Ten More Years of CPAP: Tribulations and Trials
Total Page:16
File Type:pdf, Size:1020Kb
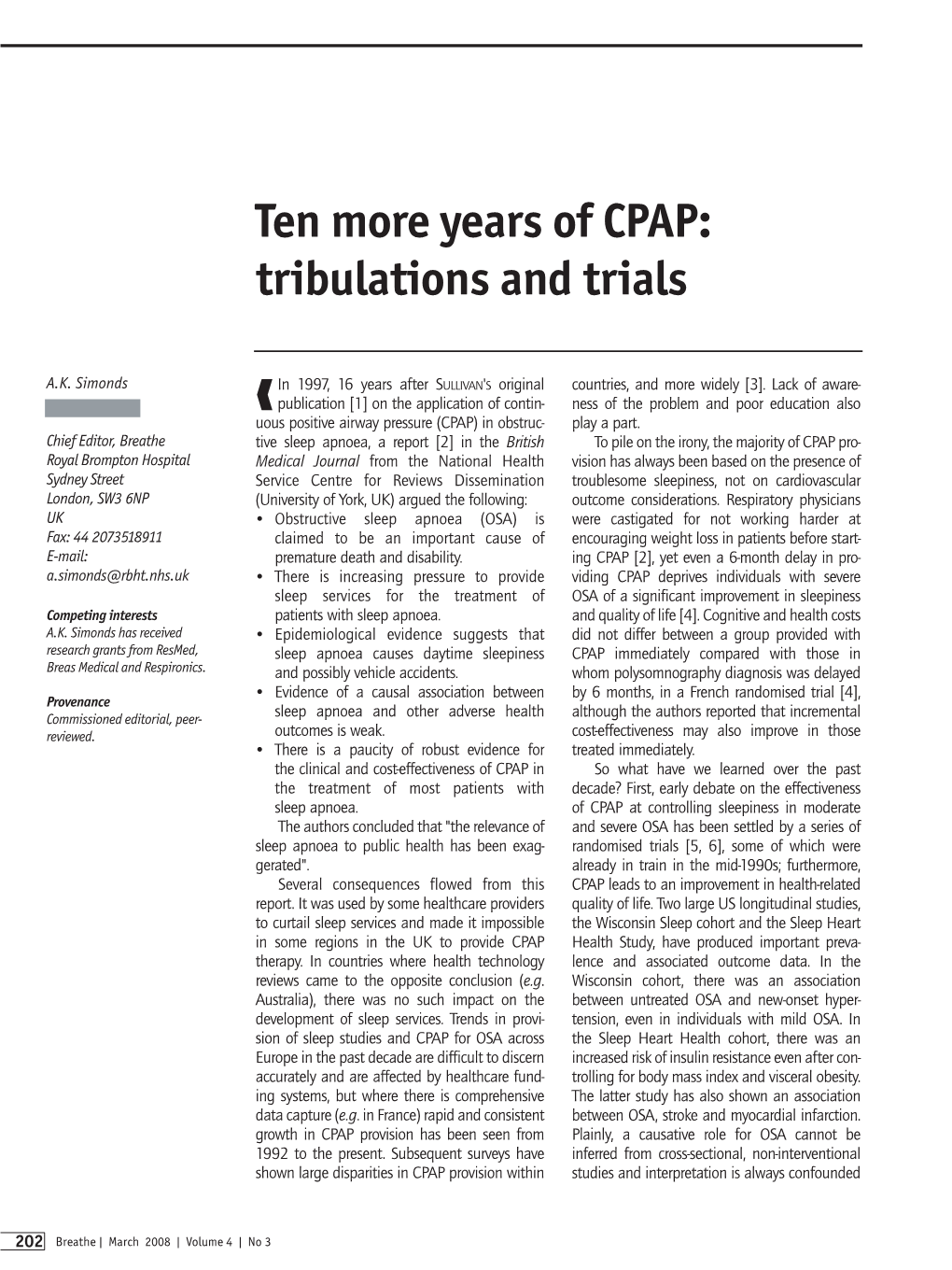
Load more
Recommended publications
-

Sleep and Its Disorders: Is the Problem
38 ISSN 0049-6804. «Врачеб. дело». 2017, № 1–2 ОБЗОР ЛИТЕРАТУРЫ 43. Williams G. R., Duncan Bassett J. H. Local control of thyroid hormone action: role of type 2 deiodinase Deiodinases: the balance of thyroid hormone // J. of Endocrinol. – 2011. – Vol. 209. – P. 261–272. 44. Wittmann G., Harney J. W., Singru P. S. et al. Inflammation-inducible type 2 deiodinase expres- sion in the leptomeninges, choroid plexus, and at brain blood vessels in male rodents // Endocri- nology. – 2014. – Vol. 155. – P. 2009–2019. 45. Yu J., Koenig R. J. Induction of type 1 iodothyronine deiodinase to prevent the nonthyroidal illness syndrome in mice // Endocrinol. – 2006. – Vol. 147, N 7. – Р. 3580–3585. СУЧАСНІ УЯВЛЕННЯ ПРО СИНДРОМ НЕТИРЕОЇДНОЇ ПАТОЛОГІЇ В КЛІНІЧНІЙ ПРАКТИЦІ Н. О. Абрамова, Н. В. Пашковська (Чернівці) Будь-які гострі та хронічні захворювання, що втягують у патологічний процес весь організм, можуть викликати порушення обміну тиреоїдних гормонів на фоні відсутності супутньої патології щитоподібної залози, гіпофіза та (або) гіпоталамуса. Такі порушення називають «син- дромом нетиреоїдної патології» (СНТП), або «синдромом низького Т3», і зустрічаються у 70 % госпіталізованих. У даному огляді ми розглянули етіологію, патогенез та частково шляхи корекції синдрому нетиреоїдної патології. Ключові слова: синдром нетиреоїдної патології, синдром низького Т3, порушення обміну тиреоїдних гормонів. CURRENT VIEWS ON NONTHYROIDAL ILLNESS SYNDROME IN CLINICAL PRACTICE (REVIEW) N. O. Abramova, N. V. Pashkovska (Chernivtsi, Ukraine) Higher State Educational Establishment of Ukraine «Bukovinian State Medical University» Any acute and chronic diseases that involve the whole organism into pathological process, can cause violation of thyroid hormones metabolism against a background of absence of concomitant diseases of thyroid gland, pituitary gland or hypothalamus. -

Sleepiness the Wheel
SLEEPINESS AT THE WHEEL WHITE PAPER SLEEPINESS AT THE WHEEL WHITE PAPER Sleepiness at the Wheel WHITE PAPER PREFACE Improving road safety is a priority of the French Government. Among the various causes of road accidents, one of them is especially common on motorways: lack of alertness, which leads to inattention and sleepiness. Lack of alertness is responsible for one in three collisions resulting in deaths on the motorway network, although it is the safest of all road networks! This phenomenon is not fully grasped by the public. Therefore, it is essential to gain knowledge and raise the publics’ awareness as regards sleepiness at the wheel. In more general terms, sleepiness at the wheel remains underestimated both socially and culturally speaking, which is a major issue for road safety and public health. This white book, put together by the French Motorway Companies (ASFA) and the National Institute of Sleep and Vigilance (INSV), presents the most recent knowledge on the subject at both the French and European levels and provides a number of recommendations. By contributing to a better understanding of sleepiness at the wheel, this work will help promote the implementation of new prevention strategies, to further reduce the number of victims on the road. Our objective is to cut down to less than 2000 the number of deaths per year on French roads by 2020. Manuel VALLS French Minister of Interior ASFA and INSV would like to express their deep thanks to the panel of European sleep experts who author this book. Most of them also participate in the research on traffic accidents associated with sleepiness in their own country and thus have contributed to enrich our knowledge and proposals for preventing from the consequences of sleepiness at the wheel. -
