Genetic Complexity of Autosomal Dominant Polycystic Kidney and Liver Diseases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glycoproteomics-Based Signatures for Tumor Subtyping and Clinical Outcome Prediction of High-Grade Serous Ovarian Cancer
ARTICLE https://doi.org/10.1038/s41467-020-19976-3 OPEN Glycoproteomics-based signatures for tumor subtyping and clinical outcome prediction of high-grade serous ovarian cancer Jianbo Pan 1,2,3, Yingwei Hu1,3, Shisheng Sun 1,3, Lijun Chen1, Michael Schnaubelt1, David Clark1, ✉ Minghui Ao1, Zhen Zhang1, Daniel Chan1, Jiang Qian2 & Hui Zhang 1 1234567890():,; Inter-tumor heterogeneity is a result of genomic, transcriptional, translational, and post- translational molecular features. To investigate the roles of protein glycosylation in the heterogeneity of high-grade serous ovarian carcinoma (HGSC), we perform mass spectrometry-based glycoproteomic characterization of 119 TCGA HGSC tissues. Cluster analysis of intact glycoproteomic profiles delineates 3 major tumor clusters and 5 groups of intact glycopeptides. It also shows a strong relationship between N-glycan structures and tumor molecular subtypes, one example of which being the association of fucosylation with mesenchymal subtype. Further survival analysis reveals that intact glycopeptide signatures of mesenchymal subtype are associated with a poor clinical outcome of HGSC. In addition, we study the expression of mRNAs, proteins, glycosites, and intact glycopeptides, as well as the expression levels of glycosylation enzymes involved in glycoprotein biosynthesis pathways in each tumor. The results show that glycoprotein levels are mainly controlled by the expression of their individual proteins, and, furthermore, that the glycoprotein-modifying glycans cor- respond to the protein levels of glycosylation enzymes. The variation in glycan types further shows coordination to the tumor heterogeneity. Deeper understanding of the glycosylation process and glycosylation production in different subtypes of HGSC may provide important clues for precision medicine and tumor-targeted therapy. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Global Mapping of Herpesvirus-‐Host Protein Complexes Reveals a Novel Transcription
Global mapping of herpesvirus-host protein complexes reveals a novel transcription strategy for late genes By Zoe Hartman Davis A dissertation submitted in partial satisfaction of the Requirements for the degree of Doctor of Philosophy in Infectious Disease and Immunity in the Graduate Division of the University of California, Berkeley Committee in charge: Professor Britt A. Glaunsinger, Chair Professor Laurent Coscoy Professor Qiang Zhou Spring 2015 Abstract Global mapping of herpesvirus-host protein complexes reveals a novel transcription strategy for late genes By Zoe Hartman Davis Doctor of Philosophy in Infectious Diseases and Immunity University of California, Berkeley Professor Britt A. Glaunsinger, Chair Mapping host-pathogen interactions has proven instrumental for understanding how viruses manipulate host machinery and how numerous cellular processes are regulated. DNA viruses such as herpesviruses have relatively large coding capacity and thus can target an extensive network of cellular proteins. To identify the host proteins hijacked by this pathogen, we systematically affinity tagged and purified all 89 proteins of Kaposi’s sarcoma-associated herpesvirus (KSHV) from human cells. Mass spectrometry of this material identified over 500 high-confidence virus-host interactions. KSHV causes AIDS-associated cancers and its interaction network is enriched for proteins linked to cancer and overlaps with proteins that are also targeted by HIV-1. This work revealed many new interactions between viral and host proteins. I have focused on one interaction in particular, that of a previously uncharacterized KSHV protein, ORF24, with cellular RNA polymerase II (RNAP II). All DNA viruses encode a class of genes that are expressed only late in the infectious cycle, following replication of the viral genome. -

