Recommendations of the Advisory Committee on Immunization Practices (ACIP): Use of Vaccines and Immune Globulins in Persons with Altered Immunocompetence
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RNA-Based Adjuvant CV8102 Enhances the Immunogenicity of a Licensed Rabies Vaccine in a first-In-Human Trial
Vaccine 37 (2019) 1819–1826 Contents lists available at ScienceDirect Vaccine journal homepage: www.elsevier.com/locate/vaccine RNA-based adjuvant CV8102 enhances the immunogenicity of a licensed rabies vaccine in a first-in-human trial Fatma Doener a,1, Henoch S. Hong a,1, Ingo Meyer b,1, Keyvan Tadjalli-Mehr c, Angelika Daehling c, ⇑ Regina Heidenreich a, Sven D. Koch a, Mariola Fotin-Mleczek a, Ulrike Gnad-Vogt c, a Curevac AG, Paul-Ehrlich-Strasse 15, 72076 Tübingen, Germany b CRS Clinical Research Services Mönchengladbach GmbH, 41061 Mönchengladbach, Germany c Curevac AG, Schumannstrasse 27, 60325 Frankfurt, Germany article info abstract Article history: Background: We report the first-in-concept human trial of the safety, tolerability and immunogenicity Received 27 September 2018 when a novel TLR 7/8/RIG I agonist RNA-based adjuvant, CV8102, was administered alone or mixed with Received in revised form 30 January 2019 fractional doses of a licensed rabies vaccine (RabipurÒ) as model antigen. Accepted 3 February 2019 Methods: The primary objective was to assess the safety and reactogenicity of various dose levels of Available online 21 February 2019 CV8102 alone or mixed with RabipurÒ in healthy 18–40 year-old male volunteers. A secondary objective was to assess the immune-enhancing potential of bedside-mixes of CV8102 with fractional doses of Keywords: Ò Rabipur by measuring induction of rabies virus neutralising titres (VNTs). Adjuvant Results: Fifty-six volunteers received 50–100 lg CV8102 alone (n = 11), bedside-mixed CV8102 and RNA Ò Ò Ò Rabies Rabipur (n = 20), or Rabipur alone (n = 25; control). -

362.Full.Pdf
AMERICAN ACADEMY OF PEDIATRICS Committee on Infectious Diseases Policy Statement: Recommendations for the Prevention of Pneumococcal Infections, Including the Use of Pneumococcal Conjugate Vaccine (Prevnar), Pneumococcal Polysaccharide Vaccine, and Antibiotic Prophylaxis ABSTRACT. Heptavalent pneumococcal conjugate vac- lular pertussis; HbOC, Haemophilus influenzae type b conjugate cine (PCV7) is recommended for universal use in chil- vaccine; HIV, human immunodeficiency virus; AOM, acute otitis dren 23 months and younger, to be given concurrently media. with other recommended childhood vaccines at 2, 4, 6, and 12 to 15 months of age. For children 7 to 23 months he purpose of this report is to provide recom- old who have not received previous doses of PCV7, ad- ministration of a reduced number of doses is recom- mendations for use of the heptavalent pneumo- mended. Two doses of PCV7 are recommended for chil- Tcoccal conjugate vaccine (PCV7), Prevnar (Led- dren 24 to 59 months old at high risk of invasive erle Laboratories, Pearl River, NY; Wyeth-Ayerst pneumococcal infection—including children with func- Pharmaceuticals, Marietta, PA), and 23-valent pneumo- tional, anatomic, or congenital asplenia; infection with coccal polysaccharide (23PS) vaccines. In addition, rec- human immunodeficiency virus; and other predisposing ommendations for the continuing use of antibiotic pro- conditions—who have not been immunized previously phylaxis in children with sickle cell disease (SCD) and with PCV7. Recommendations have been made for use of asplenia will be given, and the use of antibiotics and 23-valent pneumococcal polysaccharide (23PS) vaccine in vaccines in children who attend out-of-home care will high-risk children to expand serotype coverage. -