Polymorphism Located in TCRA Locus Confers Susceptibility to Essential Hypersomnia with HLA-DRB1&Ast;1501-DQB1&Ast;0602
Journal of Human Genetics (2010) 55, 63–65 & 2010 The Japan Society of Human Genetics All rights reserved 1434-5161/10 $32.00 www.nature.com/jhg SHORT COMMUNICATION Polymorphism located in TCRA locus confers susceptibility to essential hypersomnia with HLA-DRB1*1501-DQB1*0602 haplotype Taku Miyagawa1, Makoto Honda2,3, Minae Kawashima1,4, Mihoko Shimada1, Susumu Tanaka2, Yutaka Honda3 and Katsushi Tokunaga1 Essential hypersomnia (EHS) exhibits excessive daytime sleepiness without cataplexy and is associated with the HLA-DRB1*1501-DQB1*0602 haplotype, similar to narcolepsy with cataplexy. Single-nucleotide polymorphism (SNP) rs1154155 located in the T-cell receptor a (TCRA) locus has been recently identified as a novel genetic marker of susceptibility for narcolepsy with cataplexy. We investigated whether the SNP was associated with EHS in the Japanese population. We found a significant association with EHS patients possessing the HLA-DRB1*1501-DQB1*0602 haplotype, compared À4 with HLA-matched healthy individuals (Pallele¼0.008; Ppositivity¼5Â10 ), whereas no significant association was observed for EHS patients without this haplotype. Thus, TCRA is a plausible candidate for susceptibility to EHS patients positive for the HLA-DRB1*1501-DQB1*0602 haplotype. Journal of Human Genetics (2010) 55, 63–65; doi:10.1038/jhg.2009.118; published online 20 November 2009 Keywords: essential hypersomnia; HLA; narcolepsy; TCRA INTRODUCTION possible association between SNP rs1154155 in the TCRA locus and Earlier studies have revealed that narcolepsy with cataplexy is asso- essential hypersomnia (EHS), CNS hypersomnia similar to narcolepsy ciated with the human leukocyte antigen (HLA) and T-cell receptor a with cataplexy, with regard to the symptom of excessive daytime (TCRA) genes. -

Sleep Disorders and Sleep Deprivation: an Unmet Public Health Problem
REPORT BRIEF • APRIL 2006 SLEEP DISORDERS AND SLEEP DEPRIVATION: AN UNMET PUBLIC HEALTH PROBLEM It is estimated that 50 to 70 million Americans chronically suffer from a disorder of sleep and wakefulness, hindering daily functioning and adversely affecting their health and longevity. The cumulative effects of sleep loss and sleep disorders represent an under-recognized public health problem and have been associated with a wide range of health consequences including an increased risk of hypertension, diabetes, obesity, depression, heart attack, and stroke. Almost 20 percent of all serious car crash injuries in the general population are associated with driver sleepiness. Hundreds of billions of dollars a year are spent on direct medical costs related to sleep disorders such as doctor visits, hospital services, prescriptions, and over-the-counter medications. Recognizing the health consequences of sleep disorders and sleep deprivation, the American Academy of Sleep Medicine, the National Center on Sleep Disorders Research at the National Institutes of Health, the National Sleep Foundation, and the Sleep Research Society The cumulative requested that the Institute of Medicine review the public health effects of sleep loss significance of sleep, sleep loss, and sleep disorders; examine gaps and sleep disorders in