Local Anesthetics – Substances with Multiple Application in Medicine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Appendix 1 Table of Contents
@ECHA EUROPEAN CHEMICALS AGENCY Appendix 1 Table of Contents: Supplementary Table C:Substances on Annex II of the Cosmetic Products Regulation ... 1 Supplementary Table D: Substances proposed to be restricted due their use restriction in CPR Annex IV column 9..,,.. 119 Supplementary Table E: Substances allowed in tattoo inks subject to the conditions specified in CPR Annex IV columns h and i ......r29 Annankatu 18. P.O. Box 400, FI-00121 Helsinki, Finland I Tel. +358 9 686180 | Fax +358 9 68618210 | echa.europa.eu ANNEX XV RESTRICTION REPORT - SUBSTANCES IN TATTOO INKS AND PERMANENT MAKE UP Su lemen Table C:Substances on Annex II of the Cosmetic Products Re ulationl Substance EC# cAs # Substance EC# cAs # R T T T A- s c R I T Name Name e b b b II s M 7 c I s I I I #4 5 6 D 9 2 1 2 3 a 3 3 3 N-(s- Chlorobenzoxa zol-2- 35783- vl)acetamide 57-4 1 (2- Acetoxyethyl)t rimethylammo (2- nium acetoxyethyl hydroxide )trimethyla 200- (Acetylcholine) 200- mmonium 124-9 5 1-84-3 and its salts t2a-9 51-84-3 2 Deanol Deanol 222- 3342- aceglumate 222- 3342- aceqlumate 085-5 61-8 (INN) 085-5 61-8 3 Spironolacto 200- Spironolactone 200- ne 133-6 52-O1-7 rINN) 133-6 52-0L-7 4 14-(4- Hydroxy-3- iodophenoxy)- 3,5- diiodophenylla cetic acid (Tiratricol 200- (INN)) and its 200- Tiratricol 086- 1 5r-24-7 salts 086- 1 5l-24-7 5 Methotrexat 200- Methotrexate 200- e 413-8 59-05-2 (INN) 413-8 59-05-2 6 Aminocaproic Aminocaproi 200- acid (INN) and 200- c acid 469-3 60-32-2 its salts 469-3 60-32-2 7 Cinchophen (rNN), its salts, derivatives and salts of 205- 132-60- these 205- 132-60- Cinchophen 067-r 5 derivatives 067-l 5 Thyropropic acid (INN) and its salts 5L-26-3 9 Trichloroacet 200- Trichloroacetic 200- ic acid 927-2 75-03-9 acid 927-2 76-03-9 l0 Aconitum napellus L. -
Europæisk Patentskrift
(19) DANMARK (1°) DK/EP 2968225 T3 (12) Oversættelse af europæisk patentskrift Patent- og Varemærkestyrelsen (51) lnt.CI.: A 61 K 31/137 (2006.01) A 61 K 9/00 (2006.01) A 61 K 31/245 (2006.01) A 61 K 31/445 (2006.01) A 61 K 31/519 (2006.01) A 61 K 31/52 (2006.01) A 61 P 43/00 (2006.01) (45) Oversættelsen bekendtgjort den: 2019-05-27 (80) Dato for Den Europæiske Patentmyndigheds bekendtgørelse om meddelelse af patentet: 2019-02-20 (86) Europæisk ansøgning nr.: 14719486.4 (86) Europæisk indleveringsdag: 2014-03-17 (87) Den europæiske ansøgnings publiceringsdag: 2016-01-20 (86) International ansøgning nr.: US2014030372 (87) Internationalt publikationsnr.: WO2014145580 (30) Prioritet: 2013-03-15 US 201361789054 P (84) Designerede stater: AL AT BE BG CH CY CZ DE DK EE ES Fl FR GB GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL PT RO RS SE SI SK SM TR (73) Patenthaver: The Children's Medical Center Corporation, 55 Shattuck Street, Boston, Massachusetts 02115, USA (72) Opfinder: BERDE, Charles, 14 Doran Road, Bookline, MA 02146, USA KOHANE, Daniel S., 119 Willard Street, Newton, MA 02461, USA (74) Fuldmægtig i Danmark: AWA Denmark A/S, Strandgade 56,1401 København K, Danmark (54) Benævnelse: NEOSAXITOXINKOMBINATIONSFORMULERINGER TIL FORLÆNGET LOKALANÆSTESI (56) Fremdragne publikationer: WO-A2-98/51290 ALBERTO J. RODRIGUEZ-NAVARRO ET AL: "Potentiation of Local Anesthetic Activity of Neosaxitoxin with Bupivacaine or Epinephrine: Development of a Long-Acting Pain Blocker", NEUROTOXICITY RESEARCH, vol. 16, no. 4, 28 July 2009 (2009-07-28), pages 408-415, XP055122925, ISSN: 1029-8428, DOI: 10.1007/s12640-009- 9092-3 cited in the application Anonymous: "NCT01786655 on 2013_02_11: ClinicalTrials.gov Archive",, 11 February 2013 (2013-02-11), XP055122935, Retrieved from the Internet: URL:http://clinicaltrials.gov/archive/NCTO 1786655/2013_02_11 [retrieved on 2014-06-12] CHARLES B. -