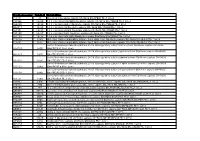
MALE Protein Name Accession Number Molecular Weight CP1 CP2 H1 H2 PDAC1 PDAC2 CP Mean H Mean PDAC Mean T-Test PDAC Vs. H T-Test
MALE t-test t-test Accession Molecular H PDAC PDAC vs. PDAC vs. Protein Name Number Weight CP1 CP2 H1 H2 PDAC1 PDAC2 CP Mean Mean Mean H CP PDAC/H PDAC/CP - 22 kDa protein IPI00219910 22 kDa 7 5 4 8 1 0 6 6 1 0.1126 0.0456 0.1 0.1 - Cold agglutinin FS-1 L-chain (Fragment) IPI00827773 12 kDa 32 39 34 26 53 57 36 30 55 0.0309 0.0388 1.8 1.5 - HRV Fab 027-VL (Fragment) IPI00827643 12 kDa 4 6 0 0 0 0 5 0 0 - 0.0574 - 0.0 - REV25-2 (Fragment) IPI00816794 15 kDa 8 12 5 7 8 9 10 6 8 0.2225 0.3844 1.3 0.8 A1BG Alpha-1B-glycoprotein precursor IPI00022895 54 kDa 115 109 106 112 111 100 112 109 105 0.6497 0.4138 1.0 0.9 A2M Alpha-2-macroglobulin precursor IPI00478003 163 kDa 62 63 86 72 14 18 63 79 16 0.0120 0.0019 0.2 0.3 ABCB1 Multidrug resistance protein 1 IPI00027481 141 kDa 41 46 23 26 52 64 43 25 58 0.0355 0.1660 2.4 1.3 ABHD14B Isoform 1 of Abhydrolase domain-containing proteinIPI00063827 14B 22 kDa 19 15 19 17 15 9 17 18 12 0.2502 0.3306 0.7 0.7 ABP1 Isoform 1 of Amiloride-sensitive amine oxidase [copper-containing]IPI00020982 precursor85 kDa 1 5 8 8 0 0 3 8 0 0.0001 0.2445 0.0 0.0 ACAN aggrecan isoform 2 precursor IPI00027377 250 kDa 38 30 17 28 34 24 34 22 29 0.4877 0.5109 1.3 0.8 ACE Isoform Somatic-1 of Angiotensin-converting enzyme, somaticIPI00437751 isoform precursor150 kDa 48 34 67 56 28 38 41 61 33 0.0600 0.4301 0.5 0.8 ACE2 Isoform 1 of Angiotensin-converting enzyme 2 precursorIPI00465187 92 kDa 11 16 20 30 4 5 13 25 5 0.0557 0.0847 0.2 0.4 ACO1 Cytoplasmic aconitate hydratase IPI00008485 98 kDa 2 2 0 0 0 0 2 0 0 - 0.0081 - 0.0 -
Epigenetic Mechanisms Involved in the Cellular Response to DNA Damage Processed by Base Excision Repair
Epigenetic mechanisms involved in the cellular response to DNA damage processed by Base Excision Repair Thesis submitted in accordance with the requirements of the University of Liverpool for the degree of Doctor in Philosophy by Laura Gail Bennett November 2017 i Abstract Chromatin remodelling is required for access to occluded sequences of DNA by proteins involved in important biological processes, including DNA replication and transcription. There is an increasing amount of evidence for chromatin remodelling during DNA repair, although this has been mostly focused towards DNA double strand break and nucleotide excision repair. At this time there is little evidence for chromatin remodelling in base excision repair (BER). BER is a highly conserved DNA repair pathway which processes spontaneous endogenous DNA base damages generated by oxidative metabolism, but also those induced by exogenous agents (eg. ionising radiation), to maintain genome stability. The mechanism in which the BER repairs damaged bases has been extensively studied and the repair proteins involved are well known. However in terms of chromatin, BER is poorly understood. It is thought that chromatin remodelling occurs due to accumulating evidence indicating that certain BER enzymes are significantly less efficient at acting on sterically occluded sites and near the nucleosome dyad axis. At this time the mechanisms and enzymes involved to facilitate BER are unknown. Therefore, the study presented in this thesis aimed to identify specific histone modification enzymes and/or chromatin remodellers that are involved in the processing of DNA base damage during BER. A method to generate two mononucleosome substrates with a site specific synthetic AP site (tetrahydrofuran; THF) was used to measure recombinant AP endonuclease 1 (APE1) activity alone, and APE1 in HeLa whole cell extract (WCE) that contained chromatin modifiers. -