research, education, and training in the public health system and academia; and provide a comprehensive plan for enhancing sleep represent an under- medicine and research. recognized public Sleep Disorders and Sleep Deprivation: An Unmet Public Health health problem and Problem concluded that although scientific opportunities and clinical have been associat- activities in the field are expanding, the available human resources and ed with a wide infrastructural capacity to improve patient care and expand scientific range of health research are insufficient. -
Somnology-Jr-Book.Pdf
1 To Grace Zamudio and Zoe Lee-Chiong. 2 Preface Carpe noctem. Teofilo Lee-Chiong MD Professor of Medicine Division of Sleep Medicine National Jewish Health Denver, Colorado University of Colorado Denver School of Medicine Denver, Colorado Chief Medical Liaison Philips Respironics Murrysville, Pennsylvania 3 Abbreviations AHI Apnea-hypopnea index BPAP Bi-level positive airway pressure CPAP Continuous positive airway pressure CSA Central sleep apnea ECG Electrocardiography EEG Electroencephalography EMG Electromyography EOG Electro-oculography FEV1 Forced expiratory volume in 1 second GABA Gamma-aminobutyric acid N1 NREM stage 1 sleep N2 NREM stage 2 sleep N3 NREM stages 3 (and 4) sleep NREM Non-rapid eye movement O2 Oxygen OSA Obstructive sleep apnea PaCO2 Partial pressure of arterial carbon dioxide PaO2 Partial pressure of arterial oxygen REM Rapid eye movement sleep SaO2 Oxygen saturation SOREMP Sleep onset REM period 4 Table of contents Introduction 15 Neurobiology of sleep 16 Neural systems generating wakefulness 16 Neural systems generating NREM sleep 16 Neural systems generating REM sleep 16 Main neurotransmitters 17 Acetylcholine 17 Adenosine 17 Dopamine 17 Gamma-aminobutyric acid 17 Glutamate 17 Glycine 17 Histamine 18 Hypocretin 18 Melatonin 18 Norepinephrine 18 Serotonin 18 Physiology during sleep 19 Autonomic nervous system 19 Respiratory system 19 Respiratory patterns 19 Cardiovascular system 19 Gastrointestinal system 20 Renal and genito-urinary systems 20 Endocrine system 20 Growth hormone 20 Thyroid stimulating hormone -

Modality Online
Modality online Duration 11 months Language Bilingual (Spanish/English) depending on the students’ The Sleep Institute and the European preference, it can be taken in either Spanish or English. University of Madrid proudly present Bibliography, supporting materials, and webinars in English ONLINE MASTER 60 ECTS credits IN SLEEP 48 | Syllabus and theory MEDICINE 6 | Master’s Thesis 6 | Internship Degree Title Private title issued by the European University of Madrid European Certificate in Somnology Preparation for the ESRS exam 01 Introduction 02 The Master 03 Methodology 04 Program 05 Faculty 06 Calendar 07 Internships 08 Requirements 09 Price 10 Contact 01 Introduction Over the last decade, sleep medicine has evolved from being a field with some medical and scientific interest, into a mature discipline with solid and widely accepted scientific foundations. In addition, given the extensive prevalence of sleep disorders among the population, knowledge and mastery of such is of great interest for the training of doctors, nurses, psychologists, dentists, biologists, etc. Considering the variety of pathologies that can be found within this field of study, it is of great importance for professionals dedicated to sleep medicine to have a multidisciplinary vision. Therefore, developing a master’s degree on sleep medicine that allows a broad and practical knowledge of these disorders is a challenge that we have committed to. 4 From a medical point of view, there are a wide variety of disciplines involved in sleep disorders such as neurology, pneumology, neurophysiology, ENT, odontology, psychiatry, endocrinology, and of course family medicine and paediatrics. Within the training programs in the different medical fields, we find that none are exclusively dedicated to sleep medicine. -