Journal of Pharmacology and Experimental Therapeutics
Journal of Pharmacology and Experimental Therapeutics Molecular Determinants of Ligand Selectivity for the Human Multidrug And Toxin Extrusion Proteins, MATE1 and MATE-2K Bethzaida Astorga, Sean Ekins, Mark Morales and Stephen H Wright Department of Physiology, University of Arizona, Tucson, AZ 85724, USA (B.A., M.M., and S.H.W.) Collaborations in Chemistry, 5616 Hilltop Needmore Road, Fuquay-Varina NC 27526, USA (S.E.) Supplemental Table 1. Compounds selected by the common features pharmacophore after searching a database of 2690 FDA approved compounds (www.collaborativedrug.com). FitValue Common Name Indication 3.93897 PYRIMETHAMINE Antimalarial 3.3167 naloxone Antidote Naloxone Hydrochloride 3.27622 DEXMEDETOMIDINE Anxiolytic 3.2407 Chlordantoin Antifungal 3.1776 NALORPHINE Antidote Nalorphine Hydrochloride 3.15108 Perfosfamide Antineoplastic 3.11759 Cinchonidine Sulfate Antimalarial Cinchonidine 3.10352 Cinchonine Sulfate Antimalarial Cinchonine 3.07469 METHOHEXITAL Anesthetic 3.06799 PROGUANIL Antimalarial PROGUANIL HYDROCHLORIDE 100MG 3.05018 TOPIRAMATE Anticonvulsant 3.04366 MIDODRINE Antihypotensive Midodrine Hydrochloride 2.98558 Chlorbetamide Antiamebic 2.98463 TRIMETHOPRIM Antibiotic Antibacterial 2.98457 ZILEUTON Antiinflammatory 2.94205 AMINOMETRADINE Diuretic 2.89284 SCOPOLAMINE Antispasmodic ScopolamineHydrobromide 2.88791 ARTICAINE Anesthetic 2.84534 RITODRINE Tocolytic 2.82357 MITOBRONITOL Antineoplastic Mitolactol 2.81033 LORAZEPAM Anxiolytic 2.74943 ETHOHEXADIOL Insecticide 2.64902 METHOXAMINE Antihypotensive Methoxamine -

Bupivacaine Injection Bp
PRODUCT MONOGRAPH INCLUDING CONSUMER INFORMATION BUPIVACAINE INJECTION BP Bupivacaine hydrochloride 0.25% (2.5 mg/mL) and 0.5% (5 mg/mL) Local Anaesthetic SteriMax Inc. Date of Preparation: 2770 Portland Dr. July 10, 2015 Oakville, ON, L6H 6R4 Submission Control No: 180156 Bupivacaine Injection Page 1 of 28 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION .................................................................... 3 SUMMARY PRODUCT INFORMATION ................................................................................... 3 INDICATIONS AND CLINICAL USE ......................................................................................... 3 CONTRAINDICATIONS .............................................................................................................. 3 WARNINGS AND PRECAUTIONS ............................................................................................. 4 ADVERSE REACTIONS ............................................................................................................... 9 DRUG INTERACTIONS ............................................................................................................. 10 DOSAGE AND ADMINISTRATION ......................................................................................... 13 OVERDOSAGE ........................................................................................................................... 16 ACTION AND CLINICAL PHARMACOLOGY ....................................................................... 18 STORAGE -