Supplementary Data Genbank Or OSE Vs RO NIA Accession Gene Name Symbol FC B-Value H3073C09 11.38 5.62 H3126B09 9.64 6.44 H3073B0
Supplementary Data GenBank or OSE vs RO NIA accession Gene name Symbol FC B-value H3073C09 11.38 5.62 H3126B09 9.64 6.44 H3073B08 9.62 5.59 AU022767 Exportin 4 Xpo4 9.62 6.64 H3073B09 9.59 6.48 BG063925 Metallothionein 2 Mt2 9.23 18.89 H3064B07 9.21 6.10 H3073D08 8.28 6.10 AU021923 Jagged 1 Jag1 7.89 5.93 H3070D08 7.54 4.58 BG085110 Cysteine-rich protein 1 (intestinal) Crip1 6.23 16.40 BG063004 Lectin, galactose binding, soluble 1 Lgals1 5.95 10.36 BG069712 5.92 2.34 BG076976 Transcribed locus, strongly similar to NP_032521.1 lectin, galactose binding, soluble 1 5.64 8.36 BG062930 DNA segment, Chr 11, Wayne State University 99, expressed D11Wsu99e 5.63 8.76 BG086474 Insulin-like growth factor binding protein 5 Igfbp5 5.50 15.95 H3002d11 5.13 20.77 BG064706 Keratin complex 1, acidic, gene 19 Krt1-19 5.06 9.07 H3007A09 5.05 2.46 H3065F02 4.84 5.43 BG081752 4.81 1.25 H3010E09 4.71 11.90 H3064c11 4.43 1.00 BG069711 Transmembrane 4 superfamily member 9 Tm4sf9 4.29 1.23 BG077072 Actin, beta, cytoplasmic Actb 4.29 3.01 BG079788 Hemoglobin alpha, adult chain 1 Hba-a1 4.26 6.63 BG076798 4.23 0.80 BG074344 Mesothelin Msln 4.22 6.97 C78835 Actin, beta, cytoplasmic Actb 4.16 3.02 BG067531 4.15 1.61 BG073468 Hemoglobin alpha, adult chain 1 Hba-a1 4.10 6.23 H3154H07 4.08 5.38 AW550167 3.95 5.66 H3121B01 3.94 5.94 H3124f12 3.94 5.64 BG073608 Hemoglobin alpha, adult chain 1 Hba-a1 3.84 5.32 BG073617 Hemoglobin alpha, adult chain 1 Hba-a1 3.84 5.75 BG072574 Hemoglobin alpha, adult chain 1 Hba-a1 3.82 5.93 BG072211 Tumor necrosis factor receptor superfamily, -

Interaction Profiling of RNA-Binding Ubiquitin Ligases Reveals A
www.nature.com/scientificreports OPEN Interaction profling of RNA- binding ubiquitin ligases reveals a link between posttranscriptional Received: 7 March 2017 Accepted: 14 September 2017 regulation and the ubiquitin system Published: xx xx xxxx Andrea Hildebrandt1, Gregorio Alanis-Lobato1,2, Andrea Voigt1, Kathi Zarnack3, Miguel A. Andrade-Navarro1,2, Petra Beli1 & Julian König1 RNA-binding ubiquitin ligases (RBULs) have the potential to link RNA-mediated mechanisms to protein ubiquitylation. Despite this, the cellular functions, substrates and interaction partners of most RBULs remain poorly characterized. Afnity purifcation (AP) combined with quantitative mass spectrometry (MS)-based proteomics is a powerful approach for analyzing protein functions. Mapping the physiological interaction partners of RNA-binding proteins has been hampered by their intrinsic properties, in particular the existence of low-complexity regions, which are prone to engage in non- physiological interactions. Here, we used an adapted AP approach to identify the interaction partners of human RBULs harboring diferent RNA-binding domains. To increase the likelihood of recovering physiological interactions, we combined control and bait-expressing cells prior to lysis. In this setup, only stable interactions that were originally present in the cell will be identifed. We exploit gene function similarity between the bait proteins and their interactors to benchmark our approach in its ability to recover physiological interactions. We reveal that RBULs engage in stable interactions with RNA-binding proteins involved in diferent steps of RNA metabolism as well as with components of the ubiquitin conjugation machinery and ubiquitin-binding proteins. Our results thus demonstrate their capacity to link posttranscriptional regulation with the ubiquitin system. -