Education in Sleep Disorders in US Dental Schools DDS Programs
Sleep Breath (2012) 16:383–392 DOI 10.1007/s11325-011-0507-z ORIGINAL ARTICLE Education in sleep disorders in US dental schools DDS programs Michael Scott Simmons & Andrew Pullinger Received: 1 September 2010 /Revised: 5 March 2011 /Accepted: 8 March 2011 /Published online: 27 April 2011 # The Author(s) 2011. This article is published with open access at Springerlink.com Abstract ly covered topics included sleep-related breathing disorders Introduction Medical school surveys of pre-doctoral cur- (32 schools) and sleep bruxism (31 schools). Although riculum hours in the somnology, the study of sleep, and its 3.92 h is an improvement from the mean 2.5 h last reported, application in sleep medicine/sleep disorders (SM) show the absolute number of curriculum hours given the slow progress. Limited information is available regarding epidemic scope of sleep problems still appears insufficient dentist training. This study assessed current pre-doctoral in most schools to achieve any competency in screening for dental education in the field of somnology with the SRBD, or sufficient foundation for future involvement in hypothesis that increased curriculum hours are being treatment. devoted to SM but that competencies are still lacking. Materials and methods The 58 US dental schools were Keywords Dental school somnology education . Teaching surveyed for curriculum offered in SM in the 2008/2009 sleep medicine . Competency . Sleep bruxism . Sleep-related academic year using an eight-topic, 52-item questionnaire breathing disorder . Oral appliance therapy mailed to the deans. Two new dental schools with interim accreditation had not graduated a class and were not included. -

What the “Man in the Moon” Can Tell Us About the Future of Our Brains
358 Editorial Page 1 of 5 What the “man in the moon” can tell us about the future of our brains Birgit Högl Department of Neurology, Medical University of Innsbruck, Innsbruck, Austria Correspondence to: Dr. Birgit Högl, MD. Associate Professor of Neurology, Head of the Sleep Disorders Clinic, Department of Neurology, Medical University of Innsbruck, Anichstrasse 35, 6020 Innsbruck, Austria. Email: [email protected]. Provenance: This is a Guest Editorial commissioned by Section Editor Yun Li, MD (Clinical Medicine, Psychiatry, Sleep Medicine Center, Translational Neuroscience Center, West China Hospital, Sichuan University, Chengdu, China). Comment on: Sasai-Sakuma T, Nishio Y, Yokoi K, et al. Pareidolias in REM Sleep Behavior Disorder: A Possible Predictive Marker of Lewy Body Diseases? Sleep 2017;40. Submitted May 17, 2017. Accepted for publication May 27, 2017. doi: 10.21037/atm.2017.06.05 View this article at: http://dx.doi.org/10.21037/atm.2017.06.05 Taeko Sasai-Sakuma and her coauthors from Professor The authors showed that a much larger proportion of Inoue’s research group at the Tokyo Medical University, patients with iRBD exhibited at least one more pareidolic recently published a study (1), which is a timely addition to response than controls, and that a larger number of ongoing research for biomarkers of neurodegeneration in ambiguous pictures evoked pareidolic responses in patients idiopathic RBD (iRBD) (2,3). compared with controls. This suggests that pareidolic Idiopathic RBD is the most specific sign of prodromal responses are elicited more easily in patients with iRBD. Parkinson’s disease, and is now considered an early stage Interestingly, the authors also found that iRBD patients synucleinopathy by itself (4). -

