ROCEPHIN (Ceftriaxone Sodium)
Total Page:16
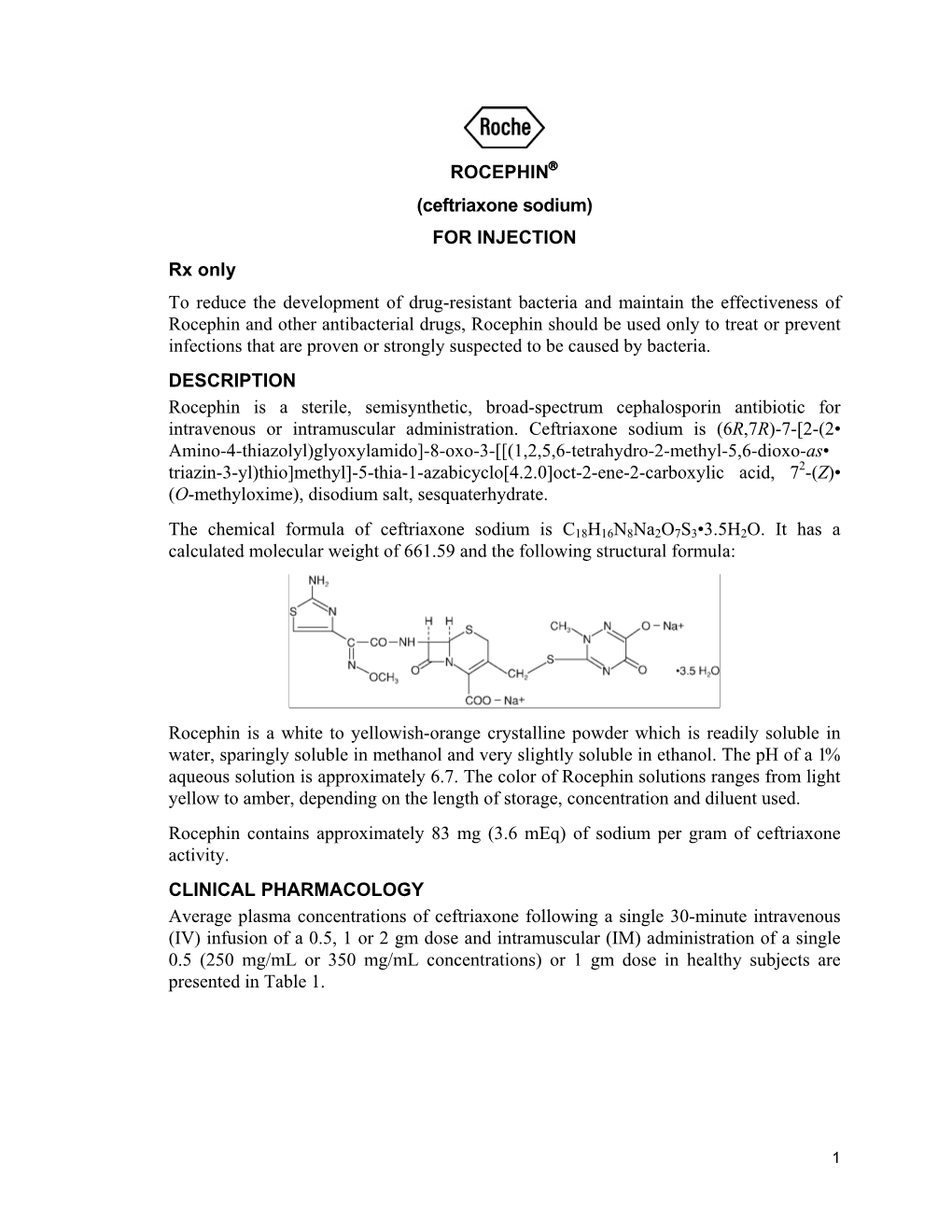
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Severe Sepsis and Septic Shock Antibiotic Guide
Stanford Health Issue Date: 05/2017 Stanford Antimicrobial Safety and Sustainability Program Severe Sepsis and Septic Shock Antibiotic Guide Table 1: Antibiotic selection options for healthcare associated and/or immunocompromised patients • Healthcare associated: intravenous therapy, wound care, or intravenous chemotherapy within the prior 30 days, residence in a nursing home or other long-term care facility, hospitalization in an acute care hospital for two or more days within the prior 90 days, attendance at a hospital or hemodialysis clinic within the prior 30 days • Immunocompromised: Receiving chemotherapy, known systemic cancer not in remission, ANC <500, severe cell-mediated immune deficiency Table 2: Antibiotic selection options for community acquired, immunocompetent patients Table 3: Antibiotic selection options for patients with simple sepsis, community acquired, immunocompetent patients requiring hospitalization. Risk Factors for Select Organisms P. aeruginosa MRSA Invasive Candidiasis VRE (and other resistant GNR) Community acquired: • Known colonization with MDROs • Central venous catheter • Liver transplant • Prior IV antibiotics within 90 day • Recent MRSA infection • Broad-spectrum antibiotics • Known colonization • Known colonization with MDROs • Known MRSA colonization • + 1 of the following risk factors: • Prolonged broad antibacterial • Skin & Skin Structure and/or IV access site: ♦ Parenteral nutrition therapy Hospital acquired: ♦ Purulence ♦ Dialysis • Prolonged profound • Prior IV antibiotics within 90 days ♦ Abscess -