Alpa Sidhu , Justin R. Miller , Ashootosh Tripathi , Danielle M. Garshott , Amy L. Brownell , Daniel J. Chiego , Carl Arevang
Alpa Sidhu€‡, Justin R. Miller€‡, Ashootosh Tripathi¶, Danielle M. Garshott€, Amy L. Brownell€, Daniel J. Chiego∑, Carl Arevang¶, Qinghua Zeng€, Leah C. Jackson€, Shelby A. Bechler€, Michael U. Calla- ghan€, George H. YooÖ, Seema Sethiñ, Ho-Sheng LinÖ, Joseph H. Callaghan§, Giselle Tamayo- CastilloØ, David H. Sherman¶, *, Randal J. KaufmanΩ, * and Andrew M. Fribley€,Ö, ≠,* € Carmen and Ann Adams Department of Pediatrics, Wayne State University School of Medicine, Detroit, MI 48201 ¶ Life Sciences Institute and Departments of Medicinal Chemistry, Chemistry, Microbiology & Immunology, University of Michigan, Ann Arbor, MI 48109 ∑ Cariology, Restorative Sciences and Endodontics, University of Michigan School of Dentistry, Ann Arbor, MI 48109 Ö Department of Otolaryngology, Wayne State University and Karmanos Cancer Institute, Detroit, MI 48201 ñ Department of Pathology, Wayne State University and Karmanos Cancer Institute, Detroit, MI 48201 § School of Business Administration, Oakland University, Rochester, MI 48309 ØInstituto Nacional de Biodiversidad, 3100-Heredia, CIPRONA-Escuela de Química, Universidad de Costa Rica Ω Degenerative Disease Research Program, Center for Cancer Research, Sanford|Burnham Medical Research Institute, La Jolla, CA 92037 ≠ Developmental Therapeutics Program, Barbara Ann Karmanos Cancer Institute, Detroit, MI 48201 ‡ These authors contributed equally Contents: Page: Experimental Procedures 2 - 3 Figure S1. SEM RT-qPCR, Leukemia proliferation, and Leukemia Casp3/7-glo 4 Table S1. UPR Gene Array. 5-7 Table S2. DNA Damage Gene Array. 8-10 Table S3. Apoptosis Gene Array. 11-13 Figure S2. Comparison of two borrelidin samples purchased from Sigma. 14 Figure S3. RT-qPCR analysis of OSCC cell lines reveals expression of cell UPR genes in 15 response to borrelidin. -

Downregulation of Carnitine Acyl-Carnitine Translocase by Mirnas
Page 1 of 288 Diabetes 1 Downregulation of Carnitine acyl-carnitine translocase by miRNAs 132 and 212 amplifies glucose-stimulated insulin secretion Mufaddal S. Soni1, Mary E. Rabaglia1, Sushant Bhatnagar1, Jin Shang2, Olga Ilkayeva3, Randall Mynatt4, Yun-Ping Zhou2, Eric E. Schadt6, Nancy A.Thornberry2, Deborah M. Muoio5, Mark P. Keller1 and Alan D. Attie1 From the 1Department of Biochemistry, University of Wisconsin, Madison, Wisconsin; 2Department of Metabolic Disorders-Diabetes, Merck Research Laboratories, Rahway, New Jersey; 3Sarah W. Stedman Nutrition and Metabolism Center, Duke Institute of Molecular Physiology, 5Departments of Medicine and Pharmacology and Cancer Biology, Durham, North Carolina. 4Pennington Biomedical Research Center, Louisiana State University system, Baton Rouge, Louisiana; 6Institute for Genomics and Multiscale Biology, Mount Sinai School of Medicine, New York, New York. Corresponding author Alan D. Attie, 543A Biochemistry Addition, 433 Babcock Drive, Department of Biochemistry, University of Wisconsin-Madison, Madison, Wisconsin, (608) 262-1372 (Ph), (608) 263-9608 (fax), [email protected]. Running Title: Fatty acyl-carnitines enhance insulin secretion Abstract word count: 163 Main text Word count: 3960 Number of tables: 0 Number of figures: 5 Diabetes Publish Ahead of Print, published online June 26, 2014 Diabetes Page 2 of 288 2 ABSTRACT We previously demonstrated that micro-RNAs 132 and 212 are differentially upregulated in response to obesity in two mouse strains that differ in their susceptibility to obesity-induced diabetes. Here we show the overexpression of micro-RNAs 132 and 212 enhances insulin secretion (IS) in response to glucose and other secretagogues including non-fuel stimuli. We determined that carnitine acyl-carnitine translocase (CACT, Slc25a20) is a direct target of these miRNAs. -