A Randomised, Non-Inferiority Study of Chloroprocaine 2% and Ropivacaine
www.nature.com/scientificreports OPEN A randomised, non‑inferiority study of chloroprocaine 2% and ropivacaine 0.75% in ultrasound‑guided axillary block Irene Sulyok1, Claudio Camponovo2, Oliver Zotti1, Werner Haslik3, Markus Köstenberger4, Rudolf Likar4, Chiara Leuratti5, Elisabetta Donati6 & Oliver Kimberger1,7* Chloroprocaine is a short‑acting local anaesthetic with a rapid onset of action and an anaesthesia duration up to 60 min. In this pivotal study success rates, onset and remission of motor and sensory block and safety of chloroprocaine 2% was compared to ropivacaine 0.75% for short‑duration distal upper limb surgery with successful block rates as primary outcome. The study was designed as a prospective, randomised, multi‑centre, active‑controlled, double‑blind, parallel‑group, non‑inferiority study, performed in 4 European hospitals with 211 patients scheduled for short duration distal upper limb surgery under axillary plexus block anaesthesia. Patients received either ultrasound guided axillary block with 20 ml chloroprocaine 2%, or with 20 ml ropivacaine 0.75%. Successful block was defned as block without any supplementation in the frst 45 min calculated from the time of readiness for surgery. 90.8% patients achieved a successful block with chloroprocaine 2% and 92.9% patients with Ropivacaine 0.75%, thus non‑inferiority was demonstrated (10% non inferiority margin; 95% CI − 0.097, 0.039; p = 0.02). Time to onset of block was not signifcantly diferent between the groups. Median time to motor and sensory block regression was signifcantly shorter as was time to home discharge (164 [155–170] min for chloroprocaine versus 380 [209–450] for the ropivacaine group, p < 0.001). -

The National Drugs List
^ ^ ^ ^ ^[ ^ The National Drugs List Of Syrian Arab Republic Sexth Edition 2006 ! " # "$ % &'() " # * +$, -. / & 0 /+12 3 4" 5 "$ . "$ 67"5,) 0 " /! !2 4? @ % 88 9 3: " # "$ ;+<=2 – G# H H2 I) – 6( – 65 : A B C "5 : , D )* . J!* HK"3 H"$ T ) 4 B K<) +$ LMA N O 3 4P<B &Q / RS ) H< C4VH /430 / 1988 V W* < C A GQ ") 4V / 1000 / C4VH /820 / 2001 V XX K<# C ,V /500 / 1992 V "!X V /946 / 2004 V Z < C V /914 / 2003 V ) < ] +$, [2 / ,) @# @ S%Q2 J"= [ &<\ @ +$ LMA 1 O \ . S X '( ^ & M_ `AB @ &' 3 4" + @ V= 4 )\ " : N " # "$ 6 ) G" 3Q + a C G /<"B d3: C K7 e , fM 4 Q b"$ " < $\ c"7: 5) G . HHH3Q J # Hg ' V"h 6< G* H5 !" # $%" & $' ,* ( )* + 2 ا اوا ادو +% 5 j 2 i1 6 B J' 6<X " 6"[ i2 "$ "< * i3 10 6 i4 11 6! ^ i5 13 6<X "!# * i6 15 7 G!, 6 - k 24"$d dl ?K V *4V h 63[46 ' i8 19 Adl 20 "( 2 i9 20 G Q) 6 i10 20 a 6 m[, 6 i11 21 ?K V $n i12 21 "% * i13 23 b+ 6 i14 23 oe C * i15 24 !, 2 6\ i16 25 C V pq * i17 26 ( S 6) 1, ++ &"r i19 3 +% 27 G 6 ""% i19 28 ^ Ks 2 i20 31 % Ks 2 i21 32 s * i22 35 " " * i23 37 "$ * i24 38 6" i25 39 V t h Gu* v!* 2 i26 39 ( 2 i27 40 B w< Ks 2 i28 40 d C &"r i29 42 "' 6 i30 42 " * i31 42 ":< * i32 5 ./ 0" -33 4 : ANAESTHETICS $ 1 2 -1 :GENERAL ANAESTHETICS AND OXYGEN 4 $1 2 2- ATRACURIUM BESYLATE DROPERIDOL ETHER FENTANYL HALOTHANE ISOFLURANE KETAMINE HCL NITROUS OXIDE OXYGEN PROPOFOL REMIFENTANIL SEVOFLURANE SUFENTANIL THIOPENTAL :LOCAL ANAESTHETICS !67$1 2 -5 AMYLEINE HCL=AMYLOCAINE ARTICAINE BENZOCAINE BUPIVACAINE CINCHOCAINE LIDOCAINE MEPIVACAINE OXETHAZAINE PRAMOXINE PRILOCAINE PREOPERATIVE MEDICATION & SEDATION FOR 9*: ;< " 2 -8 : : SHORT -TERM PROCEDURES ATROPINE DIAZEPAM INJ. -

