Phytochemical-Constituents, Safety and Efficacy of Commonly Used Medicinal Plants for the Treatment of Malaria in Ethiopia-A Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Honey Bee Suite © Rusty Burlew 2015 Master Plant List by Scientific Name United States
Honey Bee Suite Master Plant List by Scientific Name United States © Rusty Burlew 2015 Scientific name Common Name Type of plant Zone Full Link for more information Abelia grandiflora Glossy abelia Shrub 6-9 http://plants.ces.ncsu.edu/plants/all/abelia-x-grandiflora/ Acacia Acacia Thorntree Tree 3-8 http://www.2020site.org/trees/acacia.html Acer circinatum Vine maple Tree 7-8 http://www.nwplants.com/business/catalog/ace_cir.html Acer macrophyllum Bigleaf maple Tree 5-9 http://treesandshrubs.about.com/od/commontrees/p/Big-Leaf-Maple-Acer-macrophyllum.htm Acer negundo L. Box elder Tree 2-10 http://www.missouribotanicalgarden.org/PlantFinder/PlantFinderDetails.aspx?kempercode=a841 Acer rubrum Red maple Tree 3-9 http://www.missouribotanicalgarden.org/PlantFinder/PlantFinderDetails.aspx?taxonid=275374&isprofile=1&basic=Acer%20rubrum Acer rubrum Swamp maple Tree 3-9 http://www.missouribotanicalgarden.org/PlantFinder/PlantFinderDetails.aspx?taxonid=275374&isprofile=1&basic=Acer%20rubrum Acer saccharinum Silver maple Tree 3-9 http://en.wikipedia.org/wiki/Acer_saccharinum Acer spp. Maple Tree 3-8 http://en.wikipedia.org/wiki/Maple Achillea millefolium Yarrow Perennial 3-9 http://www.missouribotanicalgarden.org/PlantFinder/PlantFinderDetails.aspx?kempercode=b282 Aesclepias tuberosa Butterfly weed Perennial 3-9 http://www.missouribotanicalgarden.org/PlantFinder/PlantFinderDetails.aspx?kempercode=b490 Aesculus glabra Buckeye Tree 3-7 http://www.missouribotanicalgarden.org/PlantFinder/PlantFinderDetails.aspx?taxonid=281045&isprofile=1&basic=buckeye -
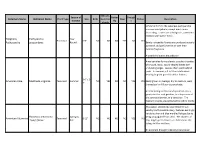
Common Name Botanical Name Alleghany
Attracts Season of Butter Drough Common Name Botanical Name Plant Type Size Birds Hummin Deer Native Description Interest fly t g birds Similar in form to the Japanese pachysandra one sees everywhere, except much more interesting. Leaves are a dull green, sometimes mottled with lighter flecks. Alleghany Pachysandra Year Perennial 6-8" NO NO NO YES NO YES Pachysandra procumbens Round Barely noticeable flowers are produced as early as March and perfume the air with their delicate fragrance. A wonderful native groundcover. American aloe forms a lovely succulent rosette of smooth, waxy, sword-shaped leaves with undulating edges. Leaves often sport reddish spots. In summer, a 3 to 5 foot stalk arises bearing fragrant greenish-white flowers. 3-6' x 2- American Aloe Manfreda virginica Perennial Summer NO YES NO NO YES YES Easily grown in average, dry to medium, well- 3' drained soil in full sun to part shade. An interesting architectural specimen, it is a good plant for rock gardens, in a dry corner of the perennial border, or a container. The fragrant blooms are pollinated by sphinx moths. This native, selected by Dale Hendrick's at nearby North Creek Nursery, features excitingly variable silver and blue marbled foliage due to Heuchera americana Spring to being propagated from seed. The clusters of American Alumroot Perennial 8-12" NO NO NO NO YES NO 'Dale's Strain' Fall tiny, bright green flowers are held above the foliage in May and June. An excellent drought tolerant groundcover. Viburnum trilobum is a native deciduous shrub to the northeastern and northwestern United States. -

Medical Ethnobotany of the Albanian Alps in Kosovo
Medical ethnobotany of the Albanian Alps in Kosovo Behxhet Mustafa, University of Prishtina Avni Hajdari, University of Prishtina Feriz Krasniqi, Kosovo Academy of Sciences and Arts Esat Hoxha, University of Prishtina Hatixhe Ademi, University of Prishtina Cassandra Quave, Emory University Andrea Pieroni, Univ Gastron Sci Journal Title: Journal of Ethnobiology and Ethnomedicine Volume: Volume 8 Publisher: BioMed Central | 2012-01-28, Pages 6-6 Type of Work: Article | Final Publisher PDF Publisher DOI: 10.1186/1746-4269-8-6 Permanent URL: https://pid.emory.edu/ark:/25593/rnh2w Final published version: http://dx.doi.org/10.1186/1746-4269-8-6 Copyright information: © 2012 Mustafa et al; licensee BioMed Central Ltd. Accessed September 26, 2021 3:06 AM EDT Mustafa et al. Journal of Ethnobiology