or coolant is cefalorahidian practice anesthesia loco-regional. -

Topical Treatments of Skin Pain Associated with Hidradenitis Supprurativa
UC Davis Dermatology Online Journal Title Topical treatments of skin pain: a general review with a focus on hidradenitis suppurativa with topical agents Permalink https://escholarship.org/uc/item/4m57506k Journal Dermatology Online Journal, 20(7) Author Scheinfeld, Noah Publication Date 2014 DOI 10.5070/D3207023131 License https://creativecommons.org/licenses/by-nc-nd/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Volume 20 Number 7 July 2014 Review Topical treatments of skin pain: a general review with a focus on hidradenitis suppurativa with topical agents Noah Scheinfeld MD JD Dermatology Online Journal 20 (7): 3 Assistant Clinical Professor of Dermatology Weil Cornel Medical College Correspondence: Noah Scheinfeld 150 West 55th Street NYC NY 10019 (212) 991-6490 [email protected] Abstract Hidradenitis Supprurativa (HS) is a painful chronic follicular disease. Few papers have addressed pain control for this debilitating condition. Possible topical agents include tricyclic antidepressants, opioids, anticonvulsants, NSAIDs, NMDA receptor antagonists, local anesthetics and other agents. The first line agents for the topical treatment of the cutaneous pain of HS are diclonefac gel 1% and liposomal xylocaine 4% and 5% cream or 5% ointment. The chief advantage of topical xylocaine is that is quick acting i.e. immediate however with a limited duration of effect 1-2 hours. The use of topical ketamine, which blocks n- methyl-D-aspartate receptors in a non-competitive fashion, might be a useful tool for the treatment of HS pain. Topical doxepin, which available in a 5% commercially preparation (Zonalon®) , makes patients drowsy and is not useful for controlling the pain of HS .