4% Citanest® Plain Dental (Prilocaine Hydrochloride Injection, USP) for Local Anesthesia in Dentistry
4% Citanest® Plain Dental (Prilocaine Hydrochloride Injection, USP) For Local Anesthesia in Dentistry Rx only DESCRIPTION 4% Citanest Plain Dental (prilocaine HCI Injection, USP), is a sterile, non-pyrogenic isotonic solution that contains a local anesthetic agent and is administered parenterally by injection. See INDICATIONS AND USAGE for specific uses. The quantitative composition is shown in Table 1. 4% Citanest Plain Dental contains prilocaine HCl, which is chemically designated as propanamide, N-(2- methyl-phenyl) -2- (propylamino)-, monohydrochloride and has the following structural formula: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration. The specific quantitative composition is shown in Table 1. TABLE 1. COMPOSITION Product Identification Formula (mg/mL) Prilocaine HCl pH 4% Citanest® Plain Dental 40.0 6.0 to 7.0 Note: Sodium hydroxide or hydrochloric acid may be used to adjust the pH of 4% Citanest Plain Dental Injection. CLINICAL PHARMACOLOGY Mechanism of Action: Prilocaine stabilizes the neuronal membrane by inhibiting the ionic fluxes required for the initiation and conduction of impulses, thereby effecting local anesthetic action. Onset and Duration of Action: When used for infiltration injection in dental patients, the time of onset of anesthesia averages less than 2 minutes with an average duration of soft tissue anesthesia of approximately 2 hours. Based on electrical stimulation studies, 4% Citanest Plain Dental Injection provides a duration of pulpal anesthesia of approximately 10 minutes in maxillary infiltration injections. In clinical studies, this has been found to provide complete anesthesia for procedures lasting an average of 20 minutes. When used for inferior alveolar nerve block, the time of onset of 4% Citanest Plain Dental Injection averages less than three minutes with an average duration of soft tissue anesthesia of approximately 2 ½hours. -

Subject Index
52_1107_1136_SI 16.11.2005 9:35 Uhr Seite 1107 Subject Index A – tape 264, 368, 940 α-adjustment 154 AAS, see atomic absorption spectrophotometry adrenocorticotrophic hormone (ACTH) 21 abietic acid 909, 943 adverse drug reaction 401 abrasion 174, 283 aeroallergen 391 absorption through appendage 169 – atopic eczema 391 α-acaridial 329 – avoidance 391 accident 889 aerospace 726 acebutolol hydrochloride 909 African aceclofenac 909 –ebony783 acetaldehyde 943 – mahagony 783 acetone 118, 666 – red padauk wood 783 acetylacetone 697 Agave acetylsalicylic acid 84, 909 – americana 354 Achillea millefolium (yarrow extract) 909 – tequilana 225 aciclovir 909 age 279 acid 110 agent orange 806 – black 48 (CI 65005) 909 AGEP 404 – dye 689 Agfa TSS 355 – halogenated 259 aggravation 204 –hydrochloric261 agricultural worker 272 –nitric261 agriculture 725 –red AICD, see activation-induced cell death – – 14 (azorubine) 909 airborne – – 118 (CI 26410) 909 – allergic contact dermatitis 218, 228, 315, 467, 477, 484, 598, ––359909 627, 654, 788 – violet 17 (CI 42650) 909 – contact urticaria 753, 758 – yellow – irritant contact dermatitis 625 – – 36 (CI 13065, metanil yellow) 909 aircraft manufacture 560 – – 61 (CI 18968) 909 airway symptom 520 acitretin 341 alachlor 953 acneiform alantolactone 55, 789, 909, 954 – folliculitis 229 alclometasone-17,21-dipropionate 909 –lesion265 alclometasone-17-propionate 58 acrodermatitis enteropathica 241 alcohol, see also ethyl 909 acrovesicular dermatitis 401 aldehyde 110, 607, 886 acrylamide 592, 944 algicide 562 acrylate -