Supplementary Materials (PDF)
Proteomics of the mediodorsal thalamic nucleus in gastric ulcer induced by restraint-water-immersion-stress Sheng-Nan Gong, Jian-Ping Zhu, Ying-Jie Ma, Dong-Qin Zhao Table S1. The entire list of 2,853 proteins identified between the control and stressed groups Protein NO Protein name Gene name Accession No LogRatio 1 Tubulin alpha-1A chain Tuba1a TBA1A_RAT 0.2320 2 Spectrin alpha chain, non-erythrocytic 1 Sptan1 A0A0G2JZ69_RAT -0.0291 3 ATP synthase subunit alpha, mitochondrial Atp5f1a ATPA_RAT -0.1155 4 Tubulin beta-2B chain Tubb2b TBB2B_RAT 0.0072 5 Actin, cytoplasmic 2 Actg1 ACTG_RAT 0.0001 Sodium/potassium-transporting ATPase Atp1a2 6 subunit alpha-2 AT1A2_RAT -0.0716 7 Spectrin beta chain Sptbn1 A0A0G2K8W9_RAT -0.1158 8 Clathrin heavy chain 1 Cltc CLH1_RAT 0.0788 9 Dihydropyrimidinase-related protein 2 Dpysl2 DPYL2_RAT -0.0696 10 Glyceraldehyde-3-phosphate dehydrogenase Gapdh G3P_RAT -0.0687 Sodium/potassium-transporting ATPase Atp1a3 11 subunit alpha-3 AT1A3_RAT 0.0391 12 ATP synthase subunit beta, mitochondrial Atp5f1b ATPB_RAT 0.1772 13 Cytoplasmic dynein 1 heavy chain 1 Dync1h1 M0R9X8_RAT 0.0527 14 Myelin basic protein transcript variant N Mbp I7EFB0_RAT 0.0696 15 Microtubule-associated protein Map2 F1LNK0_RAT -0.1053 16 Pyruvate kinase PKM Pkm KPYM_RAT -0.2608 17 D3ZQQ5_RAT 0.0087 18 Plectin Plec F7F9U6_RAT -0.0076 19 14-3-3 protein zeta/delta Ywhaz A0A0G2JV65_RAT -0.2431 20 2',3'-cyclic-nucleotide 3'-phosphodiesterase Cnp CN37_RAT -0.0495 21 Creatine kinase B-type Ckb KCRB_RAT -0.0514 Voltage-dependent anion-selective channel -

GANAB Antibody Cat
GANAB Antibody Cat. No.: 15-233 GANAB Antibody Immunohistochemistry of paraffin-embedded Immunohistochemistry of paraffin-embedded mouse brain using rat brain using GANAB antibody (15-233) at GANAB antibody (15-233) at dilution of 1:150 (40x lens). dilution of 1:150 (40x lens). Immunofluorescence analysis of C6 cells using Immunofluorescence analysis of NIH-3T3 cells using GANAB GANAB antibody (15-233) at dilution of 1:100. antibody (15-233) at dilution of 1:100. Blue: DAPI for nuclear Blue: DAPI for nuclear staining. staining. September 29, 2021 1 https://www.prosci-inc.com/ganab-antibody-15-233.html Immunofluorescence analysis of U-2 OS cells Immunofluorescence analysis of C6 cells using GANAB antibody using GANAB antibody (15-233) at dilution of (15-233) at dilution of 1:100. Blue: DAPI for nuclear staining. 1:100. Blue: DAPI for nuclear staining. Immunofluorescence analysis of NIH-3T3 cells using GANAB antibody (15-233) at dilution of 1:100. Blue: DAPI for nuclear staining. Specifications HOST SPECIES: Rabbit SPECIES REACTIVITY: Human, Mouse, Rat Recombinant fusion protein containing a sequence corresponding to amino acids 1-260 of IMMUNOGEN: human GANAB (NP_001265123.1). TESTED APPLICATIONS: IF, IHC, WB WB: ,1:500 - 1:2000 APPLICATIONS: IHC: ,1:50 - 1:200 IF: ,1:50 - 1:200 POSITIVE CONTROL: 1) U-87MG 2) Raji 3) HepG2 4) HeLa 5) Mouse brain 6) Mouse liver PREDICTED MOLECULAR Observed: 112kDa WEIGHT: September 29, 2021 2 https://www.prosci-inc.com/ganab-antibody-15-233.html Properties PURIFICATION: Affinity purification CLONALITY: Polyclonal ISOTYPE: IgG CONJUGATE: Unconjugated PHYSICAL STATE: Liquid BUFFER: PBS with 0.02% sodium azide, 50% glycerol, pH7.3. -
Protein List
Protein Accession Protein Id Protein Name P11171 41 Protein 4.