Penicillin Allergy Guidance Document
Penicillin Allergy Guidance Document Key Points Background Careful evaluation of antibiotic allergy and prior tolerance history is essential to providing optimal treatment The true incidence of penicillin hypersensitivity amongst patients in the United States is less than 1% Alterations in antibiotic prescribing due to reported penicillin allergy has been shown to result in higher costs, increased risk of antibiotic resistance, and worse patient outcomes Cross-reactivity between truly penicillin allergic patients and later generation cephalosporins and/or carbapenems is rare Evaluation of Penicillin Allergy Obtain a detailed history of allergic reaction Classify the type and severity of the reaction paying particular attention to any IgE-mediated reactions (e.g., anaphylaxis, hives, angioedema, etc.) (Table 1) Evaluate prior tolerance of beta-lactam antibiotics utilizing patient interview or the electronic medical record Recommendations for Challenging Penicillin Allergic Patients See Figure 1 Follow-Up Document tolerance or intolerance in the patient’s allergy history Consider referring to allergy clinic for skin testing Created July 2017 by Macey Wolfe, PharmD; John Schoen, PharmD, BCPS; Scott Bergman, PharmD, BCPS; Sara May, MD; and Trevor Van Schooneveld, MD, FACP Disclaimer: This resource is intended for non-commercial educational and quality improvement purposes. Outside entities may utilize for these purposes, but must acknowledge the source. The guidance is intended to assist practitioners in managing a clinical situation but is not mandatory. The interprofessional group of authors have made considerable efforts to ensure the information upon which they are based is accurate and up to date. Any treatments have some inherent risk. Recommendations are meant to improve quality of patient care yet should not replace clinical judgment. -

Safety and Efficacy of Ceftaroline Fosamil in the Management of Community-Acquired Bacterial Pneumonia Heather F
Philadelphia College of Osteopathic Medicine DigitalCommons@PCOM PCOM Scholarly Papers 2014 Safety and Efficacy of Ceftaroline Fosamil in the Management of Community-Acquired Bacterial Pneumonia Heather F. DeBellis Kimberly L. Barefield Philadelphia College of Osteopathic Medicine, [email protected] Follow this and additional works at: https://digitalcommons.pcom.edu/scholarly_papers Part of the Medicine and Health Sciences Commons Recommended Citation DeBellis, Heather F. and Barefield, Kimberly L., "Safety and Efficacy of Ceftaroline Fosamil in the Management of Community- Acquired Bacterial Pneumonia" (2014). PCOM Scholarly Papers. 1913. https://digitalcommons.pcom.edu/scholarly_papers/1913 This Article is brought to you for free and open access by DigitalCommons@PCOM. It has been accepted for inclusion in PCOM Scholarly Papers by an authorized administrator of DigitalCommons@PCOM. For more information, please contact [email protected]. Open Access: Full open access to Clinical Medicine Reviews this and thousands of other papers at http://www.la-press.com. in Therapeutics Safety and Efficacy of Ceftaroline Fosamil in the Management of Community- Acquired Bacterial Pneumonia Heather F. DeBellis and Kimberly L. Tackett South University School of Pharmacy, Savannah, GA, USA. ABSTR ACT: Ceftaroline fosamil is a new fifth-generation cephalosporin indicated for the treatment of community-acquired bacterial pneumonia (CABP). It possesses antimicrobial effects against both Gram-positive and Gram-negative bacteria, including methicillin-resistant Staphylococcus aureus (MRSA), but not against anaerobes. Organisms covered by this novel agent that are commonly associated with CABP are Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, Moraxella catarrhalis, and Klebsiella pneumoniae; however, ceftaroline fosamil lacks antimicrobial activity against Pseudomonas and Acinetobacter species. -