and Ethnomedicine 2012, 8:6 http://www.ethnobiomed.com/content/8/1/6 JOURNAL OF ETHNOBIOLOGY AND ETHNOMEDICINE RESEARCH Open Access Medical ethnobotany of the Albanian Alps in Kosovo Behxhet Mustafa1, Avni Hajdari1*, Feriz Krasniqi2, Esat Hoxha1, Hatixhe Ademi1, Cassandra L Quave3 and Andrea Pieroni4 Abstract Background: Ethnobotanical studies are crucial in South-Eastern Europe for fostering local development and also for investigating the dynamics of Traditional Environmental Knowledge (TEK) related to plants in one of the most crucial European hotspots for biocultural diversity. The current medico-ethnobotanical survey was conducted in rural alpine communities in Kosovo. The aims of the study were twofold: 1) to document the state of TEK of medicinal plants in these communities; 2) to compare these findings with that of similar field studies previously conducted among local populations inhabiting the Montenegrin and Albanian side of the same Alpine range. -
Field Grown Cut Flowers
Nursery FACTSHEET September 2015 Field Grown Cut Flowers INTRODUCTION The culture of field grown flowers is an area of floriculture that is generating a lot of interest and is enjoying a steady growth rate. It provides a way to enter the floriculture industry without the $100 to $150 per square metre capital costs that are involved in some greenhouse crops. Recently, the largest area of growth has been in the specialty cut flowers as opposed to the more traditional field grown crops like statice, dahlias and gypsophila. As gardening increases in popularity, home consumers are becoming familiar with the many new and different flower species. In turn, consumers are starting to look for and demand these flowers in floral design work. Site Selection Whether you plan to lease or own the land, there are basic, yet important, site considerations (see Table 1). It is easier if you start with a suitable site rather than try to modify it later. Table 1. Considerations when selecting a production site Soil: It should be fertile and well drained. Soil tests are a basic management tool. Even if you are familiar with the soil in the area, it must be tested to determine pH, organic matter and nutrient levels. A pH of 6.0–6.5 is suitable for most cuts. Know the requirements of your crop before you make any major changes. Water: Good quality water must be available in sufficient quantities. Have the water source tested to determine essentials like pH and EC (salinity). Terrain: Flat land is easier to work. Watch out for low lying pockets that might be prone to early and late frosts, or flooding during the wet months. -
Fragrant Annuals Fragrant Annuals
TheThe AmericanAmerican GARDENERGARDENER® TheThe MagazineMagazine ofof thethe AAmericanmerican HorticulturalHorticultural SocietySociety JanuaryJanuary // FebruaryFebruary 20112011 New Plants for 2011 Unusual Trees with Garden Potential The AHS’s River Farm: A Center of Horticulture Fragrant Annuals Legacies assume many forms hether making estate plans, considering W year-end giving, honoring a loved one or planting a tree, the legacies of tomorrow are created today. Please remember the American Horticultural Society when making your estate and charitable giving plans. Together we can leave a legacy of a greener, healthier, more beautiful America. For more information on including the AHS in your estate planning and charitable giving, or to make a gift to honor or remember a loved one, please contact Courtney Capstack at (703) 768-5700 ext. 127. Making America a Nation of Gardeners, a Land of Gardens contents Volume 90, Number 1 . January / February 2011 FEATURES DEPARTMENTS 5 NOTES FROM RIVER FARM 6 MEMBERS’ FORUM 8 NEWS FROM THE AHS 2011 Seed Exchange catalog online for AHS members, new AHS Travel Study Program destinations, AHS forms partnership with Northeast garden symposium, registration open for 10th annual America in Bloom Contest, 2011 EPCOT International Flower & Garden Festival, Colonial Williamsburg Garden Symposium, TGOA-MGCA garden photography competition opens. 40 GARDEN SOLUTIONS Plant expert Scott Aker offers a holistic approach to solving common problems. 42 HOMEGROWN HARVEST page 28 Easy-to-grow parsley. 44 GARDENER’S NOTEBOOK Enlightened ways to NEW PLANTS FOR 2011 BY JANE BERGER 12 control powdery mildew, Edible, compact, upright, and colorful are the themes of this beating bugs with plant year’s new plant introductions. -