USDA-Approved Animal Rabies Vaccines
United States Department of Agriculture (USDA) Approved Animal Rabies Vaccines Table 1. Rabies Vaccines Licensed and Marketed in the United States, 2016 Age at For use Route of Product Name Produced by Marketed by Dose primary Booster vaccination in inoculation vaccination* A) MONOVALENT (Inactivated) RAB RABVAC 1 Boehringer Boehringer Dogs 1 ml 3 months Annually IM or SC Ingelheim Ingelheim Vetmedica Cats 1 ml 3 months Annually IM or SC Vetmedica Inc Inc License No. 124 RABVAC 3 Boehringer Boehringer Dogs 1 ml 3 months 1 year later & triennially IM or SC Ingelheim Ingelheim Vetmedica Cats 1 ml 3 months 1 year later & triennially IM or SC Vetmedica Inc Inc Horses 2 ml 3 months Annually IM License No. 124 EQUIRAB with Merck Animal Merck Animal Health Horses 1 ml 4 months Annually IM Havlogen Health License No. 165A DEFENSOR 1 Zoetis Zoetis Dogs 1 ml 3 months Annually IM or SC License No. 190 Cats 1 ml 3 months Annually SC DEFENSOR 3 Zoetis Zoetis Dogs 1 ml 3 months 1 year later & triennially IM or SC License No. 190 Cats 1 ml 3 months 1 year later & triennially SC Sheep 2 ml 3 months Annually IM Cattle 2 ml 3 months Annually IM NOBIVAC: 1- Zoetis Merck Animal Health Dogs 1 ml 3 months Annually IM or SC Rabies License No. 190 Cats 1 ml 3 months Annually SC NOBIVAC: 3- Zoetis Merck Animal Health Dogs 1 ml 3 months 1 year later & triennially IM or SC Rabies and 3- License No. 190 Cats 1 ml 3 months 1 year later & triennially SC Rabies CA Sheep 2 ml 3 months Annually IM Cattle 2 ml 3 months Annually IM IMRAB 1 Merial, Inc Merial, Inc Dogs 1 ml 3 months Annually SC License No. -
A Guide to Vaccinations for Parents
A GUIDE TO VACCINATIONS FOR PARENTS What are vaccines? When should my child be vaccinated? Why does my child need the HPV vaccine? HISTORY OF VACCINATIONS Smallpox is a serious infectious disease that causes fever and a distinctive, progressive 600 1796 skin rash. years ago Edward Jenner developed Variolation, intentionally a vaccine against smallpox. Cases of paralysis from polio in the U.S. exposing an individual to Almost 200 years later, in 1980, in the early 1950s: smallpox material, traces back the World Health Organization more than to 16th-century China. This declared that smallpox process resulted in a milder had been eradicated, 15,000 form of the disease. or wiped out. In the year 2017: Childhood vaccines can prevent 14 potentially serious 0 diseases or conditions throughout your child’s lifetime. 1955 1940s 1885 Jonas Salk’s polio vaccine The routine immunization Louis Pasteur developed a was proven safe and effective. schedule included vaccines vaccine against rabies. The Polio has now been eliminated against four potentially serious rabies vaccine series, which in the U.S., and organizations diseases (smallpox, diphtheria, can be given to people who are currently working tetanus, and pertussis). may have been exposed to to eradicate polio Now the schedule includes the virus, has made rabies worldwide. vaccines to prevent a total infection very rare in the of 14 conditions. United States. In the U.S., vaccines go through three phases of clinical trials to make sure they are safe and effective before they are licensed. 2006 Today The HPV vaccine was Vaccine research licensed in the U.S. -
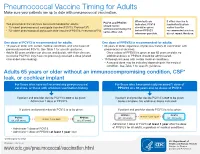
Pneumococcal Vaccine Timing for Adults Make Sure Your Patients Are up to Date with Pneumococcal Vaccination
Pneumococcal Vaccine Timing for Adults Make sure your patients are up to date with pneumococcal vaccination. When both are If either vaccine is PCV13 and PPSV23 Two pneumococcal vaccines are recommended for adults: indicated, PCV13 inadvertently given should not be 13-valent pneumococcal conjugate vaccine (PCV13, Prevnar13®) should be given earlier than the administered during the ® before PPSV23 recommended window, 23-valent pneumococcal polysaccharide vaccine (PPSV23, Pneumovax 23) same office visit. whenever possible. do not repeat the dose. One dose of PCV13 is recommended for adults: One dose of PPSV23 is recommended for adults: 19 years or older with certain medical conditions and who have not 65 years or older, regardless of previous history of vaccination with previously received PCV13. See Table 1 for specific guidance. pneumococcal vaccines. Adults 65 years or older can discuss and decide, with their clinician, – Once a dose of PPSV23 is given at age 65 years or older, no to receive PCV13 if they have not previously received a dose (shared additional doses of PPSV23 should be administered. clinical decision-making). 19 through 64 years with certain medical conditions. – A second dose may be indicated depending on the medical condition. See Table 1 for specific guidance. Adults 65 years or older without an immunocompromising condition, CSF* leak, or cochlear implant For those who have not received any pneumococcal For those who have previously received 1 dose of vaccines, or those with unknown vaccination history PPSV23 at ≥ 65 years and no doses of PCV13 If patient and provider decide PCV13 is not to be given: If patient and provider decide PCV13 is not to be given: Administer 1 dose of PPSV23. -