Cephalosporins Can Be Prescribed Safely for Penicillin-Allergic Patients ▲
JFP_0206_AE_Pichichero.Final 1/23/06 1:26 PM Page 106 APPLIED EVIDENCE New research findings that are changing clinical practice Michael E. Pichichero, MD University of Rochester Cephalosporins can be Medical Center, Rochester, NY prescribed safely for penicillin-allergic patients Practice recommendations an allergic reaction to cephalosporins, ■ The widely quoted cross-allergy risk compared with the incidence of a primary of 10% between penicillin and (and unrelated) cephalosporin allergy. cephalosporins is a myth (A). Most people produce IgG and IgM antibodies in response to exposure to ■ Cephalothin, cephalexin, cefadroxil, penicillin1 that may cross-react with and cefazolin confer an increased risk cephalosporin antigens.2 The presence of of allergic reaction among patients these antibodies does not predict allergic, with penicillin allergy (B). IgE cross-sensitivity to a cephalosporin. ■ Cefprozil, cefuroxime, cefpodoxime, Even penicillin skin testing is generally not ceftazidime, and ceftriaxone do not predictive of cephalosporin allergy.3 increase risk of an allergic reaction (B). Reliably predicting cross-reactivity ndoubtedly you have patients who A comprehensive review of the evidence say they are allergic to penicillin shows that the attributable risk of a cross- U but have difficulty recalling details reactive allergic reaction varies and is of the reactions they experienced. To be strongest when the chemical side chain of safe, we often label these patients as peni- the specific cephalosporin is similar to that cillin-allergic without further questioning of penicillin or amoxicillin. and withhold not only penicillins but Administration of cephalothin, cepha- cephalosporins due to concerns about lexin, cefadroxil, and cefazolin in penicillin- potential cross-reactivity and resultant IgE- allergic patients is associated with a mediated, type I reactions. -

A Thesis Entitled an Oral Dosage Form of Ceftriaxone Sodium Using Enteric
A Thesis entitled An oral dosage form of ceftriaxone sodium using enteric coated sustained release calcium alginate beads by Darshan Lalwani Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Master of Science Degree in Pharmaceutical Sciences with Industrial Pharmacy Option _________________________________________ Jerry Nesamony, Ph.D., Committee Chair _________________________________________ Sai Hanuman Sagar Boddu, Ph.D, Committee Member _________________________________________ Youssef Sari, Ph.D., Committee Member _________________________________________ Patricia R. Komuniecki, PhD, Dean College of Graduate Studies The University of Toledo May 2015 Copyright 2015, Darshan Narendra Lalwani This document is copyrighted material. Under copyright law, no parts of this document may be reproduced without the expressed permission of the author. An Abstract of An oral dosage form of ceftriaxone sodium using enteric coated sustained release calcium alginate beads by Darshan Lalwani Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Master of Science Degree in Pharmaceutical Sciences with Industrial Pharmacy option The University of Toledo May 2015 Purpose: Ceftriaxone (CTZ) is a broad spectrum semisynthetic, third generation cephalosporin antibiotic. It is an acid labile drug belonging to class III of biopharmaceutical classification system (BCS). It can be solvated quickly but suffers from the drawback of poor oral bioavailability owing to its limited permeability through -