Phylogeny and Phylogenetic Nomenclature of the Campanulidae Based on an Expanded Sample of Genes and Taxa
Systematic Botany (2010), 35(2): pp. 425–441 © Copyright 2010 by the American Society of Plant Taxonomists Phylogeny and Phylogenetic Nomenclature of the Campanulidae based on an Expanded Sample of Genes and Taxa David C. Tank 1,2,3 and Michael J. Donoghue 1 1 Peabody Museum of Natural History & Department of Ecology & Evolutionary Biology, Yale University, P. O. Box 208106, New Haven, Connecticut 06520 U. S. A. 2 Department of Forest Resources & Stillinger Herbarium, College of Natural Resources, University of Idaho, P. O. Box 441133, Moscow, Idaho 83844-1133 U. S. A. 3 Author for correspondence ( [email protected] ) Communicating Editor: Javier Francisco-Ortega Abstract— Previous attempts to resolve relationships among the primary lineages of Campanulidae (e.g. Apiales, Asterales, Dipsacales) have mostly been unconvincing, and the placement of a number of smaller groups (e.g. Bruniaceae, Columelliaceae, Escalloniaceae) remains uncertain. Here we build on a recent analysis of an incomplete data set that was assembled from the literature for a set of 50 campanulid taxa. To this data set we first added newly generated DNA sequence data for the same set of genes and taxa. Second, we sequenced three additional cpDNA coding regions (ca. 8,000 bp) for the same set of 50 campanulid taxa. Finally, we assembled the most comprehensive sample of cam- panulid diversity to date, including ca. 17,000 bp of cpDNA for 122 campanulid taxa and five outgroups. Simply filling in missing data in the 50-taxon data set (rendering it 94% complete) resulted in a topology that was similar to earlier studies, but with little additional resolution or confidence. -

False Flowers in Asteraceae
Available online at www.sciencedirect.com ScienceDirect Don’t be fooled: false flowers in Asteraceae Teng Zhang and Paula Elomaa The sunflower or daisy family, Asteraceae, comprises of meristems represent so-called flower unit meristems approximately 10% of all angiosperm species. Their (FUM) (Box 1) [4 ]. inflorescences form dense flower-like structures, pseudanthia or false flowers that may combine hundreds of individual In this review, we aim to highlight the most recent work flowers into a single structure. Recent data suggest that to understand the organization, patterning and develop- pseudanthia are analogs of single flowers not only ment of this unique structure and its role for adaptation. morphologically but also at developmental and genetic level, Because of still very limited number of molecular studies, and cannot merely be considered as condensed we also refer to selected older research addressing inflorescences. The large meristem size provides an advantage the major biological questions. Many of the floral traits to study basic principles of patterning as well as inflorescence in Asteraceae are of practical relevance for breeding of diversity in this evolutionary successful family. This knowledge commercially important crops within the family, includ- has also practical importance in the commercially important ing edible leaf, stem and seed oil crops (lettuce, artichoke, crops of the family. endive, sunflower, safflower), herbs and medicinal plants (Artemisia, Calendula, Echinaceae), as well as ornamental Address cut flowers (gerbera, chrysanthemum) [5]. Department of Agricultural Sciences, Viikki Plant Science Centre, 00014 University of Helsinki, Finland Origin and diversity of capitula in Asteraceae Corresponding author: Elomaa, Paula (paula.elomaa@helsinki.fi) Within flowering plants, Asteraceae belongs to the well- supported MGCA clade consisting of families of Menyanthaceae, Goodeniaceae, Calyceraceae, and Astera- Current Opinion in Plant Biology 2021, 59:101972 ceae (Figure 1). -

Medical Ethnobotany of the Albanian Alps in Kosovo