Adults with DIABETES Are Among Those Who Need Pneumococcal
Patients with diabetes are at an increased risk for complications from pneumococcal disease. Diabetes may be a unique risk factor for increased incidence of sepsis associated with pneumococcal infection. One of the reasons people with diabetes are at greater risk for pneumococcal disease is that they may have abnormalities in immune function that affect their reaction to infection. Pneumococcal disease causes serious illnesses like pneumonia, meningitis, and sepsis. Pneumococcal disease is serious and deadly. In the US, pneumococcal pneumonia, meningitis, and sepsis kill tens of thousands each year. Pneumococcal disease survivors may suffer hearing loss, seizures, blindness, or paralysis. Pneumococcal vaccination is recommended for all adults with diabetes. Adults with DIABETES Are Among Those Who Need Pneumococcal Vaccination There are two types of pneumococcal vaccine recommended for US adults: a pneumococcal conjugate vaccine (PCV13) and a pneumococcal polysaccharide vaccine (PPSV23). Adults 65 and older, and adults age 19 to 64 years with any of the following need to receive both vaccines: immunocompromising conditions or treatments (e.g., HIV/AIDS, leukemia, lymphoma, Hodgkin disease, radiation therapy); a damaged or missing spleen; cochlear implants; or cerebrospinal fluid leaks. Other adults for whom pneumococcal vaccination is recommended only need PPSV23, but may need more than one dose and will need PCV13 when they, too, reach age 65. Please refer to the Adult Pneumococcal Vaccination Guide or visit cdc.gov/vaccines/vpd-vac/pneumo/ for details on timing of vaccine doses. For more information and resources to educate patients about pneumococcal disease, visit adultvaccination.org/professional-resources/pneumo This initiative is supported by unrestricted educational grants from Merck & Co., Inc. -

Vaccinia Virus
APPENDIX 2 Vaccinia Virus • Accidental infection following transfer from the vac- cination site to another site (autoinoculation) or to Disease Agent: another person following intimate contact Likelihood of Secondary Transmission: • Vaccinia virus • Significant following direct contact Disease Agent Characteristics: At-Risk Populations: • Family: Poxviridae; Subfamily: Chordopoxvirinae; • Individuals receiving smallpox (vaccinia) vaccination Genus: Orthopoxvirus • Individuals who come in direct contact with vacci- • Virion morphology and size: Enveloped, biconcave nated persons core with two lateral bodies, brick-shaped to pleo- • Those at risk for more severe complications of infec- morphic virions, ~360 ¥ 270 ¥ 250 nm in size tion include the following: • Nucleic acid: Nonsegmented, linear, covalently ᭺ Immune-compromised persons including preg- closed, double-stranded DNA, 18.9-20.0 kb in length nant women • Physicochemical properties: Virus is inactivated at ᭺ Patients with atopy, especially those with eczema 60°C for 8 minutes, but antigen can withstand 100°C; ᭺ Patients with extensive exfoliative skin disease lyophilized virus maintains potency for 18 months at 4-6°C; virus may be stable when dried onto inanimate Vector and Reservoir Involved: surfaces; susceptible to 1% sodium hypochlorite, • No natural host 2% glutaraldehyde, and formaldehyde; disinfection of hands and environmental contamination with soap Blood Phase: and water are effective • Vaccinia DNA was detected by PCR in the blood in 6.5% of 77 military members from 1 to 3 weeks after Disease Name: smallpox (vaccinia) vaccination that resulted in a major skin reaction. • Progressive vaccinia (vaccinia necrosum or vaccinia • In the absence of complications after immunization, gangrenosum) recently published PCR and culture data suggest that • Generalized vaccinia viremia with current vaccines must be rare 3 weeks • Eczema vaccinatum after vaccination. -