Efficacy and Safety of Modafinil in Patients with Idiopathic Hypersomnia Without Long Sleep Time
Sleep Medicine 80 (2021) 315e321 Contents lists available at ScienceDirect Sleep Medicine journal homepage: www.elsevier.com/locate/sleep Original Article Efficacy and safety of modafinil in patients with idiopathic hypersomnia without long sleep time: a multicenter, randomized, double-blind, placebo-controlled, parallel-group comparison study Yuichi Inoue a, b, *, Toshiyuki Tabata c, Naoji Tsukimori d a Japan Somnology Center, Institute of Neuropsychiatry, 5-10-10 Yoyogi, Shibuya-ku, Tokyo, 151-0053, Japan b Department of Somnology, Tokyo Medical University, 6-7-1 Nishishinjuku, Shinjuku-ku, Tokyo, 160-0023, Japan c Research and Development Headquarters, Alfresa Pharma Corporation, 2-2-9 Koku-machi, Chuo-ku, Osaka, 540-8575, Japan d Medical Affairs Headquarters, Alfresa Pharma Corporation, 2-2-9 Koku-machi, Chuo-ku, Osaka, 540-8575, Japan article info abstract Article history: Background: Few treatments are available for patients with idiopathic hypersomnia (IH). Modafinil, an Received 11 September 2020 established treatment for narcolepsy, was tested for efficacy and safety in Japanese patients with IH Received in revised form without long sleep time. 9 December 2020 Methods: This multicenter, randomized, double-blind, placebo-controlled, parallel-group comparison Accepted 14 January 2021 study was conducted at 20 institutions in Japan. Patients who met the diagnostic criteria of IH in the Available online 20 January 2021 International Classification of Sleep Disorders (second edition) were included. The study comprised a 17-day observation period and a 3-week treatment period during which modafinil (200 mg) or placebo Keywords: fi Modafinil was administered orally once daily (in the morning). The primary ef cacy endpoint was change in mean Idiopathic hypersomnia without long sleep sleep latency on the Maintenance of Wakefulness Test (MWT). -

Somnology Part 2 with Dr. W. Chris Winter Ologies Podcast October 15, 2018
Somnology Part 2 with Dr. W. Chris Winter Ologies Podcast October 15, 2018 Oh heeey. It’s still your little stepbrother who tries to trade you their calcified, banana flavored Now & Laters for your Mini Reese’s Peanut Butter Cups, and you’re like, “Dude. Little dude. Step all the way off. How dare you? That’s not how life works,” Alie Ward, back for the second half of Somnology. Did you listen to Part 1 yet? Deep sleep, versus REM, versus R.E.M., versus light sleep. Which is the Ugg? Which is the glittery dress loafer? Do you regularly disco with the Night Hag? How lucid is your Property Brothers experience? Does C-3PO give you PTSD? If you have no idea what I’m talking about, I have exposed you as having skipped Part 1. So go listen to Part 1! Part 2 will be here for you when you’re done. It will make way more sense. [through bullhorn] Go on, get! Okay, Part 2-ers, it’s just us now. We get it. We have the basics on how sleep works, what happens when we don’t have enough of it, and what our brain waves do, and why insomnia is a product of fear and anxiety. But this episode answers Patreon questions to help you get better sleep, and includes, yes, the secret insomnia buster from your pod dad’s mom, your pod nana, Fancy Nancy Ward. I’m earnestly so excited to share it because I swear it works so well for me. -