Mustafa et al. Journal of Ethnobiology and Ethnomedicine 2012, 8:6 http://www.ethnobiomed.com/content/8/1/6 JOURNAL OF ETHNOBIOLOGY AND ETHNOMEDICINE RESEARCH Open Access Medical ethnobotany of the Albanian Alps in Kosovo Behxhet Mustafa1, Avni Hajdari1*, Feriz Krasniqi2, Esat Hoxha1, Hatixhe Ademi1, Cassandra L Quave3 and Andrea Pieroni4 Abstract Background: Ethnobotanical studies are crucial in South-Eastern Europe for fostering local development and also for investigating the dynamics of Traditional Environmental Knowledge (TEK) related to plants in one of the most crucial European hotspots for biocultural diversity. The current medico-ethnobotanical survey was conducted in rural alpine communities in Kosovo. The aims of the study were twofold: 1) to document the state of TEK of medicinal plants in these communities; 2) to compare these findings with that of similar field studies previously conducted among local populations inhabiting the Montenegrin and Albanian side of the same Alpine range. Methods: Field research was conducted in 36 villages on the Kosovar side of the Albanian Alps. Snowball sampling techniques were used to recruit 91 elderly informants (≥ 50 years-old) for participation in semi-structured interviews and structured surveys regarding the use of the local flora for medicinal and food purposes. Standard ethnobotanical methods were employed and prior informed consent was obtained for all study participants. Results and Conclusion: The uses of 98 plants species belonging to 39 families were recorded; the most quoted botanical families were Rosaceae, Asteraceae, and Lamiaceae. Mainly decoctions and infusions were quoted as folk medicinal preparations and the most common uses referred to gastrointestinal and respiratory disorders, as well as illnesses of the uro-genital system. -

Kugeldisteln Aus Wikipedia, Der Freien Enzyklopädie
Kugeldisteln aus Wikipedia, der freien Enzyklopädie Die Kugeldisteln (Echinops) sind eine Pflanzengattung aus der Familie der Korbblütler (Asteraceae). Kugeldisteln Inhaltsverzeichnis 1 Merkmale 2 Verbreitung 3 Systematik 4 Etymologie 5 Belege 5.1 Einzelnachweise 6 Weblinks Drüsenblättrige Kugeldistel (Echinops sphaerocephalus), Merkmale Blütenstand Systematik Die Kugeldisteln sind ausdauernde krautige Pflanzen, die als Überdauerungsorgane Rhizome ausbilden. Die Stängel Euasteriden II stehen aufrecht und sind kantig. Die wechselständig Ordnung: Asternartige (Asterales) stehenden Laubblätter sind ein- bis zweifach fiederteilig und Familie: Korbblütler (Asteraceae) unterseits weiß-wollig-filzig. Unterfamilie: Carduoideae Tribus: Cynareae Die Köpfchen sind einblütig, besitzen eine zwittrige Röhrenblüte und sind von einer mehrreihigen Hülle Gattung: Kugeldisteln umgeben. Zahlreiche Körbchen bilden kugelförmige Wissenschaftlicher Name Blütenstände zweiter Ordnung, die Durchmesser von 4 bis 8 Echinops Zentimeter aufweisen. Die Körbchen blühen innerhalb eines L. Kopfes von oben nach unten auf. Die Blütenkrone ist röhrig, dabei fast bis zum Grund geteilt. Die Blütenfarbe ist stahlblau bis weiß, die Blütenstände als Ganzes sind meist bläulich. Die Staubblätter sind blaugrau. Die Achänenfrüchte sind zylindrisch, fünfkantig und anliegend behaart. Der Pappus ist kurzschuppig. Verbreitung Die Kugeldisteln kommen in Eurasien und Afrika vor.[1] Systematik Die Kugeldisteln werden innerhalb der Unterfamilie Carduoideae in die Tribus Cardueae und Subtribus -

An Inventory of Vascular Plants Identified on the Sefton Coast
1 An inventory of vascular plants identified on the Sefton Coast Philip H. Smith November 2005 Unpublished report to Sefton Coast Partnership Introduction & Methods Five years ago, a provisional inventory of vascular plants (species, sub-species and hybrids) identified on the Sefton Coast, Merseyside, was drawn up (Smith 1999a). It listed a total of 971 taxa within the Sefton Coast Management Scheme (now Sefton Coast Partnership) area, of which 881 (90.7%) were recorded in the sand-dune system and 733 (75.5%) in the candidate Special Area of Conservation (cSAC). Some 290 taxa (29.9%) were thought to be non-native to the area and only 14 (1.4%) were considered extinct. Intensive field-work in recent years (and especially in 2004 and 2005) for the proposed new Flora of South Lancashire (vice-county 59) has resulted in a large number of new records, including many garden-escapes, and it was therefore felt appropriate to produce an up-to-date inventory on similar lines to the earlier one. However, since the boundaries of the cSAC have recently been redrawn to include most of the dune system, including dune-heath areas previously excluded, it was decided not to produce a separate list for the cSAC. In addition to sources utilised in the provisional inventory (e.g. Savidge et al. 1963, the 1988 Sefton Coast N.V.C. survey, Ainsdale Sand Dunes and Cabin Hill NNR vascular plant lists, the New Atlas survey data and the Environmental Advisory Service data-base) much use has been made of the v.c. 59 tetrad records currently stored on CD, which forms part of the forthcoming new Flora of South Lancashire. -