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -
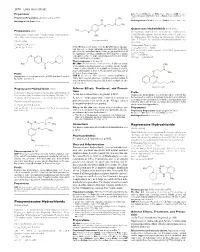
Proxymetacaine Hydrochloride Ropivacaine Hydrochloride
1870 Local Anaesthetics Preparations pore: Alcaine; Switz.: Alcaine; Turk.: Alcaine; Opticaine; USA: Ak-Taine; Alcaine; Ocu-Caine; Ophthetic; Parcaine; Venez.: Alcaine; Oftaine†; Poen- (details are given in Part 3) caina. Proprietary Preparations CH3 Multi-ingredient: Spain: Detraine. O Multi-ingredient: Canad.: Fluoracaine†; USA: Fluoracaine; Fluorocaine. N CH3 O Quinisocaine Hydrochloride (BANM, rINNM) H3C Propipocaine (rINN) O Chinisocainum Hydrochloride; Dimethisoquin Hydrochloride Propipocaína; Propipocaïne; Propipocainum; Propoxypipero- (USAN); Dimethisoquinium Chloride; Hidrocloruro de quinisocaí- NH2 caine. 3-Piperidino-4′-propoxypropiophenone. na; Quinisocaïne, Chlorhydrate de; Quinisocaini Hydrochlori- (proxymetacaine) dum. 2-(3-Butyl-1-isoquinolyloxy)-NN-dimethylethylamine hy- Пропипокаин drochloride. C17H25NO2 = 275.4. Хинизокаина Гидрохлорид CAS — 3670-68-6. NOTE. PROX is a code approved by the BP 2008 for use on single unit doses of eye drops containing proxymetacaine hydrochlo- C17H24N2O,HCl = 308.8. ride where the individual container may be too small to bear all CAS — 86-80-6 (quinisocaine); 2773-92-4 (quinisocaine the appropriate labelling information. PROXFLN is a similar hydrochloride). O code approved for eye drops containing proxymetacaine hydro- ATC — D04AB05. chloride and fluorescein sodium. ATC Vet — QD04AB05. N Pharmacopoeias. In Br. and US. BP 2008 (Proxymetacaine Hydrochloride). A white or almost H3C CH3 white, odourless or almost odourless, crystalline powder. Soluble O in water and in chloroform; very soluble in dehydrated alcohol; N practically insoluble in ether. A 1% solution in water has a pH of O CH Profile 5.7 to 6.4. Protect from light. 3 Propipocaine is a local anaesthetic (p.1850) that has been used USP 31 (Proparacaine Hydrochloride). A white to off-white, or for surface anaesthesia. -

List of Union Reference Dates A
Active substance name (INN) EU DLP BfArM / BAH DLP yearly PSUR 6-month-PSUR yearly PSUR bis DLP (List of Union PSUR Submission Reference Dates and Frequency (List of Union Frequency of Reference Dates and submission of Periodic Frequency of submission of Safety Update Reports, Periodic Safety Update 30 Nov. 2012) Reports, 30 Nov. -

The Effect of Different Doses of Chloroprocaine on Saddle Anesthesia in Perianal Surgery1
10 – ORIGINAL ARTICLE CLINICAL INVESTIGATION The effect of different doses of chloroprocaine on saddle anesthesia in perianal surgery1 Ying ZhangI, Yang BaoII, Linggeng LiIII, Dongping ShiIV IMaster, Department of Anesthesiology, Shanghai Jiading Central Hospital, Shanghai, China. Conception and design of the study; acquisition, analysis and interpretation of data; manuscript writing, final approval. IIMaster, Department of Anesthesiology, Shanghai Jiading Central Hospital, Shanghai, China. Conception and design of the study, analysis and interpretation of data, critical revision. IIIMaster, Department of Anesthesiology, Shanghai Jiading Central Hospital, Shanghai, China. Histopathological examinations, critical revision. IVMaster, Department of Anesthesiology, Shanghai Jiading Central Hospital, Shanghai, China. Acquisition and interpretation of data, final approval. ABSTRACT PURPOSE: To investigate a saddle anesthesia with different doses of chloroprocaine in perianal surgery. METHODS: Total 60 Patients aged 18–75 years (Anesthesiologists grade I or II) scheduled to receive perianal surgery. Patients using saddle anesthesia were randomized to group A, group B and group C with the same concentration (0.5%) chloroprocaine with different doses 1.0 mL, 0.8 mL and 0.6 mL, respectively. Systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR) and the sensory and motor block were recorded to evaluate the anesthesia effect of chloroprocaine in each group. RESULTS: The duration of sensory block of group C is shorter than those of group A and B. The maximum degree of motor block is observed (group C: 0 level, group A: III level; and group B: I level) after 15 minutes. Besides, there was a better anesthetic effect in group B than group A and group C, such as walking after saddle anesthesia.