Sleep Debt and Social Jetlag Associated with Sleepiness, Mood, and Work Performance Among Workers in Japan
International Journal of Environmental Research and Public Health Article Sleep Debt and Social Jetlag Associated with Sleepiness, Mood, and Work Performance among Workers in Japan Isa Okajima 1,* , Yoko Komada 2 , Wakako Ito 3 and Yuichi Inoue 3,4 1 Department of Psychological Counseling, Faculty of Humanities, Tokyo Kasei University, Tokyo 173-8602, Japan 2 Liberal Arts, Meiji Pharmaceutical University, Tokyo 204-8588, Japan; [email protected] 3 Institute of Neuropsychiatry, Tokyo 162-0851, Japan; [email protected] (W.I.); [email protected] (Y.I.) 4 Department of Somnology, Tokyo Medical University, Tokyo 151-0053, Japan * Correspondence: [email protected] Abstract: Although sleep debt and social jetlag (SJL) influence daytime dysfunctions, the effects of both sleep debt and SJL on them have not been analyzed. The aim of this study was to examine the mutual relationship between sleep debt and SJL on daytime sleepiness, mood, and work performance. This study was a cross-sectional study on sleep health conducted on the Japanese general population. A total of 4505 general workers (30% female, aged 43.57 ± 11.63 years) were selected and analyzed. Sleep debt was defined by sleep debt index (SDI), which is the discrepancy between desired and real sleep duration. SJL and SDI scores exhibited a positive but weak coefficient (r = 0.19). In a 4 (SJL) × 3 (SDI) two-way ANOVA, the interaction effects were notable for sleepiness and depression scores, while the group effects were notable for the work performance score. For sleepiness and depression scores, SDI >2 h was not significantly different from SJL. -

Comparison of Somnologica 3 Computerized Polysomnographic Systems Analysis and Manual Assessment of Sleep Apnea
313 Comparison of Somnologica 3 Computerized Polysomnographic Systems Analysis and Manual Assessment of Sleep Apnea Po-Jui Chang, Meng-Heng Hsieh, Yu-Lun Lo, Chun-Yu Lo, Fu-Tsai Chung, Chih-Hsia Kuo, Horng-Chyuan Lin Sleep disorders are increasingly being recognized by physicians, raising demand at sleep laboratories, and prompting a search for user-friendly methods of data analysis. Computerized polysomnographic systems have become a commonly used tool in sleep laboratories in Taiwan and throughout the world. This study was designed to compare the accuracy of data analysis using computerized Somnologica 3 systems and manual interpretation. Twenty-three patients with suspected respiratory sleep disorders were referred to our department from outpatient clinics. Each individual underwent a full-night sleep study in our sleep laboratory. Recorded data were simultaneously analyzed using the computerized Somnologica 3 system (Version II software) and interpreted by a pulmonologist thoroughly experienced in polysomnography, using the standard Rechtschaffen and Kales criteria. When comparing autoscoring and manual analysis, our results revealed that the computerized system produced more substantial errors with respect to the duration of each sleep stage (S1 sleep time: 34.9 ± 5.7 vs. 74.2 ± 10.4 min; S2: 94.5 ± 15.1 vs. 208.9 ± 15.8 min; S4: 36.4 ± 5.4 vs. 14.5 ± 4.1 min; REM: 26.1 ± 5.4 vs. 55.4 ± 6.2 min, respectively; all p<0.05), thus leading to a reduction not only in estimated total sleep time (226.2 ± 19.9 vs. 376.4 ± 16.4 min; p<0.05), but also a decrease in the number of hypopnea/apnea events (AHI 13.0 ± 19.5 vs.