Comparison of Ceftriaxone and Cefazolin Sodium Antibiotic
ORIGINAL RESEARCH General Urology Doi: 10.4274/jus.galenos.2018.2367 Journal of Urological Surgery, 2019;6(2):111-117 Comparison of Ceftriaxone and Cefazolin Sodium Antibiotic Prophylaxis in Terms of SIRS/Urosepsis Rates in Patients Undergoing Percutaneous Nephrolithotomy Perkütan Nefrolitotomi Ameliyatı Olan Hastalara Verilen Seftriakson ve Sefazolin Sodyum Antibiyotik Profilaksilerinin SIRS/Ürosepsis Oranları Açısından Karşılaştırılması Kerem Taken1, Alper Aşık1, Recep Eryılmaz1, Rahmi Aslan1, Muhammet İrfan Dönmez2, Mustafa Güneş1 1Yüzüncü Yıl University Faculty of Medicine, Department of Urology, Van, Turkiye 2Konya Training and Research Hospital, Clinic of Urology, Konya, Turkiye What’s known on the subject? and What does the study add? Percutaneous nephrolithotomy have infectious complications in the form of systemic inflammatory response (SIRS) and urosepsis. Antibiotic prophylaxis in order to prevent this complication has been widely investigated. Our prospective randomized study highlights two commonly used antibiotics in Turkiye and their effects on infectious complications. Our results indicate similar SIRS/urosepsis rates between groups and hence we advise to use cefazolin that has a narrower anti-bacterial spectrum. Abstract Objective: The aim of this study is to compare ceftriaxone and cefazoline sodium antibiotic prophylaxis in terms of development of Systemic Inflammatory Response syndrome (SIRS)/urosepsis in patients undergoing percutaneous nephrolithotomy (PCNL). Materials and Methods: Patients who underwent PCNL between June 2015 and October 2015 in our hospital were prospectively randomized to ceftriaxone (n=30) and cefazoline sodium (n=32) antibiotic prophylaxis groups. Patients with predisposing conditions to SIRS were excluded. Intraoperative urine cultures from renal pelvis and stone cultures were obtained from all patients. Clinical and laboratory findings of the patients who developed postoperative fever were evaluated. -

Surgical Antibiotic Prophylaxis
Surgical Antibiotic Prophylaxis - Adult Page 1 of 6 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. Local microbiology and susceptibility/resistance patterns should be taken into consideration when selecting antibiotics. Patients scheduled for surgery should have the following antibiotics administered prior to their procedure: ● Vancomycin, ciprofloxacin/levofloxacin, and gentamicin are to be initiated 60 to 120 minutes prior to incision, and all other antibiotics are to be initiated within 60 minutes of incision ● Carefully evaluate allergy histories before using alternative agents - the majority of patients with listed penicillin allergies can safely be given cephalosporins or carbapenems ● If the patient has multiple known antibiotic drug allergies, is colonized with or has a history of a recent multi-drug infection, administer antibiotics as indicated or consider an outpatient Infectious Diseases consultation ● Discontinue all antibiotics within 24 hours of first dose except for: 1) Treatment of established infection, 2) Prophylaxis of prosthesis in the setting of postoperative co-located -

Ceftriaxone Ceftriaxone Is an Antibiotic Given by Injection Into a Muscle for the Treatment of Certain Sexually Transmitted Infections (STI)
Clinical Prevention Services Tel 604.707.5600 Provincial STI/HIV Clinic Fax 604.707.5604 655 West 12th Avenue www.bccdc.ca Vancouver, BC V5Z 4R4 www.SmartSexResource.com Ceftriaxone Ceftriaxone is an antibiotic given by injection into a muscle for the treatment of certain sexually transmitted infections (STI). Allergies • Tell your healthcare provider if you have a history of an anaphylactic allergy or immediate reaction to any penicillin antibiotic such as penicillin V-K, amoxicillin (Amoxil®) or any cephalosporin antibiotic such as cefixime (Suprax®), ceftriaxone (Rocephin®) • Tell your healthcare provider if you have an allergy to lidocaine, or other local anesthetics of the amide type e.g. prilocaine (lidocaine is mixed with ceftriaxone to reduce pain at the injection site). Pregnancy and Chest/Breastfeeding Ceftriaxone may be used with caution during pregnancy and chest/breastfeeding. Please consult your healthcare provider. CAUTION • Drug Interactions: Tell your healthcare provider if you are taking any prescription, non-prescription, herbal, or recreational products. Not all individual drug interactions are listed in this document. • Tell your healthcare provider if you have any gallbladder, liver, kidney, pancreas or bleeding disorder, or a history of stomach dysfunction, particularly colitis. • Do not take the following medications with ceftriaxone: ® Oral Typhoid vaccine (Vivotif ) o • Ceftriaxone may interfere with certain urine glucose tests. (Clinitest ) • Ceftriaxone is contraindicated in preterm newborns or infants less than one month old with high blood levels of bilirubin. Side Effects • You may experience discomfort, redness or swelling at the injection site. • You may experience skin rash or diarrhea. • If any of these effects persist or worsen, please contact your healthcare provider. -