The Geography of Gardening the Geography of Gardening
TheThe AmericanAmerican GARDENERGARDENER® TheThe MagazineMagazine ofof thethe AmericanAmerican HorticulturalHorticultural SocietySociety JanuaryJanuary // FebruaryFebruary 20122012 the Geography of Gardening New Plants for 2012 Alluring Jasmines Garden Edging contents Volume 91, Number 1 . January / February 2012 FEATURES DEPARTMENTS 5 NOTES FROM RIVER FARM 6 MEMBERS’ FORUM 8 NEWS FROM THE AHS American Horticultural Society celebrates 90th anniversary, grant awarded to the AHS to fund digital archive of AHS periodicals, 2012 seed exchange catalog available for members, East Coast spring gardening symposiums, new member password for AHS website, register your community for 2012 America in Bloom competition. 12 AHS MEMBERS MAKING A DIFFERENCE Samuel Salsbury and Sabrena Schweyer. 36 GARDEN SOLUTIONS Preventive pruning for woody plants. 38 HOMEGROWN HARVEST Gourmet shallots. page 14 40 GARDENER’S NOTEBOOK Research finds fungi and plant roots negotiate for scarce resources, sterile NEW FOR 2012 BY MARY YEE 14 burning bush developed, night-blooming Here’s a look at some of the new plants that will be available this orchid discovered, grant supports manual to spring, with recommended varieties from regional gardening assist American Chestnut Foundation, new experts who have successfully grown them. network to study effects of climate change on plants, legacy of Frank Cabot. ® 20 MAINTAINING AN EDGE BY RITA PELCZAR Green Garage : Selected useful garden tools and products. Edgings physically separate and define spaces in the landscape and can contribute significant style to a garden. 45 TRAVELER’S GUIDE TO GARDENS *NEW* Indianapolis Museum of Art. 24 ALLURING JASMINES BY RAND B. LEE 46 BOOK REVIEWS Dirr’s Encyclopedia of Trees and Shrubs, Beloved by poets, perfumers, and gar- Designing with Conifers, and One Writer’s deners, jasmines bring mystery and Garden. -
Latin for Gardeners: Over 3,000 Plant Names Explained and Explored
L ATIN for GARDENERS ACANTHUS bear’s breeches Lorraine Harrison is the author of several books, including Inspiring Sussex Gardeners, The Shaker Book of the Garden, How to Read Gardens, and A Potted History of Vegetables: A Kitchen Cornucopia. The University of Chicago Press, Chicago 60637 © 2012 Quid Publishing Conceived, designed and produced by Quid Publishing Level 4, Sheridan House 114 Western Road Hove BN3 1DD England Designed by Lindsey Johns All rights reserved. Published 2012. Printed in China 22 21 20 19 18 17 16 15 14 13 1 2 3 4 5 ISBN-13: 978-0-226-00919-3 (cloth) ISBN-13: 978-0-226-00922-3 (e-book) Library of Congress Cataloging-in-Publication Data Harrison, Lorraine. Latin for gardeners : over 3,000 plant names explained and explored / Lorraine Harrison. pages ; cm ISBN 978-0-226-00919-3 (cloth : alkaline paper) — ISBN (invalid) 978-0-226-00922-3 (e-book) 1. Latin language—Etymology—Names—Dictionaries. 2. Latin language—Technical Latin—Dictionaries. 3. Plants—Nomenclature—Dictionaries—Latin. 4. Plants—History. I. Title. PA2387.H37 2012 580.1’4—dc23 2012020837 ∞ This paper meets the requirements of ANSI/NISO Z39.48-1992 (Permanence of Paper). L ATIN for GARDENERS Over 3,000 Plant Names Explained and Explored LORRAINE HARRISON The University of Chicago Press Contents Preface 6 How to Use This Book 8 A Short History of Botanical Latin 9 Jasminum, Botanical Latin for Beginners 10 jasmine (p. 116) An Introduction to the A–Z Listings 13 THE A-Z LISTINGS OF LatIN PlaNT NAMES A from a- to azureus 14 B from babylonicus to byzantinus 37 C from cacaliifolius to cytisoides 45 D from dactyliferus to dyerianum 69 E from e- to eyriesii 79 F from fabaceus to futilis 85 G from gaditanus to gymnocarpus 94 H from haastii to hystrix 102 I from ibericus to ixocarpus 109 J from jacobaeus to juvenilis 115 K from kamtschaticus to kurdicus 117 L from labiatus to lysimachioides 118 Tropaeolum majus, M from macedonicus to myrtifolius 129 nasturtium (p.