Mm7002e1 Allergic Reactions Including Anaphylaxis After Receipt
Morbidity and Mortality Weekly Report Early Release / Vol. 70 January 6, 2021 Allergic Reactions Including Anaphylaxis After Receipt of the First Dose of Pfizer-BioNTech COVID-19 Vaccine — United States, December 14–23, 2020 CDC COVID-19 Response Team; Food and Drug Administration As of January 3, 2021, a total of 20,346,372 cases of were determined not to be anaphylaxis, 86 were judged to coronavirus disease 2019 (COVID-19) and 349,246 associ- be nonanaphylaxis allergic reactions, and 61 were considered ated deaths have been reported in the United States. Long- nonallergic adverse events. Seven case reports were still under term sequalae of COVID-19 over the course of a lifetime investigation. This report summarizes the clinical and epide- currently are unknown; however, persistent symptoms and miologic characteristics of case reports of allergic reactions, serious complications are being reported among COVID-19 including anaphylaxis and nonanaphylaxis allergic reactions, survivors, including persons who initially experience a mild after receipt of the first dose of Pfizer-BioNTech COVID-19 acute illness.* On December 11, 2020, the Food and Drug vaccine during December 14–23, 2020, in the United States. Administration (FDA) issued an Emergency Use Authorization CDC has issued updated interim clinical considerations for (EUA) for Pfizer-BioNTech COVID-19 vaccine to prevent use of mRNA COVID-19 vaccines currently authorized in the COVID-19, administered as 2 doses separated by 21 days. On United States (4) and interim considerations for preparing for December 12, 2020, the Advisory Committee on Immunization the potential management of anaphylaxis (5). In addition to Practices (ACIP) issued an interim recommendation for use screening for contraindications and precautions before admin- of Pfizer-BioNTech COVID-19 vaccine (1); initial doses were istering COVID-19 vaccines, vaccine locations should have recommended for health care personnel and long-term care the necessary supplies available to manage anaphylaxis, should facility residents (2). -

(ACIP) General Best Guidance for Immunization
Appendix 1: Glossary Adverse event. An undesirable medical condition that occurs following vaccination which might be truly caused by a vaccine, or it might be pure coincidence. Adverse reaction. An undesirable medical condition that has been demonstrated to be caused by a vaccine. Evidence for the causal relation is usually obtained through randomized clinical trials, controlled epidemiologic studies, isolation of the vaccine strain from the pathogenic site, or recurrence of the condition with repeated vaccination (i.e., rechallenge); synonyms include side effect and adverse effect. Adjuvant. A vaccine component distinct from the antigen that enhances the immune response to the antigen. Antitoxin. A solution of antibodies against a toxin. Antitoxin can be derived from either human (e.g., tetanus immune globulin) or animal (usually equine) sources (e.g., diphtheria and botulism antitoxin). Antitoxins are used to confer passive immunity and for treatment. Hyperimmune globulin (specific). Special preparations obtained from blood plasma from donor pools preselected for a high antibody content against a specific antigen (e.g., hepatitis B immune globulin, varicella-zoster immune globulin, rabies immune globulin, tetanus immune globulin, vaccinia immune globulin, cytomegalovirus immune globulin, botulism immune globulin). Immune globulin. A sterile solution containing antibodies, which are usually obtained from human blood. It is obtained by cold ethanol fractionation of large pools of blood plasma and contains 15%-18% protein. Intended for intramuscular administration, immune globulin is primarily indicated for routine maintenance of immunity among certain immunodeficient persons and for passive protection against measles and hepatitis A. General Best Practice Guidelines for Immunization: Appendix 1: Glossary 189 Immunobiologic. Antigenic substances (e.g., vaccines and toxoids) or antibody- containing preparations (e.g., globulins and antitoxins) from human or animal donors. -