Cephalosporins
Appropriate use of CEPHALOSPORINS 22 | BPJ | Issue 41 Understanding cephalosporins Cephalosporins are broad spectrum antibiotics similar to Key concepts penicillins. They have a beta-lactam ring which interferes ■ There are few infections where cephalosporins with bacterial cell wall synthesis by binding to penicillin- are the antibiotics of first choice and their use binding proteins, eventually leading to cell lysis and death.1 should be avoided when other more narrow Like amoxicillin clavulanate, cephalosporins should be spectrum antibiotics remain effective avoided when a narrower spectrum antibiotic would be ■ effective because they increase the risk of Clostridium Ceftriaxone is an appropriate first line treatment difficile, MRSA and other resistant infections. for gonorrhoea, pelvic inflammatory disease and epididymo-orchitis Cephalosporins mainly used in general practice are; ■ Ceftriaxone may also be used for suspected cefaclor, cephalexin and ceftriaxone (injection). Other meningitis in patients allergic to penicillin cephalosporins available on the Pharmaceutical Schedule (benzylpenicillin is first-line) are; cefazolin, cefoxitin and cefuroxime – these medicines ■ Cefaclor may be considered as a second-line are usually prescribed for patients undergoing dialysis and treatment for otitis media, sinusitis, cellulitis, for patients with cystic fibrosis. diabetic foot infection and mastitis ■ Cephalexin is a third-line alternative for the Cephalosporins are grouped based on their antibacterial treatment of urinary tract infection in pregnant 2 properties and when they were introduced: women (after nitrofurantoin and trimethoprim) ▪ First generation cephalosporins include cephalexin and cefazolin. They have good activity against a wide spectrum of Gram-positive bacteria including penicillinase-producing staphylococci. However, they are not active against methicillin-resistant staphylococci (MRSA). Enterococci are resistant.2 ▪ Second generation cephalosporins include cefaclor, cefuroxime and cefoxitin. -

Efficacy and Safety of Injectable and Oral Antibiotics in Treating Gonorrhea
Journal of Clinical Medicine Article Efficacy and Safety of Injectable and Oral Antibiotics in Treating Gonorrhea: A Systematic Review and Network Meta-Analysis Jiaru Yang * , Subhash Dhital and Thomas Naderer * Department of Biochemistry & Molecular Biology, Biomedicine Discovery Institute, Monash University, Clayton, VIC 3800, Australia; [email protected] * Correspondence: [email protected] or [email protected] (J.Y.); [email protected] (T.N.) Received: 22 October 2019; Accepted: 9 December 2019; Published: 11 December 2019 Abstract: Gonorrhea is the second most frequently reported sexually transmitted infectious disease of bacterial origin in the world. Current empiric therapies rely on broad-spectrum antibiotics. However, treatment options are becoming limited due to the rise of drug-resistant gonorrhea. To control the rise of drug-resistant gonorrhea and to identify alternative treatment options, clinicians will have to increasingly rely on experimental evidence for the treatment of gonorrhea patients. Thus, we performed a systematic review and network meta-analysis of all randomized clinical trials about the efficacy and safety of various antibiotic regimens in adults with gonorrhea. We searched all references in Embase and PubMed from the date of their inception to January 2019, and then an updated search was performed in March 2019. Of the 28,843 identified references, 44 fulfilled our selection criteria. We used a network meta-analysis based on a frequentist approach to evaluate the efficacy and safety of 12 injectable and 11 oral antibiotics. The efficacy of treatments was ranked by p score and inconsistency was assessed by a back-calculation method. Certainty of evidence was evaluated by the GRADE system. -