2021 Medicare Vaccine Coverage Part B Vs Part D
CDPHP® Medicare Advantage Vaccine Coverage Guide Part B (Medical) vs. Part D (Pharmacy) Medicare Part B (Medical): Medicare Part D (Pharmacy): Vaccinations or inoculations Vaccinations or inoculations are included when the administration is (except influenza, pneumococcal, reasonable and necessary for the prevention of illness. and hepatitis B for members at risk) are excluded unless they are directly related to the treatment of an injury or direct exposure to a disease or condition. • Influenza Vaccine (Flu) • BCG Vaccine • Pneumococcal Vaccine • Diphtheria/Tetanus/Acellular Pertussis Vaccine (ADACEL, (Pneumovax, Prevnar 13) BOOSTRIX, DAPTACEL, INFANRIX) • Hepatitis B Vaccine • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus (Recombivax, Engerix-B) Vaccine (KINRIX, QUADRACEL) for members at moderate • Diphtheria/Tetanus Vaccine (DT, Td, TDVAX, TENIVAC) to high risk • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus Vac • Other vaccines when directly cine/ Haemophilus Influenzae Type B Conjugate Vaccine (PENTACEL) related to the treatment of an • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus injury or direct exposure to a Vaccine/Hepatitis B Vaccine (PEDIARIX) disease or condition, such as: • Haemophilus Influenzae Type B Conjugate Vaccine (ActHIB, PedvaxHIB, • Antivenom Sera Hiberix) • Diphtheria/Tetanus Vaccine • Hepatitis A Vaccine, Inactivated (VAQTA) (DT, Td, TDVAX, TENIVAC) • Hepatitis B Vaccine, Recombinant (ENGERIX-B, RECOMBIVAX HB) • Rabies Virus Vaccine for members at low risk (RabAvert, -

Global Immunization News 25 February 2011
Global Immunization News 25 February 2011 World Health Organization Global Immunization News Inside this issue: Technical Information Meeting of the Global Advisory 2 Committee on Vaccine Safety Polio eradication mourns loss of 2 NEW VACCINES, NEW true polio champion OPPORTUNITIES Announcements from The SIVAC 3 25/02/2011 from Hayatee Hasan, WHO/HQ Initiative In the past two months, four countries ― WHO position on pandemic influ- 3 Guyana, Kenya, Sierra Leone and Yemen ― enza vaccination following reports of narcolepsy subsequent to use of have introduced the pneumococcal conjugate Pandemrix vaccine. They represent the first of a series of countries introducing the vaccine in 2011. PHOTO Cold Chain and Logistics Taskforce 3 WHO concludes that quality issues 4 These introductions represent a major relating to Quinvaxem production milestone - the gap between access to new have been resolved vaccines between developed and developing AFRICA 4-6 countries is shortening; it is extraordinary to The launching of the Pneumococcal see a new vaccine launched in a developing conjugate vaccine (PCV-13) in Si- erra Leone country within one to two years of its introduction in the Americas and Europe, Kenya launches ten-valent pneumo- while in the past, it has taken several years coccal conjugate vaccine (PCV10) Vaccine carrier containing pneumococcal vaccine in (averaging 15 years) between the Kenya Meetings held in afro central introduction of new vaccines in developed and developing countries. AMERICAS 6-8 Peru introduces nationwide HPV vaccination; Argentina announces For more information regarding the launches in these countries, please see the articles on HPV vaccine introduction Kenya, Sierra Leone and Yemen. -

The Study of Thimerosal and Autism
The Study of Thimerosal and Autism Documentation and Codebook for the Child Vaccination Histories File: Cambridge, MA Lexington, MA Hadley, MA Bethesda, MD September 3, 2010 Chicago, IL Prepared for Frank DeStefano National Immunization Program Centers for Disease Control and Prevention Atlanta, GA 30329 Prepared by Cristofer Price Yeqin He Abt Associates Inc. Suite 800 North 4550 Montgomery Avenue Bethesda, MD 20814-3343 This documentation was prepared by Cristofer Price and Yeqin He of Abt Associates Inc. for the Immunization Safety Office (ISO) of the Centers for Disease Control and Prevention (CDC) Atlanta, GA 30333. Questions about the documentation, substantive questions, or technical issues regarding the data file should be directed to the CDC ISO, MS D26, 1600 Clifton Road, Atlanta, Georgia 30333 (404-639-8256). Suggested Citation for Study of Thimerosal and Autism Public Use Data Set: Price, C.S., He, Y. (2010) The Study of Thimerosal and Autism: Data Set Documentation. Bethesda MD: Abt Associates, Inc; Prepared for the National Immunization Program Centers for Disease Control and Prevention Atlanta, GA Abt Associates Inc. 1 Documentation and Codebook for the Child Vaccination Histories File 1. Introduction to the Child Vaccination Histories File............................................... 2 2. File Formats and Variable Descriptions................................................................... 4 1. Introduction to the Child Vaccination Histories File The Child Vaccination Histories File contains the data that were used to construct the measures of early childhood (postnatal) exposure to ethylmercury from thimerosal- containing vaccines and immune globulin preparations received by the study children during the age range spanning birth to 20 months. The Child Vaccination Histories File is provided with the public use data in order to make the calculation of exposure amounts transparent, and so that analysts have the potential to calculate alternative measures of exposure1.