N200327s0160
Clinical Review Sheral S. Patel, M.D. NDA 200327 SD478 S-16 and S-17 Ceftaroline fosamil (Teflaro®) CLINICAL REVIEW Application Type Pediatric Efficacy Supplements Application Number(s) NDA 200327 SD478 S-16 and S-17 Priority or Standard Priority Submit Date 7 December 2015 Received Date 7 December 2015 PDUFA Goal Date 7 June 2016 Division/Office Division of Anti-Infective Products/ OAP/ OND/ CDER Reviewer Name Sheral S. Patel, M.D. Team Leader Hala Shamsuddin, M.D. Review Completion Date 13 May 2016 Established Name Ceftaroline fosamil (Proposed) Trade Name Teflaro® Applicant Cerexa, Inc. (A Subsidiary of Forest Laboratories, LLC.) Formulation(s) Powder for Injection Dosing Regimen 1. Children aged 2 months to < 2 years: 8 mg/kg every 8 hours IV administered over 5 to 60 minutes 2. Children and adolescents aged 2 years to ≤ 18 years: 12 mg/kg (up to a maximum of 400 mg for pediatric patients weighing > 33 kg) q8h by IV infusion administered over 5 to 60 minutes Applicant Proposed For the pediatric population 2 months to < 18 years Indication(s)/Population(s) 1. Acute bacterial skin and skin structure infections 2. Community acquired bacterial pneumonia Recommendation on Approval Regulatory Action Recommended For the pediatric population 2 months to < 18 years Indication(s)/Population(s) 1. Acute bacterial skin and skin structure infections (if applicable) 2. Community acquired bacterial pneumonia CDER Clinical Review Template 2015 Edition 1 Reference ID: 3933750 Clinical Review Sheral S. Patel, M.D. NDA 200327 SD478 S-16 and S-17 Ceftaroline fosamil (Teflaro®) Table of Contents Glossary ........................................................................................................................................ -

Safety in Neonates Ceftriaxone Has a Broad Spectrum of in Vitro Activity
Second Meeting of the Subcommittee of the Expert Committee on the Selection and Use of Essential Medicines Geneva, 29 September to 3 October 2008 Ceftriaxone – safety in neonates Ceftriaxone has a broad spectrum of in vitro activity and is used in neonates for treating gonococcal ophthalmia and as a second line drug for sepsis and meningitis. It can precipitate if used together with calcium leading to severe reactions including neonatal death. Other possible adverse events of significance in the neonate include biliary sludging, kernicterus and increased chances of invasive candidiasis. Third generation cephalosporin use can also lead to an increase in infections due to Extended spectrum beta lactamase (ESBL) producing organisms. A recent FDA alert advocates that ceftriaxone should not be mixed with calcium- containing products and not administered in the same or different infusion lines or sites in any patient within 48 hours of each other. This can be problematic in neonates especially in those requiring total parenteral nutrition. A letter (Nov, 2006) to health professionals from AFSSAPS, France states that ceftriaxone is contra indicated in premature infants till 41 weeks of age (GA at delivery + wks after birth) and in term neonates less than 28 days if there is hyper bilirubinemia or if receiving calcium. BNF C recommends caution in preterm neonates and states it is contra indicated in neonates with jaundice, hypoalbuminemia, acidosis or impaired bilirubin binding. It is administered either IM or IV. Maximum single dose for neonates is 150mg. The strengths commercially available are 250 mg, 500mg and 1gm as powder for injection. Recommendation Age restriction required – since fatal adverse events are reported Not for use in premature infants till 41 wks total age Consider restriction below 1 m since there are several situations where it is contraindicated in this age group and other alternatives available Review Ceftriaxone is used mostly in hospital practice for neonatal sepsis, meningitis and ophthalmia neonatorum.